Medical Education: Resident
Category: Abstract Submission
Medical Education 2 - Medical Education: Resident I - Hot Topics
573 - Pediatric Resident Burnout and its Relation to the Neuroendocrine System
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 573
Publication Number: 573.116
Publication Number: 573.116
Daniel S. Tawfik, Stanford University School of Medicine, Palo Alto, CA, United States; Cynthia R. Rovnaghi, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States; Timothy Cornell, Stanford University, Palo Alto, CA, United States; Jochen Profit, Stanford University, Palo Alto, CA, United States; Kanwaljeet S. Anand, Stanford University School of Medicine, Stanford, CA, United States

Daniel Tawfik, MD, MS
Instructor
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background: Burnout is common, particularly among residency training, with adverse consequences for quality of care and patient outcomes. Measuring burnout relies on infrequent and subjective surveys, resulting in an inability to identify the underlying factors or biological mechanisms that promote or prevent professional burnout. Cortisol is released with physiologic responses to stress, whereas oxytocin results from social bonding experiences. Burnout status correlates with cortisol release and dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, but the precise chronology and mechanisms of this relationship are unknown. Objective quantification of physician burnout using biomarkers such as cortisol and oxytocin could assist both in identifying the key drivers of physician burnout and in evaluating the counter-measures to burnout.
Objective: Pilot study to determine feasibility and quantify longitudinal pediatric resident burnout in relation to hair cortisol and hair oxytocin concentrations.
Design/Methods: Longitudinal observational cohort study of pediatric residents that assessed burnout using the Stanford Professional Fulfillment Index, hair cortisol and hair oxytocin at 3-month intervals from January 2020-January 2021. We evaluated test-retest reliability, sensitivity to change using Pearson product-moment correlations, and relationships between burnout and hair biomarkers using hierarchical mixed-effects linear regressions.
Results: We evaluated 17 Pediatrics residents with 78 wellness surveys and 54 hair samples. Burnout symptoms were present in 39 (50%) of wellness surveys, with 14 (82%) residents reporting burnout at one or more time points. April 2020 had the lowest burnout prevalence (41%), while January 2021 had the highest burnout prevalence (60%) (Figure 1). No significant associations between burnout score and hair cortisol (β -0.01, 95% CI -0.14 to 0.13), oxytocin (β 0.06, 95% CI -0.06 to 0.19), or cortisol:oxytocin ratio (β -0.04, 95% CI -0.09 to 0.02) were noted. Hair cortisol reactivity was not associated with burnout reactivity (Figure 2).Conclusion(s): Burnout is prevalent among pediatrics residents, with highest burnout apparent by January 2021. Hair cortisol and oxytocin did not significantly associate with burnout in this pilot study.
Figure 1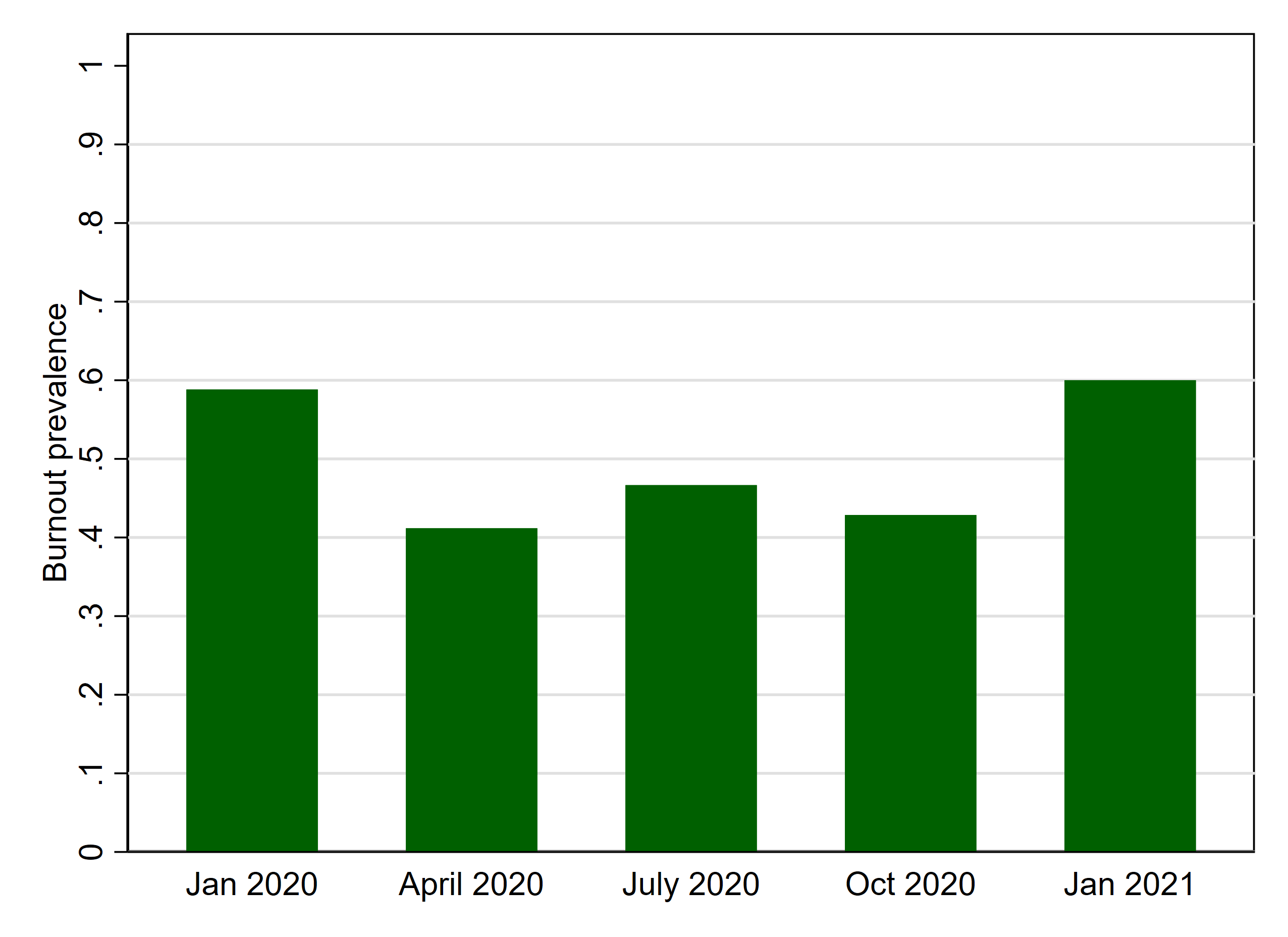 Burnout prevalence during 5 study timeponts. N = 17 pediatrics residents.
Burnout prevalence during 5 study timeponts. N = 17 pediatrics residents.
Figure 2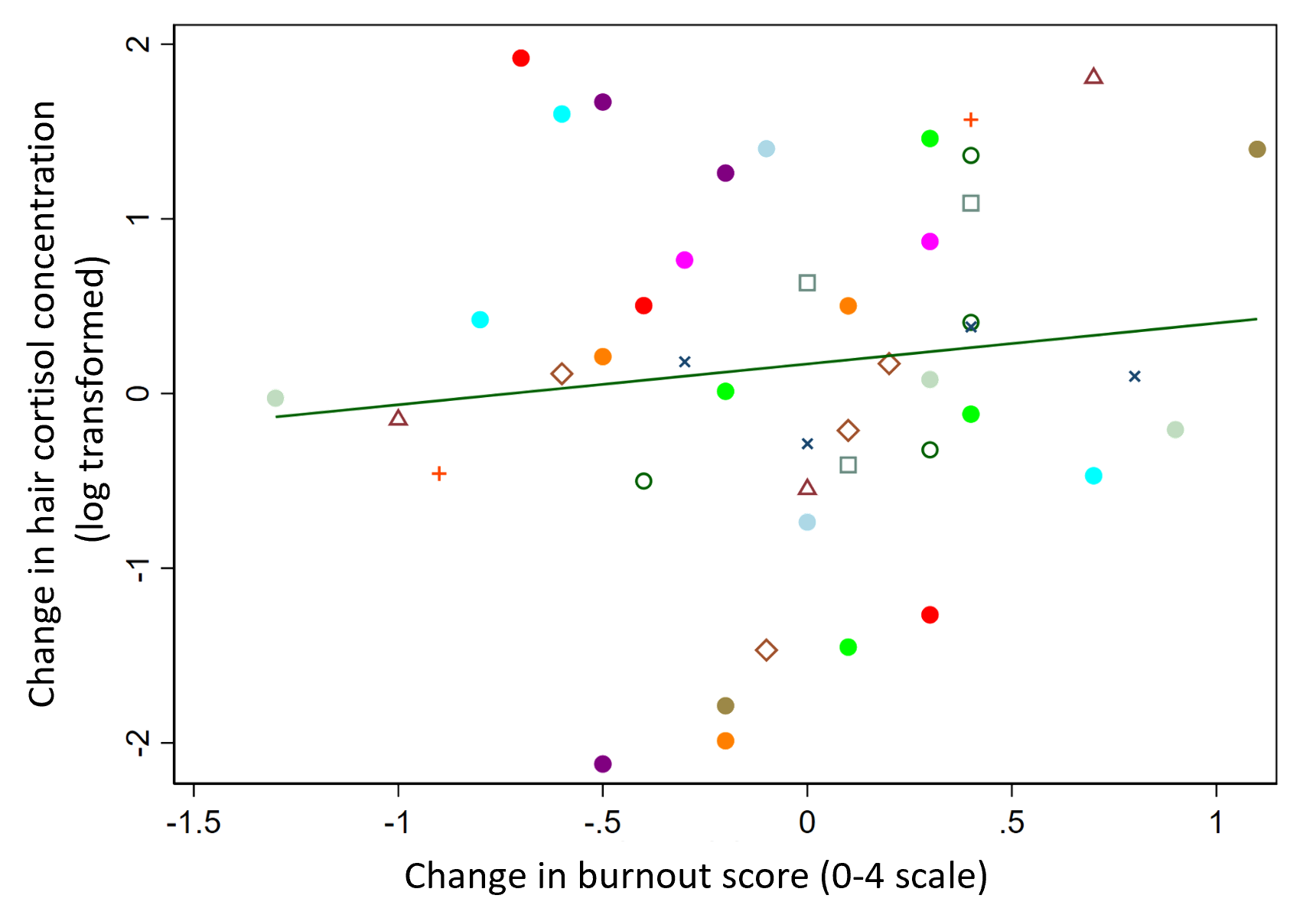 Change in hair cortisol concentration (log-transformed) between adjacent time points, in relation to change in burnout score (0-4 scale) during the same time interval. N = 45 time intervals from 15 pediatrics residents.
Change in hair cortisol concentration (log-transformed) between adjacent time points, in relation to change in burnout score (0-4 scale) during the same time interval. N = 45 time intervals from 15 pediatrics residents.
Objective: Pilot study to determine feasibility and quantify longitudinal pediatric resident burnout in relation to hair cortisol and hair oxytocin concentrations.
Design/Methods: Longitudinal observational cohort study of pediatric residents that assessed burnout using the Stanford Professional Fulfillment Index, hair cortisol and hair oxytocin at 3-month intervals from January 2020-January 2021. We evaluated test-retest reliability, sensitivity to change using Pearson product-moment correlations, and relationships between burnout and hair biomarkers using hierarchical mixed-effects linear regressions.
Results: We evaluated 17 Pediatrics residents with 78 wellness surveys and 54 hair samples. Burnout symptoms were present in 39 (50%) of wellness surveys, with 14 (82%) residents reporting burnout at one or more time points. April 2020 had the lowest burnout prevalence (41%), while January 2021 had the highest burnout prevalence (60%) (Figure 1). No significant associations between burnout score and hair cortisol (β -0.01, 95% CI -0.14 to 0.13), oxytocin (β 0.06, 95% CI -0.06 to 0.19), or cortisol:oxytocin ratio (β -0.04, 95% CI -0.09 to 0.02) were noted. Hair cortisol reactivity was not associated with burnout reactivity (Figure 2).Conclusion(s): Burnout is prevalent among pediatrics residents, with highest burnout apparent by January 2021. Hair cortisol and oxytocin did not significantly associate with burnout in this pilot study.
Figure 1
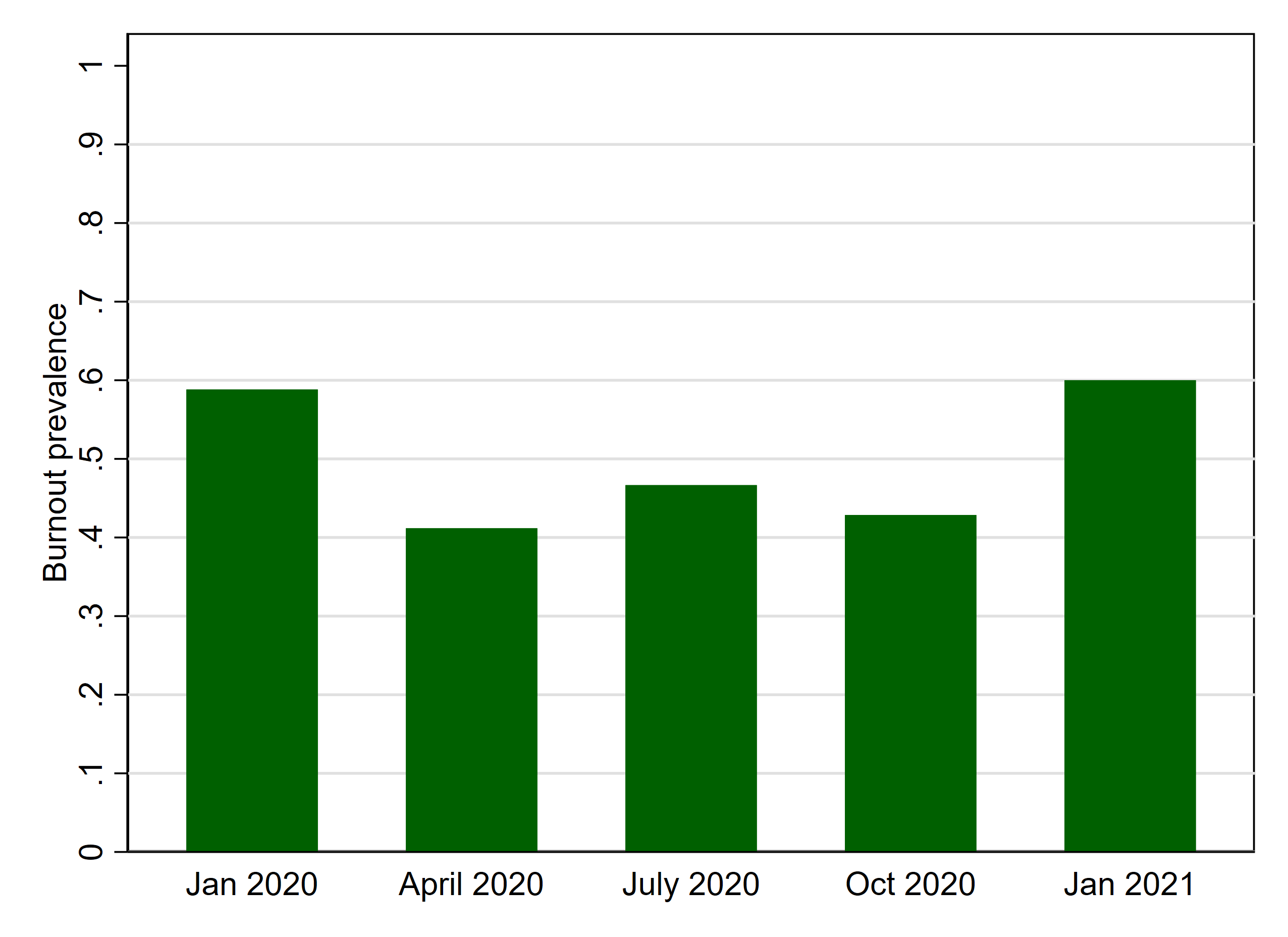 Burnout prevalence during 5 study timeponts. N = 17 pediatrics residents.
Burnout prevalence during 5 study timeponts. N = 17 pediatrics residents.Figure 2
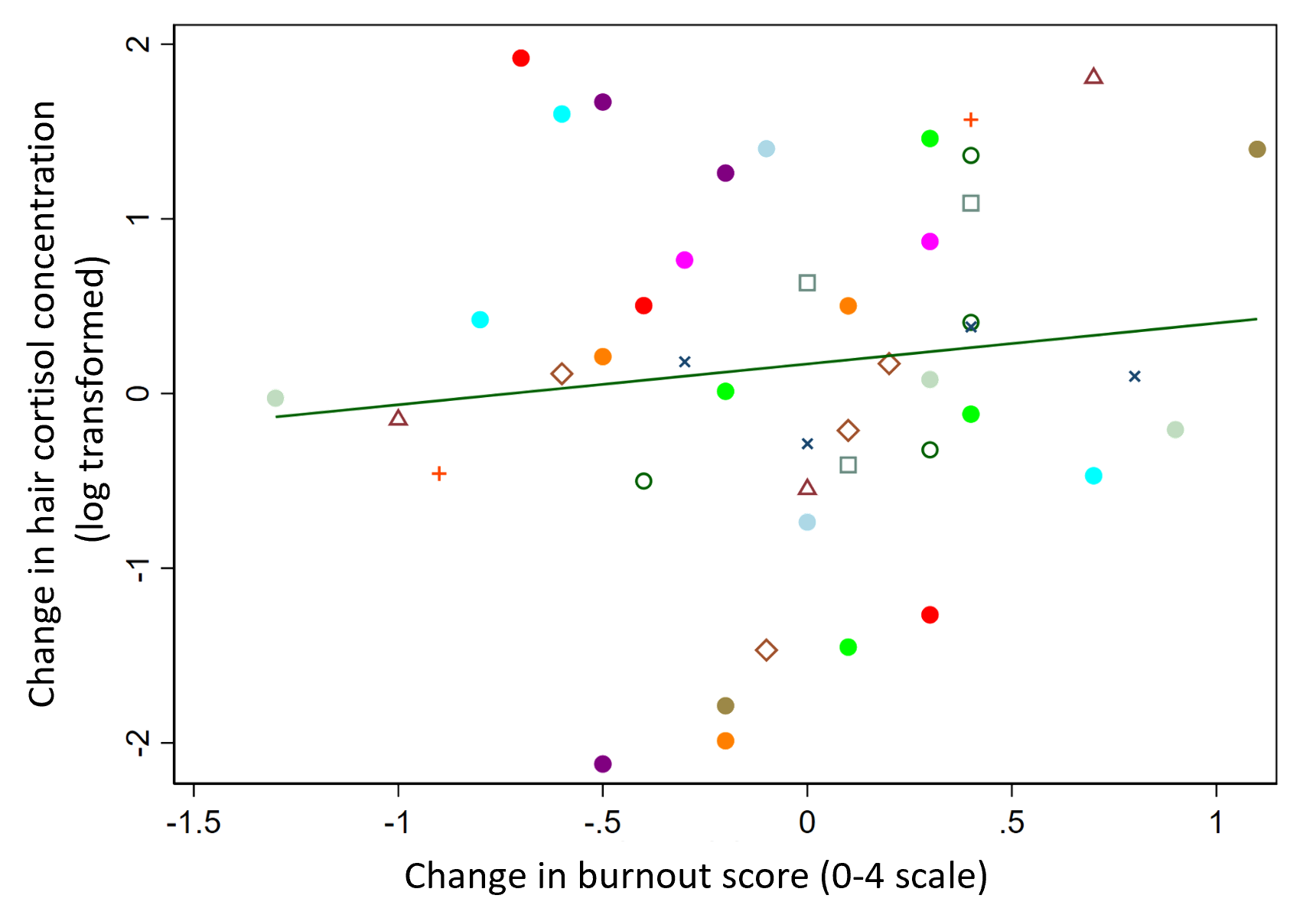 Change in hair cortisol concentration (log-transformed) between adjacent time points, in relation to change in burnout score (0-4 scale) during the same time interval. N = 45 time intervals from 15 pediatrics residents.
Change in hair cortisol concentration (log-transformed) between adjacent time points, in relation to change in burnout score (0-4 scale) during the same time interval. N = 45 time intervals from 15 pediatrics residents.