Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up I
452 - Neurodevelopmental and Behavioral Outcomes at Two Years’ Corrected Age of Very Preterm Infants following a Post Discharge Responsive Parenting Program (TOP program).
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 452
Publication Number: 452.121
Publication Number: 452.121
Nienke M. Halbmeijer, Emma Children's Hospital, Amsterdam UMC, 'S-GRAVENHAGE, Zuid-Holland, Netherlands; Martine jeukens-Visser, Amsterdam UMC, Amsterdam, Noord-Holland, Netherlands; Wes Onland, Emma Children's Hospital Amsterdam UMC, Amsterdam, Noord-Holland, Netherlands; Anton van Kaam, Emma Children's Hospitial, Amsterdam UMC, Amsterdam, Noord-Holland, Netherlands; Aleid Leemhuis, amsterdam UMC, Amsterdam, Noord-Holland, Netherlands

Nienke M. Halbmeijer, MD
Research Fellow
Emma Children's Hospital, Amsterdam UMC
'S-GRAVENHAGE, Zuid-Holland, Netherlands
Presenting Author(s)
Background: Post-discharge responsive parenting programs have shown to improve neurodevelopmental outcomes in very preterm infants, but are rarely part of routine care. In 2010, a development and implementation process of the TOP program (Transmural developmental support for very preterm infants and their parents) was set up after a randomized study have shown a positive effect on neurodevelopment. Since 2014 it is part of routine care. The placebo controlled SToP-BPD (Systemic Hydrocortisone To Prevent Bronchopulmonary Dysplasia in preterm infants) study recruited patients from 2011 to 2016 and included very preterm infants with high risk for adverse neurodevelopmental outcomes.
Objective: The aim of this study was to evaluate the outcomes of the TOP program during its implementation process within the SToP-BPD cohort.
Design/Methods: The TOP program starts after discharge home and consisted after 2014 of 12 home visits, until one year corrected age (CA). Neurodevelopmental and behavioral outcomes of infants who were supported by the TOP program were compared to those who were not supported. At two years’ CA, infants were evaluated with the Dutch Bayley Scales of Infant Development, third edition yielding a composite cognitive and motor score (CCS and CMS) and the Child Behavior Check List (CBCL1½ -5) according to the STOP-BPD protocol. Multiple imputation was used to account for missing data of the CBCL1½ -5.
Results: Among 262 infants who survived till two years’ CA (mean gestational age 25.8 (±1.3) weeks), 93 infants (35%) had received the TOP program during the implementation process (mean home visits 10.7 (range 2 to 13)). Background characteristics were similar between both groups. Infants in the TOP group had a significant higher mean CCS (96.7 (± 13.8), compared to the non-TOP group (92.0 (± 17.5); mean difference 4.7 [95% CI 0.3 to 9.2], p=0.04), with also a significant lower incidence of a CCS < 85 (20.3% vs. 35.2%; risk difference -14.9 [95% CI -27.2 to -2.6], p=0.03). No significant differences were found on CMS. For behavior problems, a significantly lower T-score for anxious/depressive problems was found in the TOP group (50.5 vs. 51.2; mean difference -0.72 [95% CI -1.37 to -0.08], p=0.03).Conclusion(s): At two years’ CA, one year after the TOP intervention program ends, very preterm infants supported in the TOP program had better cognitive function and less anxious/depressive problems. This finding confirms its positive effect, now outside the setting of a randomized trial.
Table 1. Neurodevelopmental and behavioral outcomes at 2 years’ corrected age.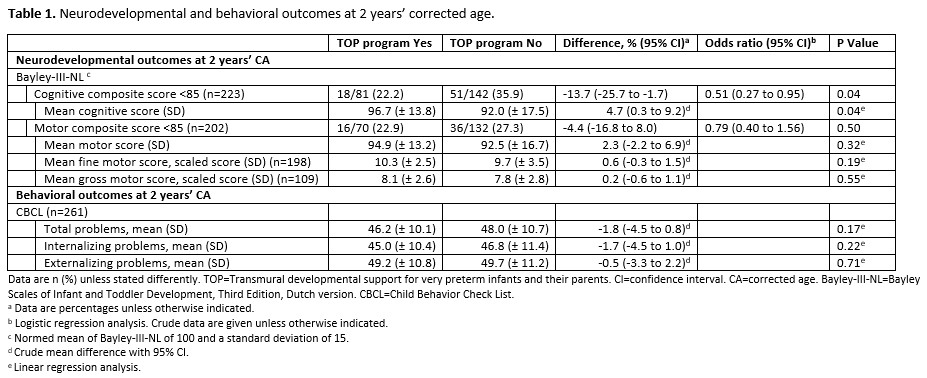 Data are n (%) unless stated differently. TOP=Transmural developmental support for very preterm infants and their parents. CI=confidence interval. CA=corrected age. Bayley-III-NL=Bayley Scales of Infant and Toddler Development, Third Edition, Dutch version. CBCL=Child Behavior Check List.
Data are n (%) unless stated differently. TOP=Transmural developmental support for very preterm infants and their parents. CI=confidence interval. CA=corrected age. Bayley-III-NL=Bayley Scales of Infant and Toddler Development, Third Edition, Dutch version. CBCL=Child Behavior Check List.
a Data are percentages unless otherwise indicated.
b Logistic regression analysis. Crude data are given unless otherwise indicated.
c Normed mean of Bayley-III-NL of 100 and a standard deviation of 15.
d Crude mean difference with 95% CI.
e Linear regression analysis.
Objective: The aim of this study was to evaluate the outcomes of the TOP program during its implementation process within the SToP-BPD cohort.
Design/Methods: The TOP program starts after discharge home and consisted after 2014 of 12 home visits, until one year corrected age (CA). Neurodevelopmental and behavioral outcomes of infants who were supported by the TOP program were compared to those who were not supported. At two years’ CA, infants were evaluated with the Dutch Bayley Scales of Infant Development, third edition yielding a composite cognitive and motor score (CCS and CMS) and the Child Behavior Check List (CBCL1½ -5) according to the STOP-BPD protocol. Multiple imputation was used to account for missing data of the CBCL1½ -5.
Results: Among 262 infants who survived till two years’ CA (mean gestational age 25.8 (±1.3) weeks), 93 infants (35%) had received the TOP program during the implementation process (mean home visits 10.7 (range 2 to 13)). Background characteristics were similar between both groups. Infants in the TOP group had a significant higher mean CCS (96.7 (± 13.8), compared to the non-TOP group (92.0 (± 17.5); mean difference 4.7 [95% CI 0.3 to 9.2], p=0.04), with also a significant lower incidence of a CCS < 85 (20.3% vs. 35.2%; risk difference -14.9 [95% CI -27.2 to -2.6], p=0.03). No significant differences were found on CMS. For behavior problems, a significantly lower T-score for anxious/depressive problems was found in the TOP group (50.5 vs. 51.2; mean difference -0.72 [95% CI -1.37 to -0.08], p=0.03).Conclusion(s): At two years’ CA, one year after the TOP intervention program ends, very preterm infants supported in the TOP program had better cognitive function and less anxious/depressive problems. This finding confirms its positive effect, now outside the setting of a randomized trial.
Table 1. Neurodevelopmental and behavioral outcomes at 2 years’ corrected age.
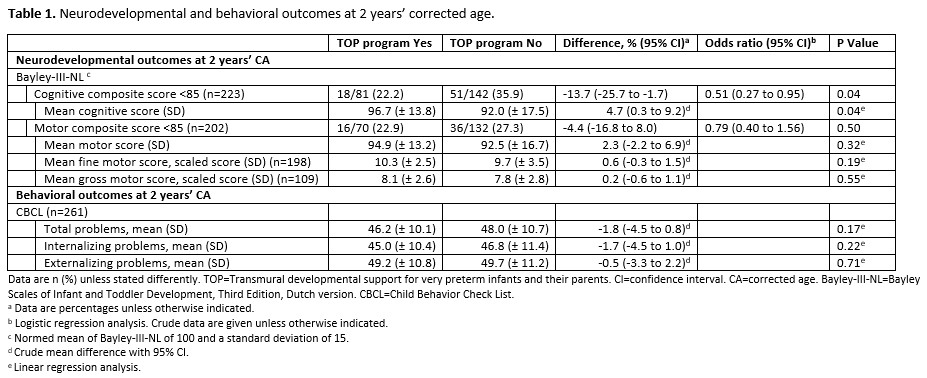 Data are n (%) unless stated differently. TOP=Transmural developmental support for very preterm infants and their parents. CI=confidence interval. CA=corrected age. Bayley-III-NL=Bayley Scales of Infant and Toddler Development, Third Edition, Dutch version. CBCL=Child Behavior Check List.
Data are n (%) unless stated differently. TOP=Transmural developmental support for very preterm infants and their parents. CI=confidence interval. CA=corrected age. Bayley-III-NL=Bayley Scales of Infant and Toddler Development, Third Edition, Dutch version. CBCL=Child Behavior Check List.a Data are percentages unless otherwise indicated.
b Logistic regression analysis. Crude data are given unless otherwise indicated.
c Normed mean of Bayley-III-NL of 100 and a standard deviation of 15.
d Crude mean difference with 95% CI.
e Linear regression analysis.
