Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health I
137 - Characterizing the Epidemiology of Bloodstream Infections among Hospitalized Neonates in Botswana: Are HIV-exposed neonates protected?
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 137
Publication Number: 137.111
Publication Number: 137.111
Carolyn M. McGann, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jonathan Strysko, Children's Hospital of Philadelphia, Gaborone, South-East, Botswana; One Bayani, University of Botswana, Gaborone, South-East, Botswana; Tefelo Thela, University of Manchester, Gaborone, South-East, Botswana; Ngwao Ngwako, University of Botswana Faculty of medicine, Bobonong, North-East, Botswana; Alemayehu M. Gezmu, POBox 70505, Gaborone, South-East, Botswana; Britt Nakstad, University of Botswana, Gaborone, Central, Botswana; Tonya Arscott-Mills, Levine Children's Hospital, Charlotte, NC, United States; Matthew S. Kelly, Duke University School of Medicine, Durham, NC, United States; Lauren Gianchetti, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Melissa Richard-Greenblatt, Public Health Ontario, Toronto, ON, Canada; Rebecca Luckett, Beth Israel Deaconess Medical Center, Boston, MA, United States; Justus Hofmeyr, University of Botswana, Gaborone, South-East, Botswana; Andrew P. Steenhoff, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Susan Coffin, Childrens' Hospital of Philadelphia, Philadelphia, PA, United States

Carolyn McGann, MD (she/her/hers)
Attending Neonatologist
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Although in-utero HIV exposure has been linked to higher infectious morbidity risk in infancy, some reports from sub-Saharan Africa describe lower sepsis risk among HIV-exposed (HE) neonates for unclear reasons. One proposed mechanism for this phenomenon is the use of prophylactic zidovudine, which has both anti-retroviral and bactericidal properties, and is given at birth to all HE neonates for first four weeks of life.
Objective: To describe the epidemiology and microbiology of bloodstream infections (BSIs) among hospitalized HE and HIV-unexposed (HU) neonates in Botswana, where approximately 20% of infants are born to a mother living with HIV with vertical transmission rates of < 1%.
Design/Methods: We enrolled a prospective cohort of neonates ≤96 hours old admitted to a tertiary care neonatal unit in Botswana from November 2020-December 2021, with intermittent pauses related to the COVID-19 pandemic. Data were collected by maternal interview and chart review. Patients were followed until death or discharge. Blood cultures (BACT/ALERT®, bioMérieux) were drawn at the discretion of the clinical team for suspicion of sepsis. BSI was defined as growth of a pathogen on blood culture, excluding likely contaminants, and divided into early-onset ( < 72 hours) or late-onset (>72 hours). Infant HIV infection was determined by HIV polymerase chain reaction (PCR) tests performed at 4-6 weeks of age in all HE infants.
Results: Of 479 neonates enrolled, 107 (23%) were HE. Fourteen had early-onset BSI, 5 of whom were HE. Of the 358 neonates still hospitalized at 72 hours, 82 (23%) were HE and 95 (27%) were evaluated for sepsis (Fig. 1). The incidence of late-onset BSI was 1.2% in HE compared to 5.8% in HU neonates, with a nearly 80% lower risk (RR 0.21, p=0.09). The risk of mortality and early-onset BSI were higher among HE neonates, and there was a slightly lower risk of Gram-negative compared to Gram-positive sepsis among HE, although results were not statistically significant (Table 1). Follow up is ongoing but of the 107 HE neonates, HIV PCR results were available for 42, all of which were negative.Conclusion(s): In this setting of high HIV prevalence, the influence of HIV exposure on BSI risk differed by onset age, but there was insufficient power to determine whether maternal HIV infection (or some other co-variate, such as zidovudine prophylaxis) was protective for late-onset-BSI. The lower incidence of late-onset BSI among HE neonates corroborates findings from other settings in sub-Saharan Africa. Future work will examine the association between maternal HIV status, maternal vaginal microbiome, and the evolving neonatal microbiome.
Figure 1. Study enrollment cohorts with frequencies of early- and late-onset bloodstream infection, by maternal HIV status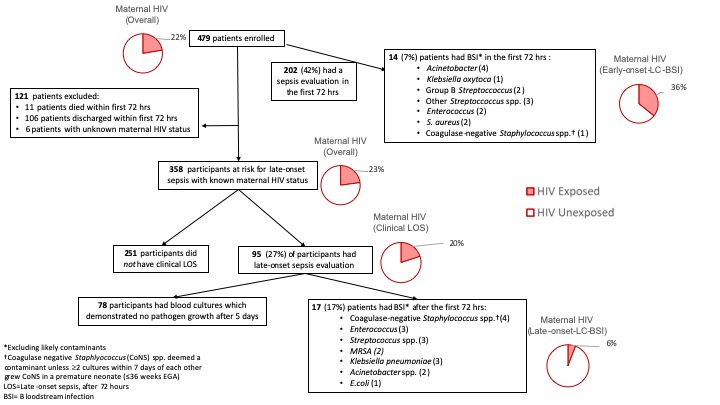
Table 1. Characteristics and outcomes of neonates and mothers, by maternal HIV status.jpg) BSI = Bloodstream infection
BSI = Bloodstream infection
EGA = Estimated gestational age
IQR = Interquartile range
VLBW = very low birthweight ( < 1,500g)
ELBW = extremely low birthweight ( < 1,000g)
RR = relative risk
Objective: To describe the epidemiology and microbiology of bloodstream infections (BSIs) among hospitalized HE and HIV-unexposed (HU) neonates in Botswana, where approximately 20% of infants are born to a mother living with HIV with vertical transmission rates of < 1%.
Design/Methods: We enrolled a prospective cohort of neonates ≤96 hours old admitted to a tertiary care neonatal unit in Botswana from November 2020-December 2021, with intermittent pauses related to the COVID-19 pandemic. Data were collected by maternal interview and chart review. Patients were followed until death or discharge. Blood cultures (BACT/ALERT®, bioMérieux) were drawn at the discretion of the clinical team for suspicion of sepsis. BSI was defined as growth of a pathogen on blood culture, excluding likely contaminants, and divided into early-onset ( < 72 hours) or late-onset (>72 hours). Infant HIV infection was determined by HIV polymerase chain reaction (PCR) tests performed at 4-6 weeks of age in all HE infants.
Results: Of 479 neonates enrolled, 107 (23%) were HE. Fourteen had early-onset BSI, 5 of whom were HE. Of the 358 neonates still hospitalized at 72 hours, 82 (23%) were HE and 95 (27%) were evaluated for sepsis (Fig. 1). The incidence of late-onset BSI was 1.2% in HE compared to 5.8% in HU neonates, with a nearly 80% lower risk (RR 0.21, p=0.09). The risk of mortality and early-onset BSI were higher among HE neonates, and there was a slightly lower risk of Gram-negative compared to Gram-positive sepsis among HE, although results were not statistically significant (Table 1). Follow up is ongoing but of the 107 HE neonates, HIV PCR results were available for 42, all of which were negative.Conclusion(s): In this setting of high HIV prevalence, the influence of HIV exposure on BSI risk differed by onset age, but there was insufficient power to determine whether maternal HIV infection (or some other co-variate, such as zidovudine prophylaxis) was protective for late-onset-BSI. The lower incidence of late-onset BSI among HE neonates corroborates findings from other settings in sub-Saharan Africa. Future work will examine the association between maternal HIV status, maternal vaginal microbiome, and the evolving neonatal microbiome.
Figure 1. Study enrollment cohorts with frequencies of early- and late-onset bloodstream infection, by maternal HIV status
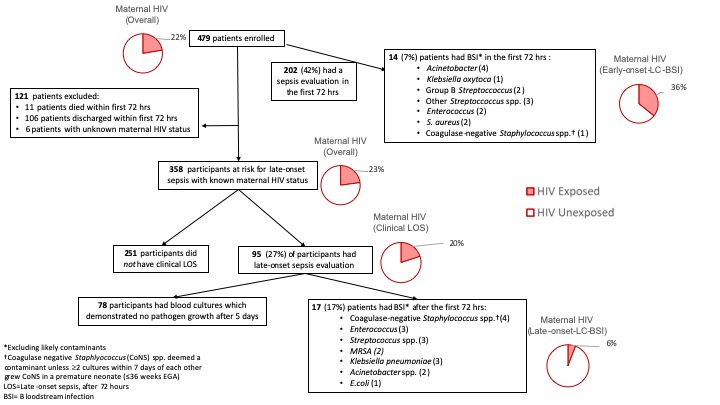
Table 1. Characteristics and outcomes of neonates and mothers, by maternal HIV status
.jpg) BSI = Bloodstream infection
BSI = Bloodstream infectionEGA = Estimated gestational age
IQR = Interquartile range
VLBW = very low birthweight ( < 1,500g)
ELBW = extremely low birthweight ( < 1,000g)
RR = relative risk
