Back
Medical Education: Medical Student
Category: Abstract Submission
Medical Education 1 - Medical Education: Medical Student
556 - Impact of a Pediatric Night Float on Medical Students’ Learning: Clerkship Student Perspectives
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 556
Publication Number: 556.115
Publication Number: 556.115
Barry Seltz, University of Colorado School of Medicine, Denver, CO, United States; Michael Edwards, University of Colorado School of Medicine, Denver, CO, United States; Kelsey Simek, University of Utah School of Medicine, Salt Lake City, UT, United States; Robert A. Levy, University of Washington School of Medicine, Seattle, WA, United States
Barry Seltz, MD
Pediatric Hospitalist
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: The structure and frequency of nighttime clinical experiences for medical students varies among clerkships. A night float model, in which learners work a series of successive inpatient overnight shifts, is increasingly common, yet few studies have examined its impact on students.
Objective: To explore 3rd year medical students’ perspectives on the impact on learning and wellness of a night float experience during their pediatric clerkship.
Design/Methods: Our qualitative study used grounded theory methods to interview 3rd year medical students who completed a night float experience between May 2019-December 2020 at an academic children’s hospital. The lens of situated learning informed the development of the interview guide. Four coders analyzed the data with the constant comparative method. Codes were built using an iterative approach and organized into categories describing themes. Discrepancies were resolved by consensus.
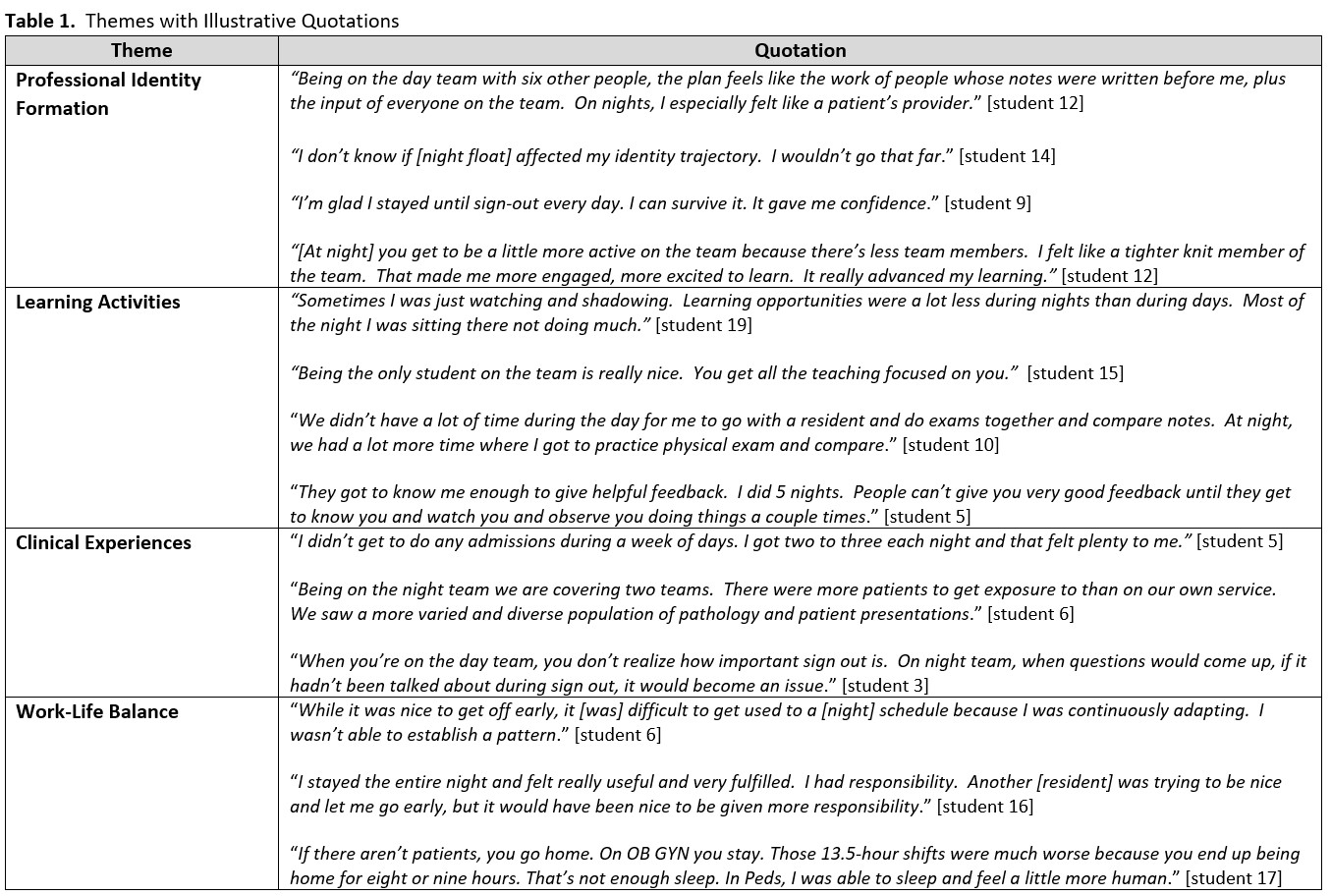
Results: Nineteen students participated in the study. Analysis yielded four themes: professional identity formation, learning activities, clinical experiences, and work-life balance. Quotes are shown in Table 1. Students described both high and low educational value of the night float. For students who felt like a member of the team and had a clear role, the night float experience promoted professional identity formation by providing opportunities to complete patient care tasks, justify clinical reasoning, increase confidence, and develop team camaraderie. However, not all students felt included in the team and this limited their learning. Students perceived the night float experience to be key residency preparation. Educational activities included experiential learning, teaching, receiving feedback, and self-directed learning. Students had more opportunities to admit and evaluate patients at night than on day shifts and were exposed to a greater diversity of patient illnesses. Fatigue was common with little time to do anything but sleep and work. Students were occasionally sent home early; this helped some, but not all, maintain a good quality of life but hampered their transition into a nighttime schedule.Conclusion(s): For students who felt like an integral member of the team, a night float was a valuable learning experience. Students also felt experiencing the night float was key preparation for residency. Evidence-based strategies to enhance integration of learners into the night team’s community of practice are needed.
Table 1. Illustrative Quotations.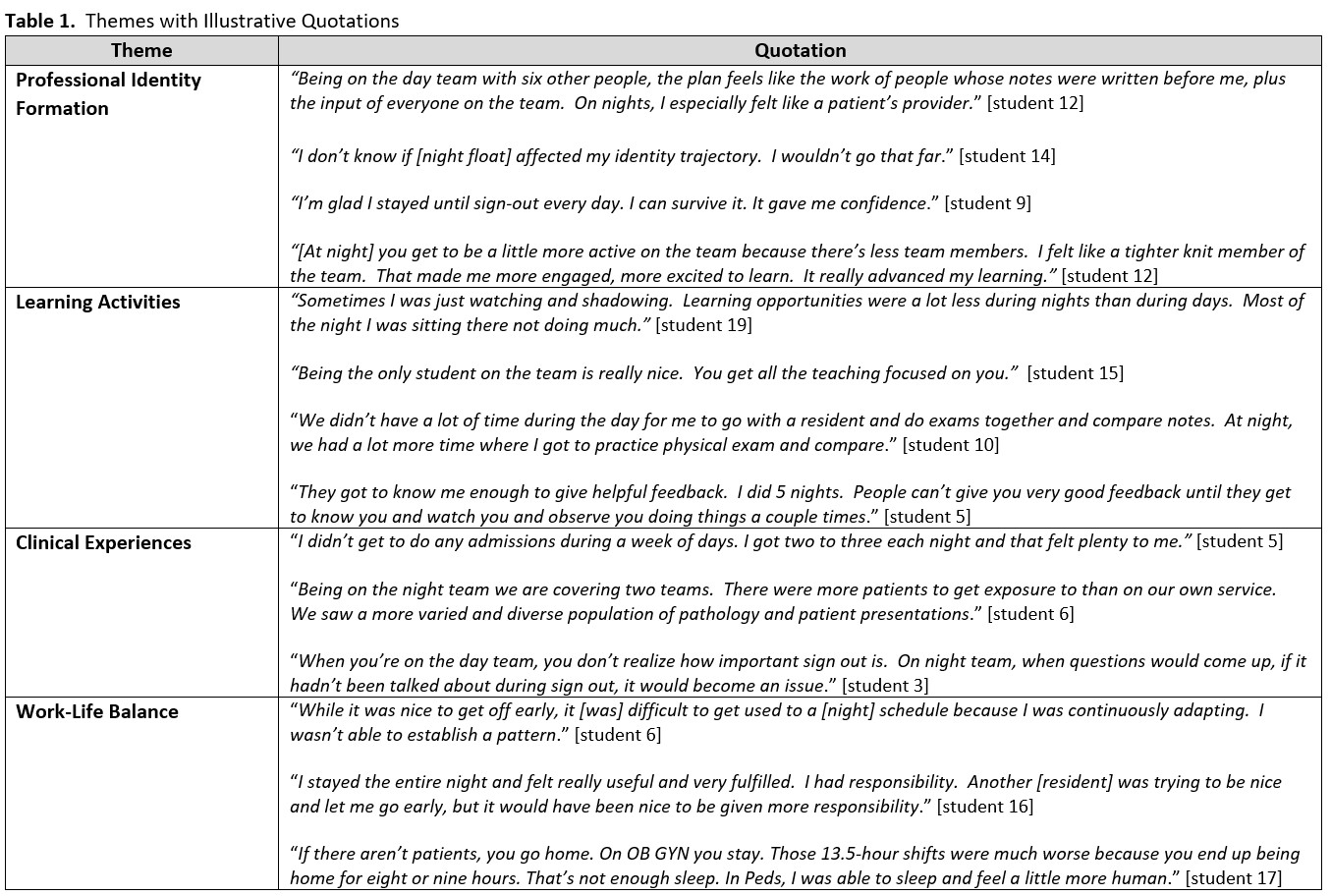
Objective: To explore 3rd year medical students’ perspectives on the impact on learning and wellness of a night float experience during their pediatric clerkship.
Design/Methods: Our qualitative study used grounded theory methods to interview 3rd year medical students who completed a night float experience between May 2019-December 2020 at an academic children’s hospital. The lens of situated learning informed the development of the interview guide. Four coders analyzed the data with the constant comparative method. Codes were built using an iterative approach and organized into categories describing themes. Discrepancies were resolved by consensus.
Results: Nineteen students participated in the study. Analysis yielded four themes: professional identity formation, learning activities, clinical experiences, and work-life balance. Quotes are shown in Table 1. Students described both high and low educational value of the night float. For students who felt like a member of the team and had a clear role, the night float experience promoted professional identity formation by providing opportunities to complete patient care tasks, justify clinical reasoning, increase confidence, and develop team camaraderie. However, not all students felt included in the team and this limited their learning. Students perceived the night float experience to be key residency preparation. Educational activities included experiential learning, teaching, receiving feedback, and self-directed learning. Students had more opportunities to admit and evaluate patients at night than on day shifts and were exposed to a greater diversity of patient illnesses. Fatigue was common with little time to do anything but sleep and work. Students were occasionally sent home early; this helped some, but not all, maintain a good quality of life but hampered their transition into a nighttime schedule.Conclusion(s): For students who felt like an integral member of the team, a night float was a valuable learning experience. Students also felt experiencing the night float was key preparation for residency. Evidence-based strategies to enhance integration of learners into the night team’s community of practice are needed.
Table 1. Illustrative Quotations.