Neonatal Hematology & Bilirubin Metabolism
Category: Abstract Submission
Neonatal Hematology & Bilirubin Metabolism I
340 - Predicting neonatal mortality with a disseminated intravascular coagulation scoring system
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 340
Publication Number: 340.122
Publication Number: 340.122
Hayato Go, Fukushima Medical University, Fukushima, Fukushima, Japan; Hajime Maeda, Brown University, Providence, RI, United States; Kei Ogasawara, Fukushima medical university, Fukushima, Fukushima, Japan; Mitsuaki Hosoya, Fukushima Medical University, Fukushima, Fukushima, Japan
- HG
Hayato Go (he/him/his)
Associate professor
Fukushima Medical University
Fukushima Medical University
Fukushima, Fukushima, Japan
Presenting Author(s)
Background: Disseminated intravascular coagulation (DIC) is a critical disease that can provoke organ failure as well as severe bleeding from thrombocytopenia and irregular coagulation parameters. However, gold standard interventions and treatments for DIC are lacking in neonatal medicine. We previously reported that, especially at birth, asphyxia was the predominant cause of DIC, but the DIC score at birth did not predict mortality. On the other hand, reports are lacking about diseases associated with neonatal DIC diagnosed on or after the second day of life and whether anything predicts mortality in this context.
Objective: The aims of this study were to investigate underlying diseases associated with neonatal DIC diagnosed on or after the second day of life through 28 days of life, and whether DIC score could predict mortality in neonates.
Design/Methods: This retrospective cohort study, using records from January 2010 to November 2019, was conducted at the Neonatal Intensive Care Unit (NICU) of Fukushima Medical University Hospital (FMU). We enrolled only neonates diagnosed with DIC from the second day of life to 28 days of life, but excluded those who were diagnosed with DIC at birth. The Ethics Committee of FMU, guided by local policy, national law, and the World Medical Association Declaration of Helsinki, approved this study without requiring informed consent from guardians. We retrospectively evaluated the DIC scores of neonates diagnosed on or after the second day of life, in conjunction with underlying conditions associated with DIC. DIC was diagnosed according to Japan Society of Obstetrical, Gynecological & Neonatal Hematology (JSOGNH) 2016 neonatal DIC criteria.
Results: Among 23 neonates with DIC, 8 had gastrointestinal perforation with necrotizing enterocolitis and 6 had congenital heart disease (Table 1). Although factors such as birth weight, gestational age, D-dimer and fibrinogen were not predictive of mortality, a significant difference emerged in median PT-INR between the two groups (survived 1.69 vs died 2.42, P=0.005). Furthermore, the median DIC scores were statistically different for outcomes of death and survival (P=0.013) (Table 2). Multivariate analysis showed that DIC scores and PT-INR were significantly associated with mortality among neonate with DIC (Table 3).Conclusion(s): DIC scores based on JSOGNH2016 neonatal DIC criteria are predictive of mortality in infants diagnosed with DIC on or after the second day of life.
Table 1. Underlying diseases in 23 neonates diagnosed with DIC on or after the second day of life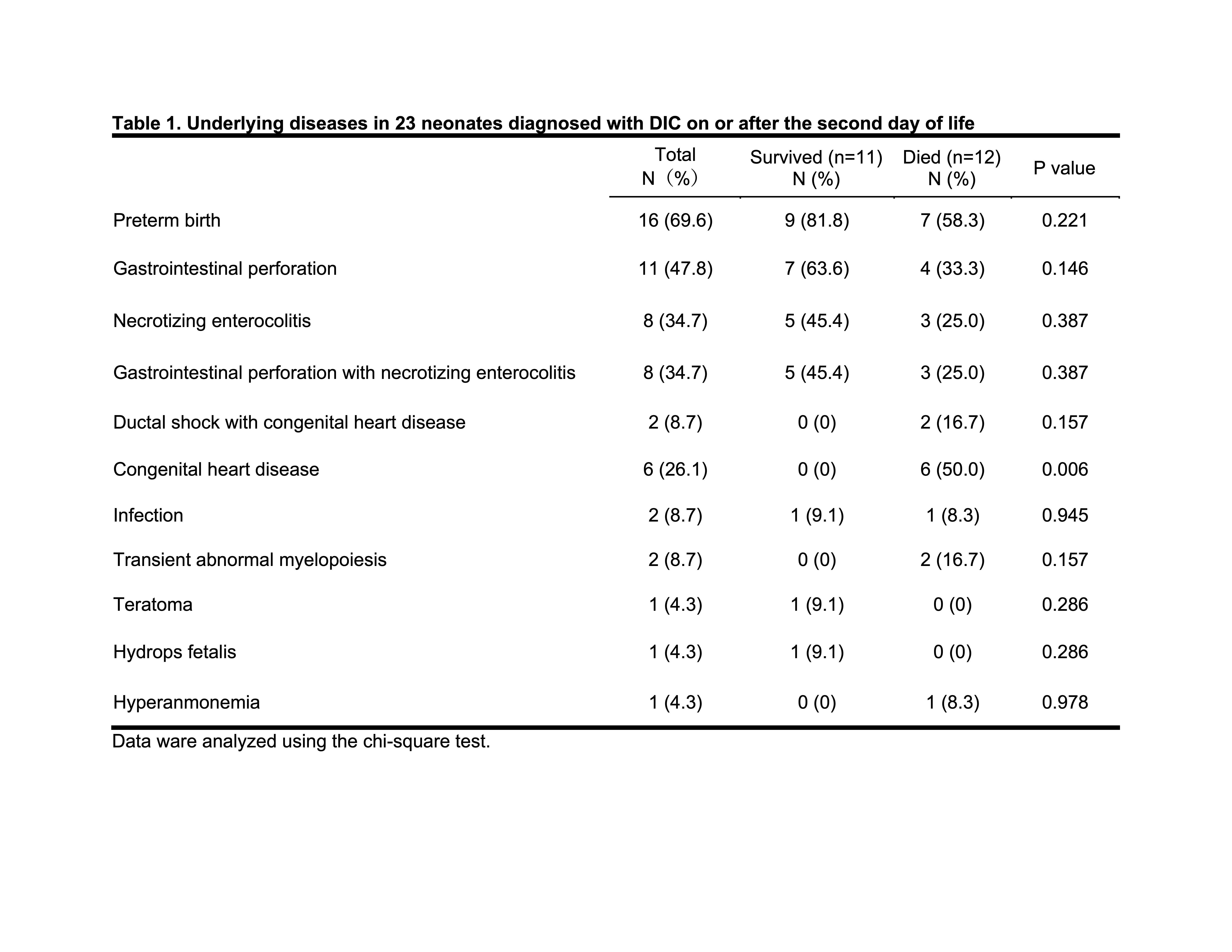
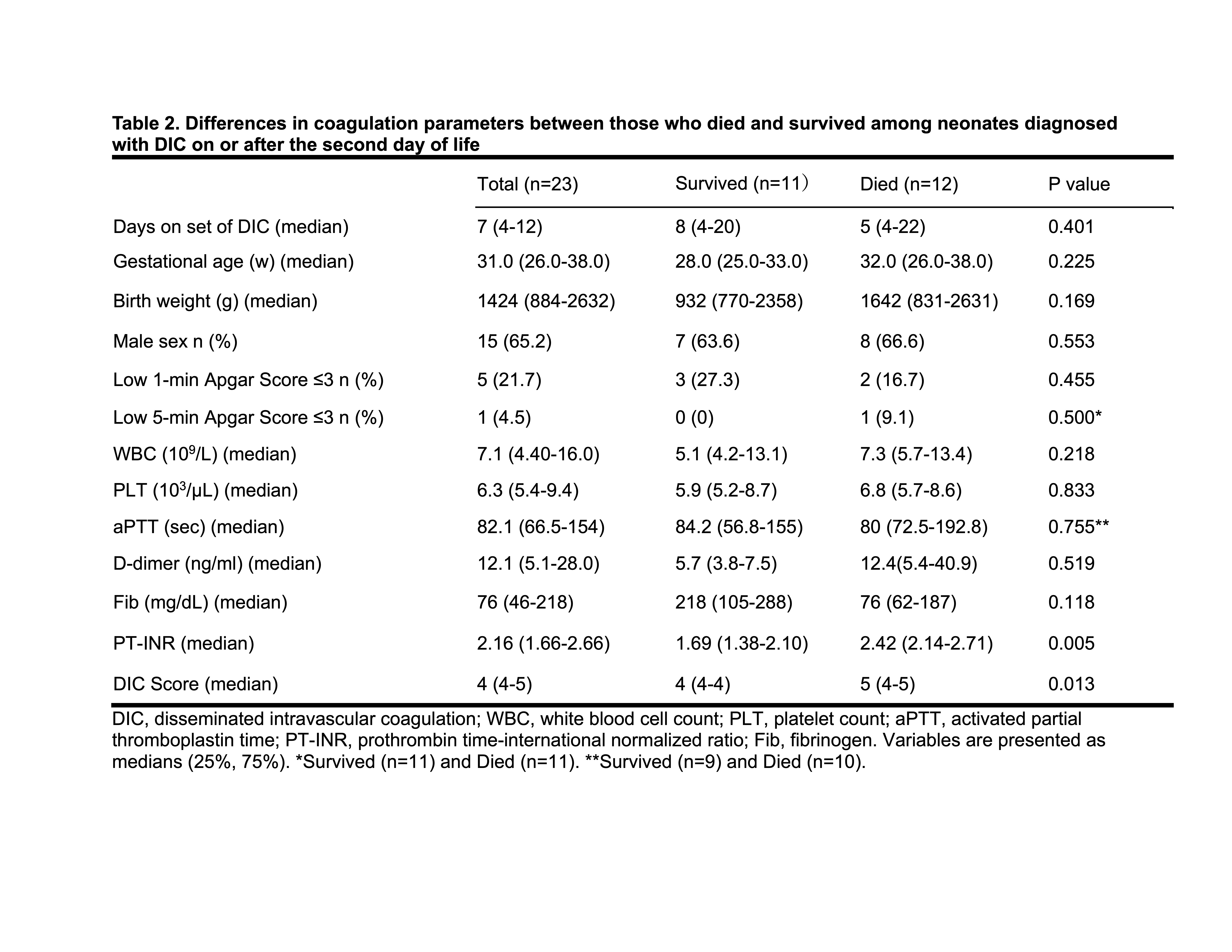
Table 2. Differences in coagulation parameters between those who died and survived among neonates diagnosed with DIC on or after the second day of life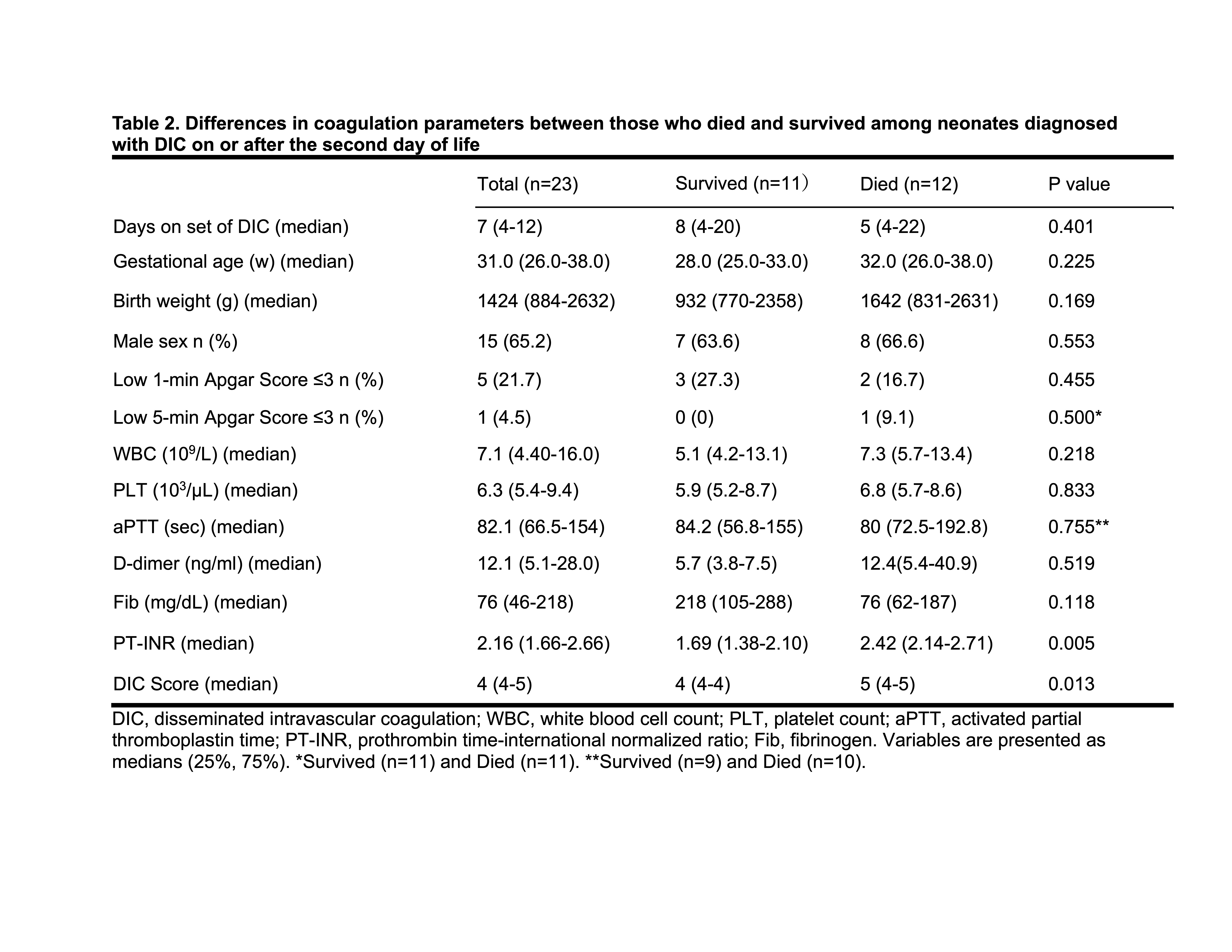
Objective: The aims of this study were to investigate underlying diseases associated with neonatal DIC diagnosed on or after the second day of life through 28 days of life, and whether DIC score could predict mortality in neonates.
Design/Methods: This retrospective cohort study, using records from January 2010 to November 2019, was conducted at the Neonatal Intensive Care Unit (NICU) of Fukushima Medical University Hospital (FMU). We enrolled only neonates diagnosed with DIC from the second day of life to 28 days of life, but excluded those who were diagnosed with DIC at birth. The Ethics Committee of FMU, guided by local policy, national law, and the World Medical Association Declaration of Helsinki, approved this study without requiring informed consent from guardians. We retrospectively evaluated the DIC scores of neonates diagnosed on or after the second day of life, in conjunction with underlying conditions associated with DIC. DIC was diagnosed according to Japan Society of Obstetrical, Gynecological & Neonatal Hematology (JSOGNH) 2016 neonatal DIC criteria.
Results: Among 23 neonates with DIC, 8 had gastrointestinal perforation with necrotizing enterocolitis and 6 had congenital heart disease (Table 1). Although factors such as birth weight, gestational age, D-dimer and fibrinogen were not predictive of mortality, a significant difference emerged in median PT-INR between the two groups (survived 1.69 vs died 2.42, P=0.005). Furthermore, the median DIC scores were statistically different for outcomes of death and survival (P=0.013) (Table 2). Multivariate analysis showed that DIC scores and PT-INR were significantly associated with mortality among neonate with DIC (Table 3).Conclusion(s): DIC scores based on JSOGNH2016 neonatal DIC criteria are predictive of mortality in infants diagnosed with DIC on or after the second day of life.
Table 1. Underlying diseases in 23 neonates diagnosed with DIC on or after the second day of life
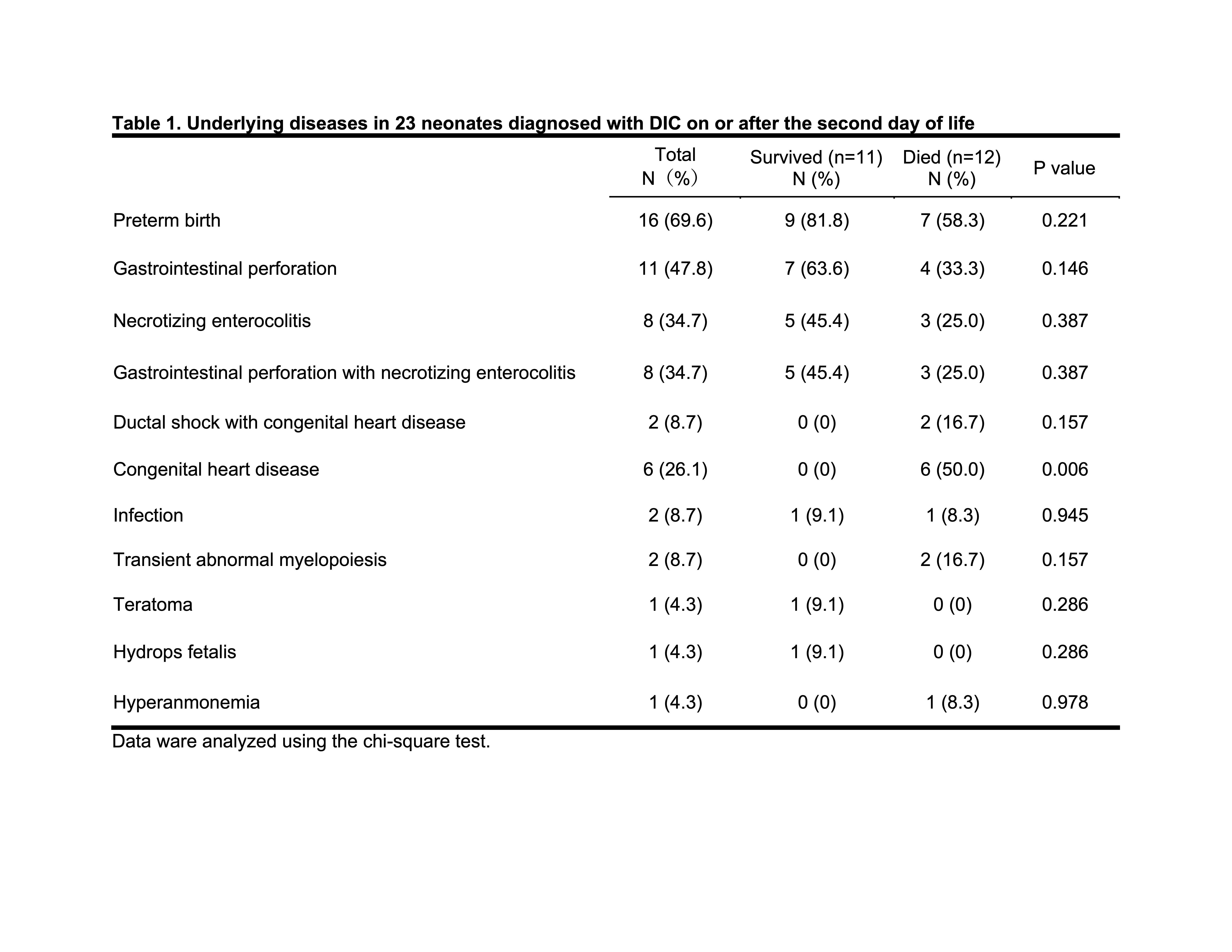
Table 2. Differences in coagulation parameters between those who died and survived among neonates diagnosed with DIC on or after the second day of life