Neonatal General
Category: Abstract Submission
Neonatology General 5
408 - Mortality in Very Low Birth Weight Infants During Initial Hospital Stay: Effect of Maternal Age
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 408
Publication Number: 408.135
Publication Number: 408.135
Nisha Patil, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States; Sandeep k. chilakala, University of Tennessee Health Science Center College of Medicine, Germantown, TN, United States; Ramasubbareddy Dhanireddy, University of Tennessee Health Science Center College of Medicine, Memphiis, TN, United States

Nisha Patil
Student
University of Tennessee Health Science Center College of Medicine
Memphis, Tennessee, United States
Presenting Author(s)
Background: Adolescent and advanced maternal age (Under 19 and over 35 years) are associated with higher rates of preterm birth and increased risk of neonatal morbidity and mortality. Impact of maternal age at birth and risk of neonatal mortality has been studied. Factors including quality of prenatal care, antenatal steroids, quality of neonatal care influence the outcomes in very low birth weight (VLBW) infants. It is not clear whether there is any maternal age effect on mortality in VLBW infants who are already at highest risk for adverse outcomes
Objective: To identify whether maternal age independently contributed to adverse outcomes and mortality in VLBW infants
Design/Methods: 1353 VLBW infants born at Regional One Health from Jan 2012 to Dec 2019 were included. Infants died in delivery room were excluded. Maternal and neonatal demographics, and clinical data were collected. Risk factors associated with in-hospital neonatal mortality (INMR) were compared. Chi- squared test was used to compare categorical variables and the unpaired t- test to compare the compare continuous variables. Multivariate logistic regression was performed to adjust for the clinically significant univariates on INMR. Additionally, polynomial regression was used to analyze the association between maternal age and risk of INMR
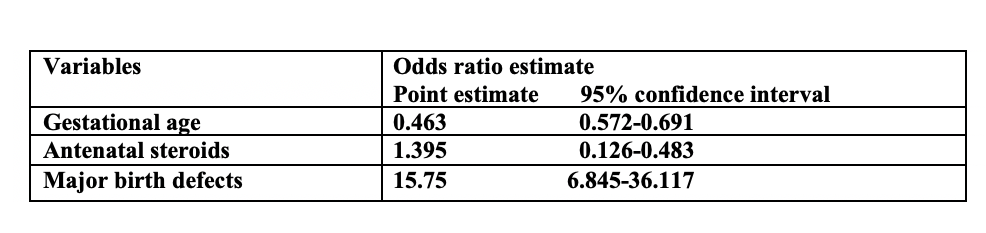
Results: Variables associated with significantly increased risk of mortality include, decreased exposure to antenatal corticosteroids, vaginal delivery, major birth defects, lower five-minute Apgar score, male gender, lower gestational age, and lower birth weight. (Table 1)Multivariate logistic regression of all the significant variables (Table 2) showed that lower gestational age [odds ratio of 0.463 with 95% CI (0.572-0.69)], absence of antenatal steroids [ odds ratio of 1.395 with 95%CI (0.126-0.483)], and presence of major birth defects [odds ratio of 15.75 with 95% CI (6.845-36.117)] significantly influence mortality. A polynomial fit regression (Graph 1) with maternal age as a continuous variable suggests 28 years of age with the lowest risk (3.2%) of INMR (r= 0.4989, p < 0.05). Maternal age groups on either side of 28 years have increased risk of INMR.Conclusion(s): Younger and older maternal ages are correlated with increased mortality in even in VLBW infants. Our analysis points to an interesting observation that maternal age of 28 years corresponds to the lowest risk of INMR in VLBW infants. Clinical factors which influence mortality in VLBW infants are driven by maternal age and are severe in extremes of maternal age
Table 1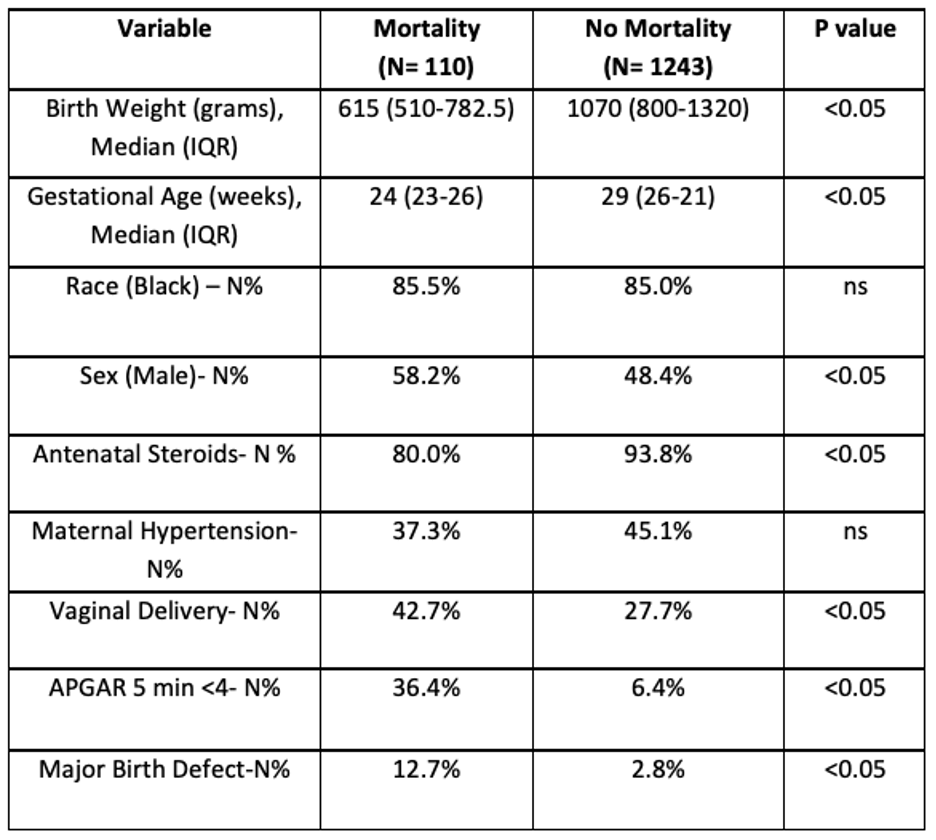
Table 2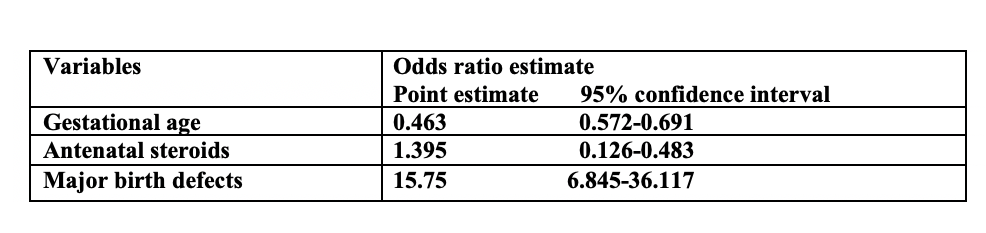
Objective: To identify whether maternal age independently contributed to adverse outcomes and mortality in VLBW infants
Design/Methods: 1353 VLBW infants born at Regional One Health from Jan 2012 to Dec 2019 were included. Infants died in delivery room were excluded. Maternal and neonatal demographics, and clinical data were collected. Risk factors associated with in-hospital neonatal mortality (INMR) were compared. Chi- squared test was used to compare categorical variables and the unpaired t- test to compare the compare continuous variables. Multivariate logistic regression was performed to adjust for the clinically significant univariates on INMR. Additionally, polynomial regression was used to analyze the association between maternal age and risk of INMR
Results: Variables associated with significantly increased risk of mortality include, decreased exposure to antenatal corticosteroids, vaginal delivery, major birth defects, lower five-minute Apgar score, male gender, lower gestational age, and lower birth weight. (Table 1)Multivariate logistic regression of all the significant variables (Table 2) showed that lower gestational age [odds ratio of 0.463 with 95% CI (0.572-0.69)], absence of antenatal steroids [ odds ratio of 1.395 with 95%CI (0.126-0.483)], and presence of major birth defects [odds ratio of 15.75 with 95% CI (6.845-36.117)] significantly influence mortality. A polynomial fit regression (Graph 1) with maternal age as a continuous variable suggests 28 years of age with the lowest risk (3.2%) of INMR (r= 0.4989, p < 0.05). Maternal age groups on either side of 28 years have increased risk of INMR.Conclusion(s): Younger and older maternal ages are correlated with increased mortality in even in VLBW infants. Our analysis points to an interesting observation that maternal age of 28 years corresponds to the lowest risk of INMR in VLBW infants. Clinical factors which influence mortality in VLBW infants are driven by maternal age and are severe in extremes of maternal age
Table 1
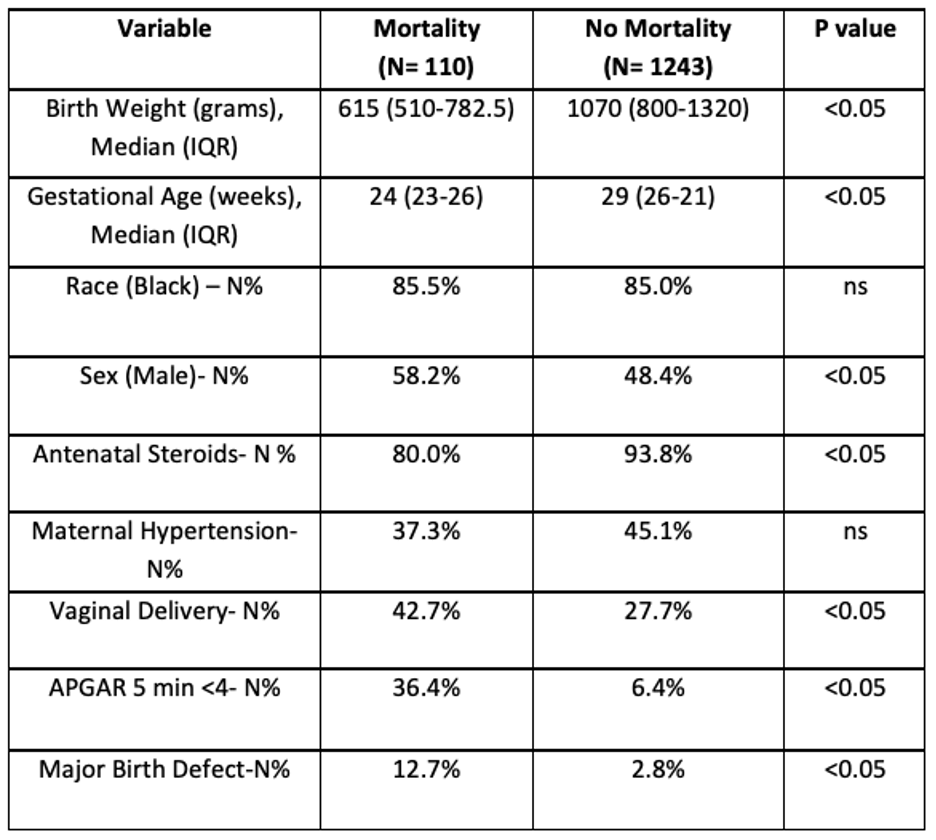
Table 2