Back
Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health I
141 - Implementation of a Trauma Registry for Pediatric Injury Patients in Northern Tanzania
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 141
Publication Number: 141.111
Publication Number: 141.111
Elizabeth M. Keating, University of Utah, Salt Lake City, UT, United States; Melissa H. Watt, University of Utah School of Medicine, Salt Lake City, UT, United States; Francis Sakita, Kilimanjaro Christian Medical University College, Moshi, Kilimanjaro, Tanzania; Blandina T. Mmbaga, Kilimanjaro Christian Medical University College, Kilimanjaro, Kilimanjaro, Tanzania; Getrude M. Nkini, KCMC-DUKE COLLABORATION, Moshi, Kilimanjaro, Tanzania; Ismail Amiri, KCMC-DUKE COLLABORATION, Kilimanjaro, Kilimanjaro, Tanzania; Chermiqua Tsosie, Arizona State University, Phoenix, AZ, United States; NORA F. FINO, University of Utah, Salt Lake City, UT, United States; Catherine A. Staton, Duke University School of Medicine, Durham, NC, United States
- EK
Elizabeth M. Keating, MD, MSPH (she/her/hers)
Assistant Professor
University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Pediatric injuries in low- and middle-income countries are a leading cause of morbidity and mortality worldwide. Implementing hospital-based trauma registries can reduce the knowledge gap in both hospital care and patient outcomes and lead to quality improvement initiatives.
Objective: The goal of this study was to create a pediatric trauma registry at a large tertiary referral hospital in Northern Tanzania to provide insight into the epidemiology, outcomes, and factors associated with poor outcomes in injured children.
Design/Methods: This was a prospective observational study in which a pediatric trauma registry was implemented at a large tertiary referral hospital in Northern Tanzania. Data included demographics, hospital-based care, and outcomes including morbidity and mortality. Morbidity was measured by the Pediatric Glasgow Outcome Score-Extended (GOS-E) score and the Patient Specific Functional Scale (PSFS). Data were input into REDCap© and analyzed using ANOVA and Chi-squared tests in SAS(Version 9.4)©.
Results: 365 patients were enrolled in the registry from November 2020 to October 2021. The majority were males (n=240, 65.8%). Most were children 0-5 years (41.7%, n=152), 34.5% (n=126) were 6-11 years, and 23.8% (n=87) were 12-17 years. The leading causes of pediatric injuries were falls (n=137, 37.5%) and road traffic injuries (n=125, 34.5%). The mortality rate was 8.2% (n=27). Of the in-hospital deaths, 43.3% were children with burn injuries who also had a higher odds of mortality than children with other injuries (OR 8.72, p < 0.001). The factors associated with in-hospital mortality and morbidity were vital sign abnormalities, burn severity, abnormal GCS score, and ICU admission.Conclusion(s): The mortality rate of injured children in our cohort was high, especially in children with burn injuries. In order to reduce morbidity and mortality, interventions should be prioritized that focus on pediatric injured patients that present with abnormal vital signs, altered mental status, and severe burns. These findings highlight the need for health system capacity building to improve outcomes of pediatric injury patients in Northern Tanzania, especially in those with burn injuries.
Figure 1. Bar Plot of Primary Injuries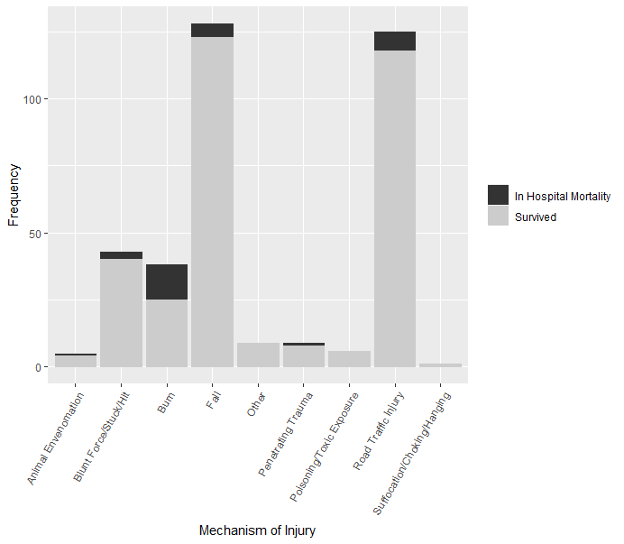 Bar plot of primary mechanisms of injury for pediatric injury patients with bars proportional to percentage of patients who survived and died.
Bar plot of primary mechanisms of injury for pediatric injury patients with bars proportional to percentage of patients who survived and died.
Objective: The goal of this study was to create a pediatric trauma registry at a large tertiary referral hospital in Northern Tanzania to provide insight into the epidemiology, outcomes, and factors associated with poor outcomes in injured children.
Design/Methods: This was a prospective observational study in which a pediatric trauma registry was implemented at a large tertiary referral hospital in Northern Tanzania. Data included demographics, hospital-based care, and outcomes including morbidity and mortality. Morbidity was measured by the Pediatric Glasgow Outcome Score-Extended (GOS-E) score and the Patient Specific Functional Scale (PSFS). Data were input into REDCap© and analyzed using ANOVA and Chi-squared tests in SAS(Version 9.4)©.
Results: 365 patients were enrolled in the registry from November 2020 to October 2021. The majority were males (n=240, 65.8%). Most were children 0-5 years (41.7%, n=152), 34.5% (n=126) were 6-11 years, and 23.8% (n=87) were 12-17 years. The leading causes of pediatric injuries were falls (n=137, 37.5%) and road traffic injuries (n=125, 34.5%). The mortality rate was 8.2% (n=27). Of the in-hospital deaths, 43.3% were children with burn injuries who also had a higher odds of mortality than children with other injuries (OR 8.72, p < 0.001). The factors associated with in-hospital mortality and morbidity were vital sign abnormalities, burn severity, abnormal GCS score, and ICU admission.Conclusion(s): The mortality rate of injured children in our cohort was high, especially in children with burn injuries. In order to reduce morbidity and mortality, interventions should be prioritized that focus on pediatric injured patients that present with abnormal vital signs, altered mental status, and severe burns. These findings highlight the need for health system capacity building to improve outcomes of pediatric injury patients in Northern Tanzania, especially in those with burn injuries.
Figure 1. Bar Plot of Primary Injuries
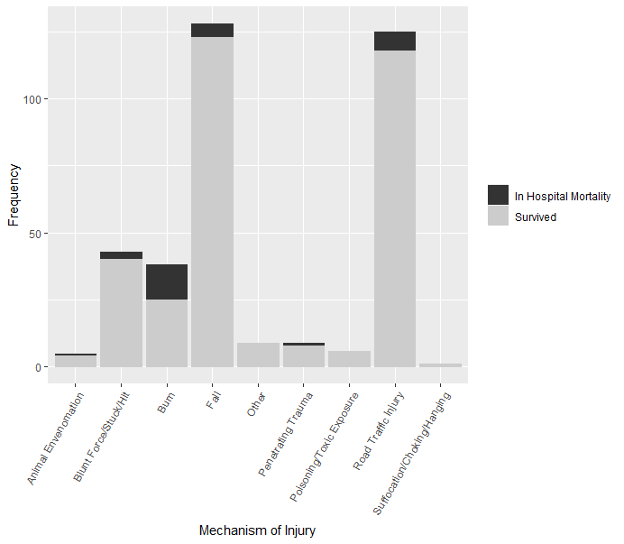 Bar plot of primary mechanisms of injury for pediatric injury patients with bars proportional to percentage of patients who survived and died.
Bar plot of primary mechanisms of injury for pediatric injury patients with bars proportional to percentage of patients who survived and died.