Back
Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement III: GI and Nutrition
236 - Improving Enteral Feeding Practices and Human Milk Consumption In Multiple NICUS: A Quality Improvement Project
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 236
Publication Number: 236.128
Publication Number: 236.128
Navin Bhopal, Phoenix Children's Hospital, Phoenix, AZ, United States; Lara Ulm, Phoenix Children's Hospital, Scottsdale, AZ, United States; Deborah Tom, Phoenix Children's Hospital, Phoenix, AZ, United States; Sheralyn K. Kaprolet, Phoenix Children's Hospital, Chandler, AZ, United States; Jade Parker, University of Arizona College of Medicine - Phoenix, Glendale, AZ, United States; Megan Shea, Phoenix Children's Hospital, Phoenix, AZ, United States; Cheryl Wieweck, Phoenix Children's Hospital, Gilbert, AZ, United States; Shelley A. Akey, Phoenx Children’s Hospital, Phoenix, AZ, United States; Jessica Wickland, Phoenix Children's Hospital, Phoenix, AZ, United States; Whitney Ruben, Phoenix Children's Hospital, Phoenix, AZ, United States; Oleksandr Kudin, Phoenix Children's Hospital, Phoenix, AZ, United States; Jennifer Weber, University of Arizona College of Medicine - Phoenix, Phoenix, AZ, United States; Marc Ellsworth, Phoenix Children's Hospital, Gilbert, AZ, United States; Kevin R. Ellsworth, Phoenix Children's Hospital, Gilbert, AZ, United States; Pamela Griffiths, Phoenix Children's Hospital, Phoenix, AZ, United States; Kimberlee A. Allred, Phoenix Children's Hospital, Phoenix, AZ, United States; Katherine Marshall, Phoenix Children's Hospital, Scottsdale, AZ, United States; Nanette Whittington, Phoenix Children’s Hospital, Queen Creek, AZ, United States; Nicole Lattanzio, Phoenix Children's Hospital, Phoenix, AZ, United States; Mohammed Elkhwad, Phoenix Children's Hospital, Phoenix, AZ, United States; Gregg Martin, Phoenix Children's Hospital, Cave Creek, AZ, United States
Navin Bhopal, MD
Neonatologist
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Optimal nutrition is essential to overcome common disease processes in preterm and high-risk term newborns. Introduction of enteral feedings creates a possible risk of developing necrotizing enterocolitis (NEC). NEC is a potentially devastating inflammatory disease of the gastrointestinal tract, which may lead to intestinal perforation and death. Simple interventions such as prioritizing human milk over formula feeds and following a standardized feeding protocol are well established practices for improving outcomes and reducing NEC.
Objective: The Phoenix Children’s Hospital Division of Neonatology was established in 2020, providing medical services to a level 4 NICU and to two level 2 NICUs. We introduced a standardized feeding protocol and used quality improvement methodology to measure compliance in non-surgical infants < 37 weeks, with a goal to increase compliance by > 10% over a 1 year period. Secondarily, we also measured human milk use during hospitalization and at discharge in infants of all gestational ages with a goal to increase human milk consumption by >10% over the same time period.
Design/Methods: We collected data on our feeding practices at all 3 NICUs to measure compliance with the feeding protocol from December 2020 to December 2021. Outcomes were compared in 3 distinct epochs: Epoch 1 from December 2020 to March 2021, epoch 2 from April to July 2021 and epoch 3 from August to December 2021. To increase compliance with our feeding protocol, we educated providers and nursing staff. Awareness was increased by posting copies at work stations and in bedside charts (February to May 2021). Interim quality metrics were reviewed periodically with the medical team.
Results: Feeding data was tracked on 355 infants. The mean gestational age and birth weight were 33 weeks +/- 2.7 weeks and 2120g +/- 769g. The mean time to full feeds was 4.4 days +/- 2.8 days. Compliance with protocol improved with time from 72% in epoch 1 to 88% in epoch 3 in babies < 37 weeks. Maternal breast milk use for initiating feeds increased from 40% to 45% from epoch 1 to 3. Babies discharging home exclusively on breast milk remained relatively stable over time at 16% in epoch 1 and 17% in epoch 3. There were 2 cases of medical NEC and no cases of surgical NEC.Conclusion(s): In this QI project, we improved compliance with a feeding protocol and increased in-hospital human milk usage in infants < 37 weeks. Exclusive human milk diets were not sustained through hospital discharge and remained stable at 15-17%. There were 2 cases of medical NEC and no cases of surgical NEC over the course of the year.
Feeding Protocol Compliance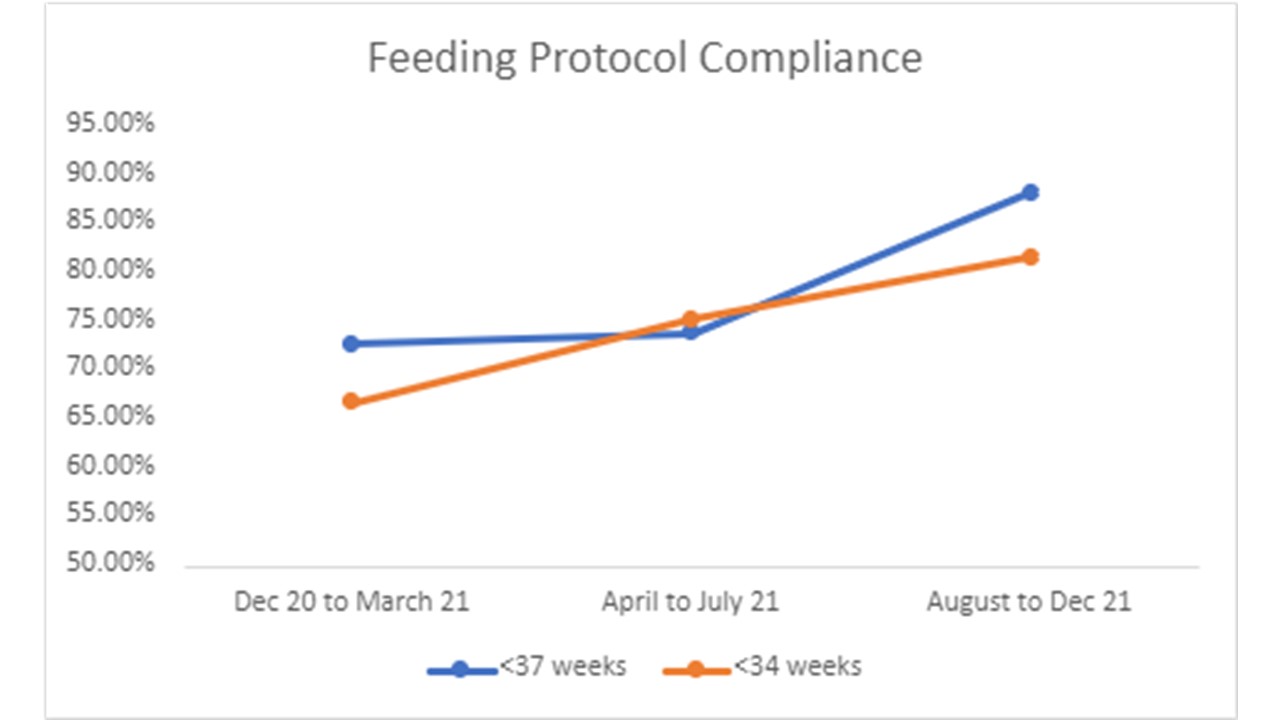 Compliance with following the neonatal feeding protocol improved over time in infants < 37 weeks from 72% to 88% (blue) and in infants < 34 weeks from 66% to 81% (orange)
Compliance with following the neonatal feeding protocol improved over time in infants < 37 weeks from 72% to 88% (blue) and in infants < 34 weeks from 66% to 81% (orange)
Initiation of feeds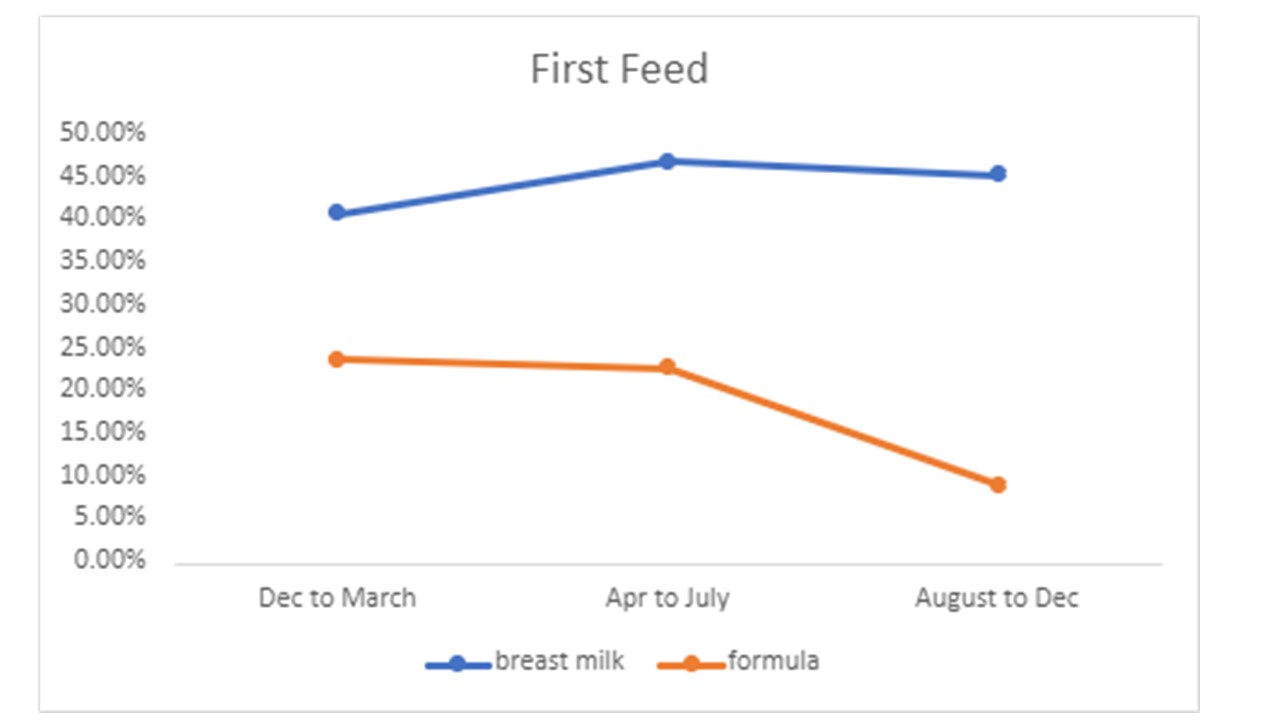 Maternal milk use improved from 40 to 45% for the first enteral feed (blue), while formula use declined from 23% to 11% (orange)
Maternal milk use improved from 40 to 45% for the first enteral feed (blue), while formula use declined from 23% to 11% (orange)
Objective: The Phoenix Children’s Hospital Division of Neonatology was established in 2020, providing medical services to a level 4 NICU and to two level 2 NICUs. We introduced a standardized feeding protocol and used quality improvement methodology to measure compliance in non-surgical infants < 37 weeks, with a goal to increase compliance by > 10% over a 1 year period. Secondarily, we also measured human milk use during hospitalization and at discharge in infants of all gestational ages with a goal to increase human milk consumption by >10% over the same time period.
Design/Methods: We collected data on our feeding practices at all 3 NICUs to measure compliance with the feeding protocol from December 2020 to December 2021. Outcomes were compared in 3 distinct epochs: Epoch 1 from December 2020 to March 2021, epoch 2 from April to July 2021 and epoch 3 from August to December 2021. To increase compliance with our feeding protocol, we educated providers and nursing staff. Awareness was increased by posting copies at work stations and in bedside charts (February to May 2021). Interim quality metrics were reviewed periodically with the medical team.
Results: Feeding data was tracked on 355 infants. The mean gestational age and birth weight were 33 weeks +/- 2.7 weeks and 2120g +/- 769g. The mean time to full feeds was 4.4 days +/- 2.8 days. Compliance with protocol improved with time from 72% in epoch 1 to 88% in epoch 3 in babies < 37 weeks. Maternal breast milk use for initiating feeds increased from 40% to 45% from epoch 1 to 3. Babies discharging home exclusively on breast milk remained relatively stable over time at 16% in epoch 1 and 17% in epoch 3. There were 2 cases of medical NEC and no cases of surgical NEC.Conclusion(s): In this QI project, we improved compliance with a feeding protocol and increased in-hospital human milk usage in infants < 37 weeks. Exclusive human milk diets were not sustained through hospital discharge and remained stable at 15-17%. There were 2 cases of medical NEC and no cases of surgical NEC over the course of the year.
Feeding Protocol Compliance
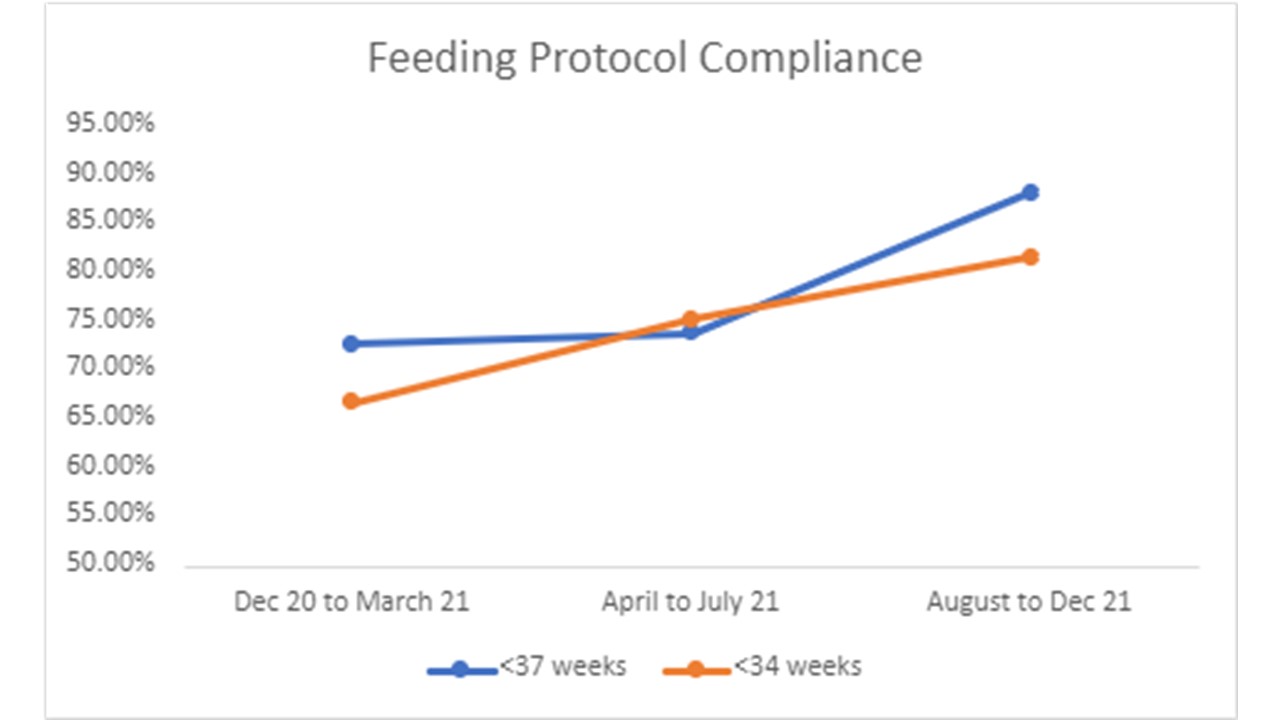 Compliance with following the neonatal feeding protocol improved over time in infants < 37 weeks from 72% to 88% (blue) and in infants < 34 weeks from 66% to 81% (orange)
Compliance with following the neonatal feeding protocol improved over time in infants < 37 weeks from 72% to 88% (blue) and in infants < 34 weeks from 66% to 81% (orange)Initiation of feeds
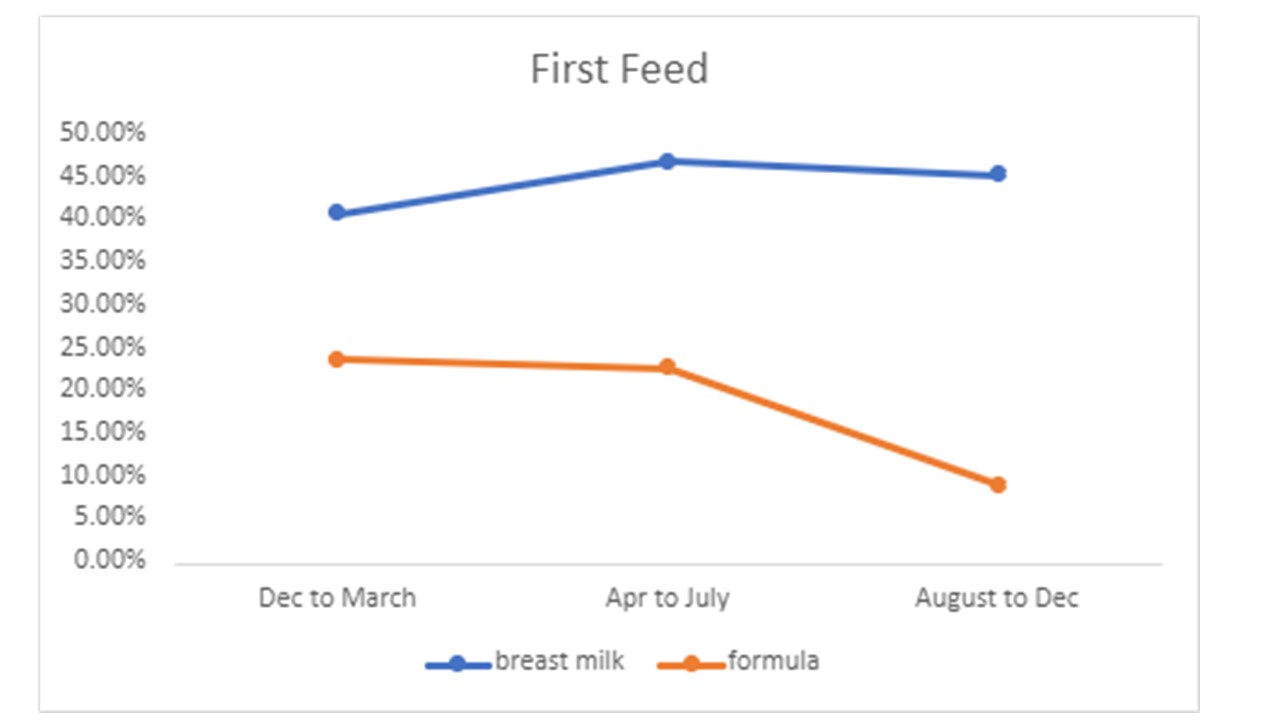 Maternal milk use improved from 40 to 45% for the first enteral feed (blue), while formula use declined from 23% to 11% (orange)
Maternal milk use improved from 40 to 45% for the first enteral feed (blue), while formula use declined from 23% to 11% (orange)