Back
Neonatal General
Category: Abstract Submission
Neonatology General 6: NOWS - Maternal-Fetal Exposures
424 - Prenatal Lead Exposure and Auditory Toxicity in Premature Infants
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 424
Sanjiv Amin, Children's Hospital of Michigan, Detroit, MI, United States; Mark S. Orlando, University of Rochester ehster, Rochester, NY, United States
- SA
Sanjiv Amin, MD, MS
Professor of Pediatrics
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Prenatal low-level lead exposure has been associated with developmental delay in children born at term gestation. Auditory brainstem evoked response (ABR) has been shown to be a sensitive detector of subclinical lead exposure effects on the developing nervous system in term neonates and children. Premature infants may be at increased risk of neurotoxicity from subclinical lead exposure. However, there is limited data on the effects of low-level lead exposure on the developing nervous system in premature infants.
Objective: To evaluate if prenatal low-level lead exposure is associated with auditory toxicity as evaluated by ABR at 35 weeks post-menstrual age (PMA) in premature infants.
Design/Methods: A prospective study was performed involving infants ≤ 33 weeks gestational age (GA). Infants with cranial facial malformations, chromosomal disorders, family history of deafness/auditory neuropathy, maternal drug use, TORCH infections, or who were transferred to other hospitals were excluded. Cord blood lead (Pb) levels were measured using Inductively Coupled Plasma Mass Spectrometry. ABRs were performed by an audiologist at 35 weeks PMA using 80 dB click stimuli presented to each ear with a click rate of 29.9/sec. Interpeak latencies (IPL), a measure of auditory neural myelination, were measured for each ear. IPL decreases with improvement in myelination.
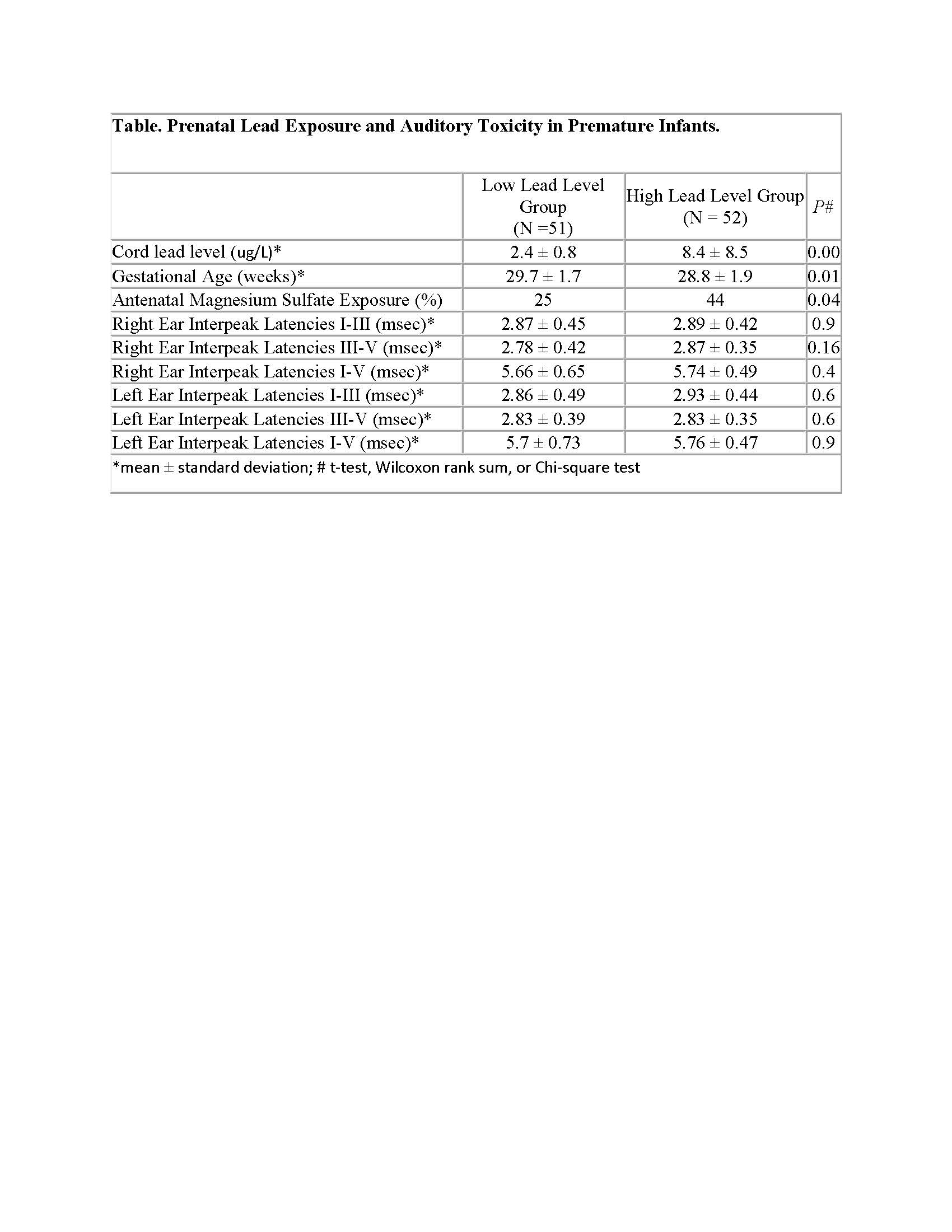
Results: 110 infants were enrolled, of which 3 died and 4 met exclusion criteria. The median Pb level of 103 infants was 3.7 ug/L and was used to subdivide into 2 groups: Low Lead Group (Pb < 3.7 ug/L) and High Lead Group (Pb ≥ 3.7 ug/L). There was no significant difference in clinical factors including birth weight, gender, race, mode of delivery, Apgar score ≤ 3 at 5 minutes, chorioamnionitis, maternal hypertension, antenatal steroid exposure, respiratory distress syndrome, patent ductus arteriosus, necrotizing enterocolitis, intraventricular hemorrhage, peak total serum bilirubin level, days on oxygen, culture proven sepsis, type of enteral feeding, or days on parenteral nutrition between the 2 groups. There was a significant difference in GA and antenatal magnesium sulfate exposure between the 2 groups (Table). There was no significant difference in IPL I-III, III-V, and I-V in either ear between the 2 groups (Table). On regression analyses, controlling for confounders, the High Lead Group was not associated with an increase in I-III, III-V, and I-V IPLs in either ear compared to the Low Lead Group (p >0.3). Conclusion(s): Prenatal low lead level exposure may not be associated with auditory toxicity when evaluated at 35 weeks PMA in premature infants.
Table. Prenatal Lead Exposure and Auditory Toxicity in Premature Infants.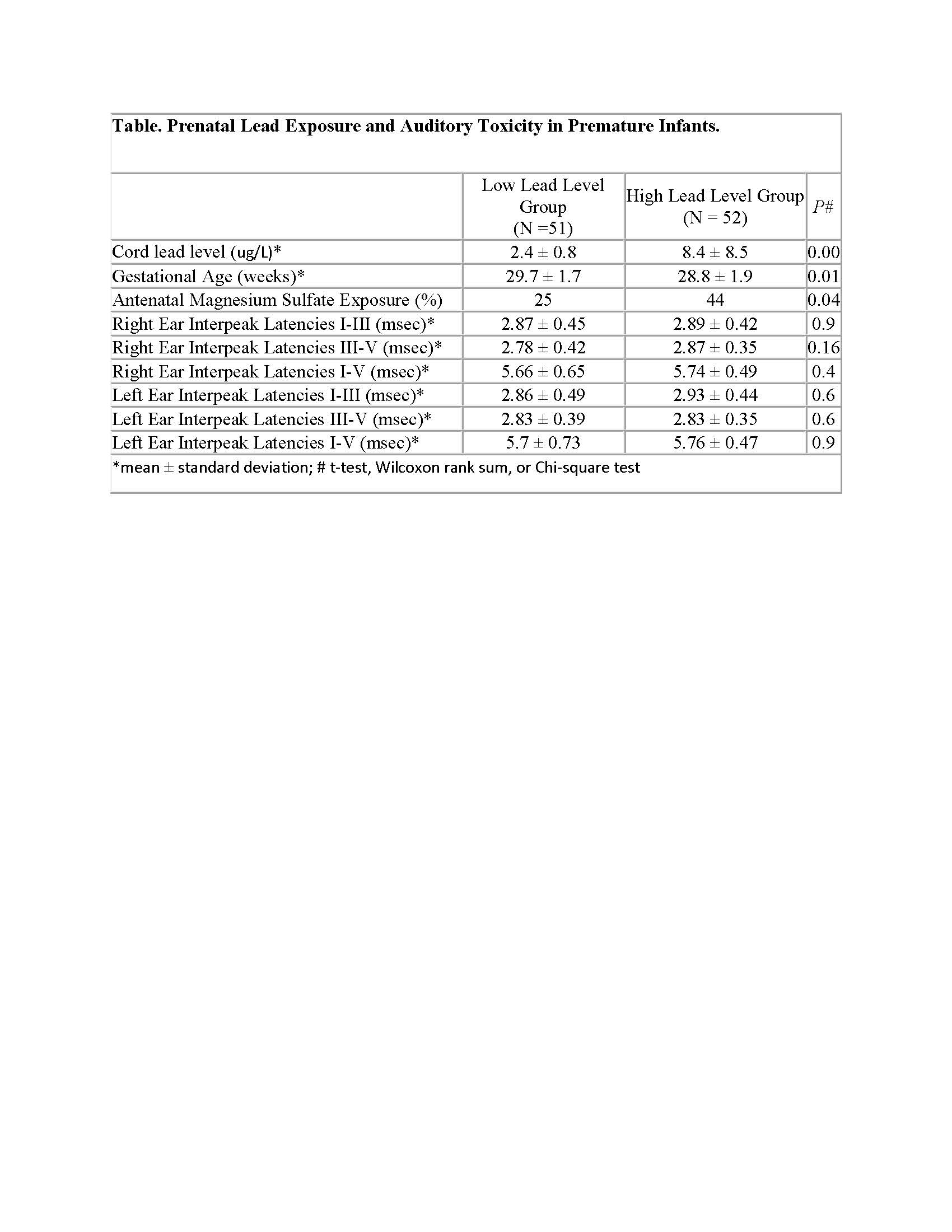
Objective: To evaluate if prenatal low-level lead exposure is associated with auditory toxicity as evaluated by ABR at 35 weeks post-menstrual age (PMA) in premature infants.
Design/Methods: A prospective study was performed involving infants ≤ 33 weeks gestational age (GA). Infants with cranial facial malformations, chromosomal disorders, family history of deafness/auditory neuropathy, maternal drug use, TORCH infections, or who were transferred to other hospitals were excluded. Cord blood lead (Pb) levels were measured using Inductively Coupled Plasma Mass Spectrometry. ABRs were performed by an audiologist at 35 weeks PMA using 80 dB click stimuli presented to each ear with a click rate of 29.9/sec. Interpeak latencies (IPL), a measure of auditory neural myelination, were measured for each ear. IPL decreases with improvement in myelination.
Results: 110 infants were enrolled, of which 3 died and 4 met exclusion criteria. The median Pb level of 103 infants was 3.7 ug/L and was used to subdivide into 2 groups: Low Lead Group (Pb < 3.7 ug/L) and High Lead Group (Pb ≥ 3.7 ug/L). There was no significant difference in clinical factors including birth weight, gender, race, mode of delivery, Apgar score ≤ 3 at 5 minutes, chorioamnionitis, maternal hypertension, antenatal steroid exposure, respiratory distress syndrome, patent ductus arteriosus, necrotizing enterocolitis, intraventricular hemorrhage, peak total serum bilirubin level, days on oxygen, culture proven sepsis, type of enteral feeding, or days on parenteral nutrition between the 2 groups. There was a significant difference in GA and antenatal magnesium sulfate exposure between the 2 groups (Table). There was no significant difference in IPL I-III, III-V, and I-V in either ear between the 2 groups (Table). On regression analyses, controlling for confounders, the High Lead Group was not associated with an increase in I-III, III-V, and I-V IPLs in either ear compared to the Low Lead Group (p >0.3). Conclusion(s): Prenatal low lead level exposure may not be associated with auditory toxicity when evaluated at 35 weeks PMA in premature infants.
Table. Prenatal Lead Exposure and Auditory Toxicity in Premature Infants.