Neonatal General
Category: Abstract Submission
Neonatology General 6: NOWS - Maternal-Fetal Exposures
425 - Prenatal Methamphetamine Exposure Results in Frequent Adverse Short-Term Outcomes in Infants
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 425
Publication Number: 425.136
Publication Number: 425.136
Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States; Catherine A. Rottkamp, University of California Davis, Sacramento, CA, United States; Rosa R. Pesavento, University of California, Davis, School of Medicine, Sacramento, CA, United States; Heather Siefkes, University of California, Davis, Sacramento, CA, United States; Veena Manja, Stanford University School of Medicine, Sacramento, CA, United States; Satyan Lakshminrusimha, University of California Davis Children's Hospital, Sacramento, CA, United States

Deepika Sankaran, MD
Neonatologist
University of California Davis Children's Hospital
Sacramento, California, United States
Presenting Author(s)
Background: Methamphetamine (MA) use is increasing among women of childbearing age (Kevil, C.G et al. 2019). Fetal growth restriction and neurobehavioral effects in offspring are linked to prenatal MA exposure (Eze et al 2016). Prevalence of MA use among deliveries and disposition of infants at discharge in urban and rural areas in Northern California is unknown.
Objective: To compare the prevalence of MA use among women delivering at an urban university hospital and a rural community hospital in Northern California, and to assess short-term neonatal outcomes.
Design/Methods: We performed a retrospective study of women who delivered at the University of California Davis Children’s (Urban University) Hospital and Adventist Health-Rideout (Rural Community) Hospital to identify prenatal MA use during August 2020 to November 2021. We collected maternal demographics (age, self-reported Race), social and obstetrical history, health insurance, urine toxicology results, infant’s gestational age at birth, birth weight, need for intensive care (NICU) admission, and disposition at discharge.
Results: Among 2229 (29% non-Hispanic White, 38% Medicaid) and 2446 (33.5% non-Hispanic White, 63% Medicaid) deliveries during the 16-month study period, 45 (2.0%) and 42 (1.7%) mothers tested positive for MA at the university and community hospitals respectively (p=0.1). Age and mode of delivery were similar between the two settings, but ethnicity/race and health insurance were different with higher prevalence of MA use among non-Hispanic White (71%, p=0.04) and mothers on Medicaid (93%, p< 0.001) in the rural hospital (Table 1). Eighty-two percent (urban) and 88% (rural) of mothers had limited or no prenatal care, and more than a third were homeless (Table 1). Maternal comorbidities identified (Table 1) included history of hypertension, preeclampsia, heart failure, stroke, and mental illness. More than half of the infants required NICU care (Table 2). Three-quarters of the infants were discharged to foster care (Table 2).Conclusion(s): Prenatal MA use is prevalent in urban and rural areas, is associated with limited prenatal care, homelessness, significant maternal and neonatal comorbidities, and adverse short-term neonatal outcomes. Over half of the newborns required NICU admission and majority were discharged to foster care. Significant gaps exist in healthcare access and delivery for pregnant women using MA. Targeted antenatal interventions for high-risk groups in urban and rural areas may improve maternal and neonatal outcomes.
Table 1: Comparison of maternal characteristics between mothers testing positive for methamphetamine delivering at the urban University hospital and rural Community hospital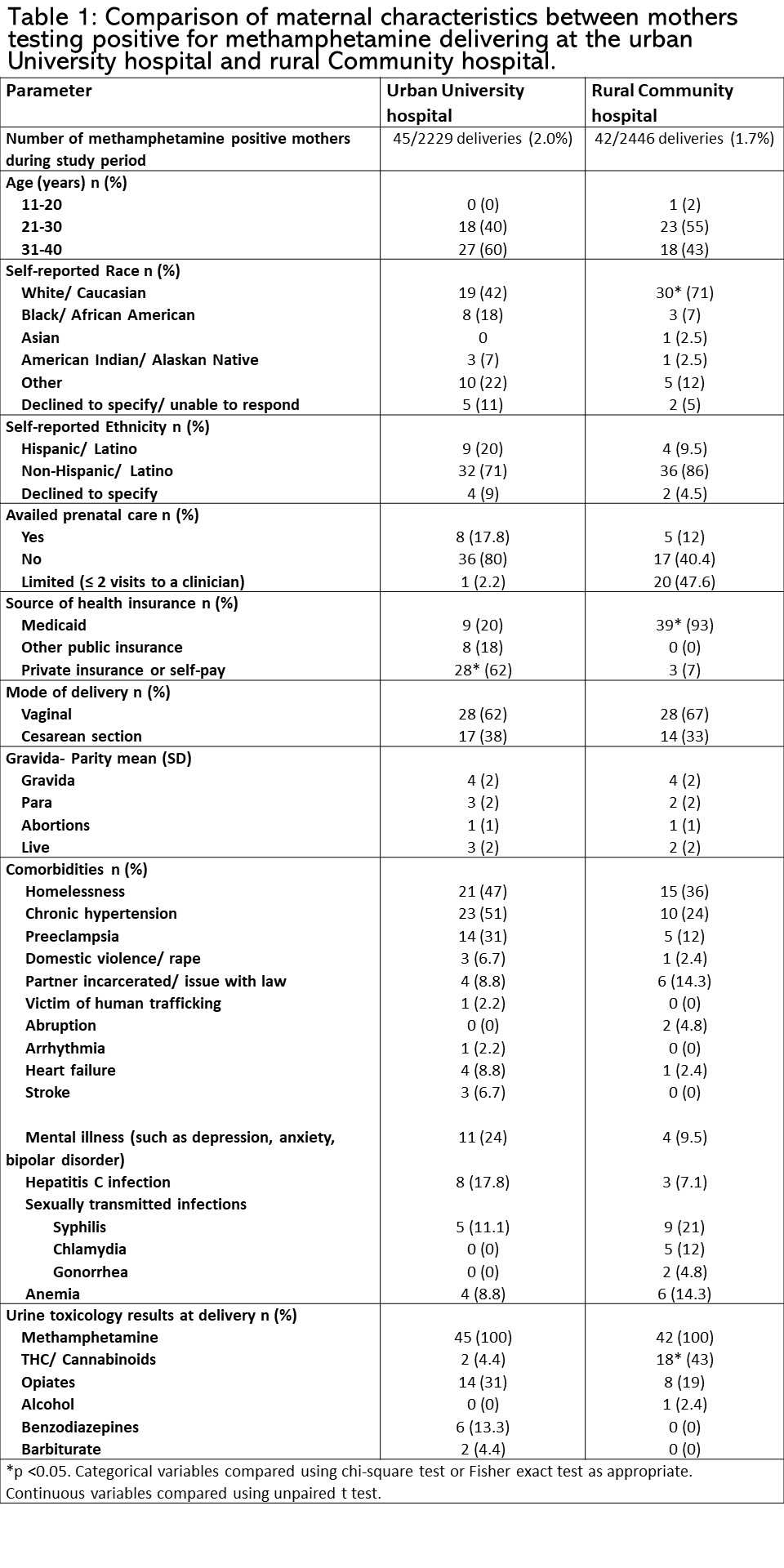 *p < 0.05. Categorical variables compared using chi-square test or Fisher exact test as appropriate. Continuous variables compared using unpaired t test.
*p < 0.05. Categorical variables compared using chi-square test or Fisher exact test as appropriate. Continuous variables compared using unpaired t test.
Table 2: Infant characteristics and short-term outcomes after prenatal methamphetamine exposure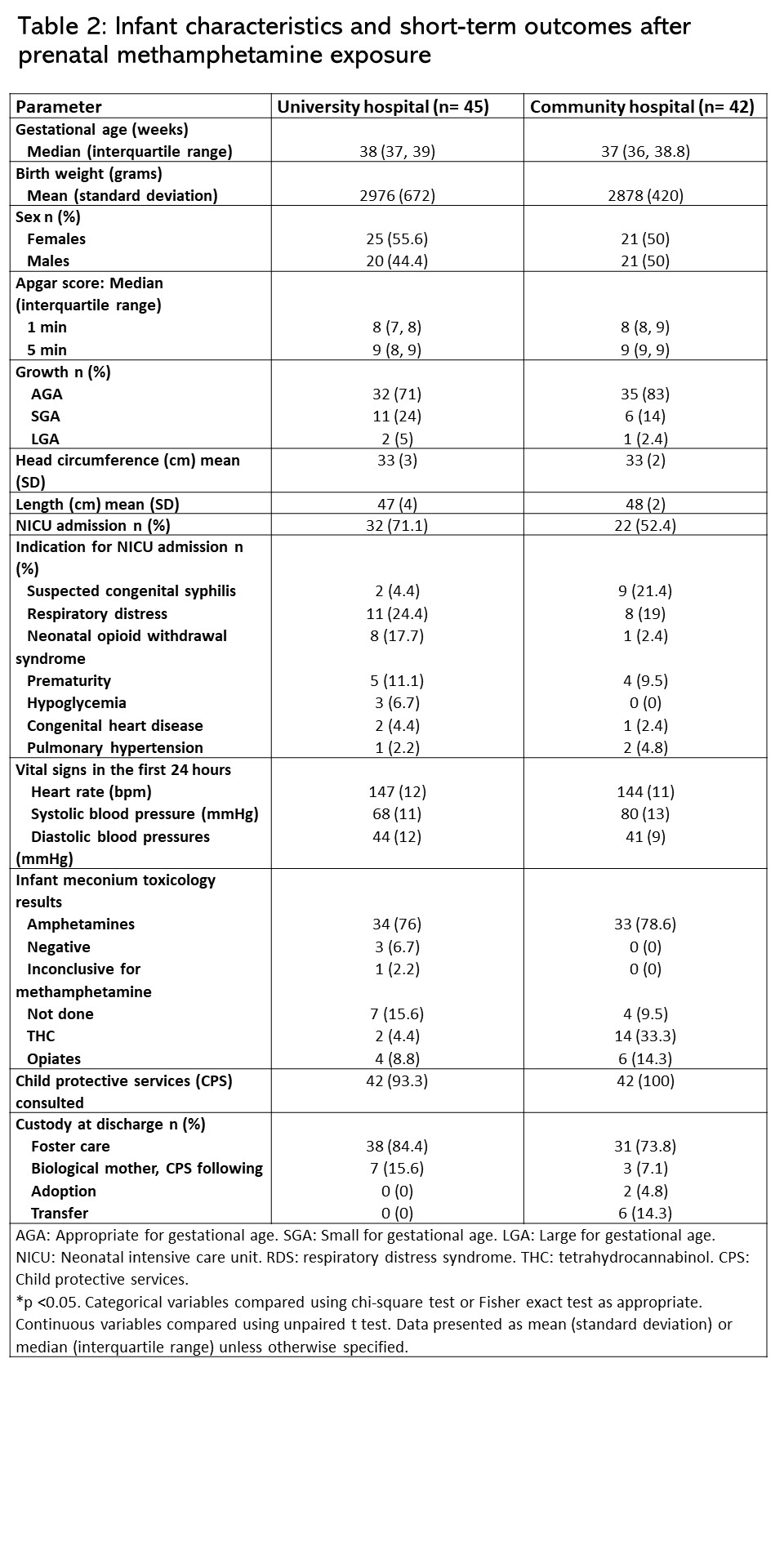 AGA: Appropriate for gestational age. SGA: Small for gestational age. LGA: Large for gestational age. NICU: Neonatal intensive care unit. RDS: respiratory distress syndrome. THC: tetrahydrocannabinol. CPS: Child protective services.
AGA: Appropriate for gestational age. SGA: Small for gestational age. LGA: Large for gestational age. NICU: Neonatal intensive care unit. RDS: respiratory distress syndrome. THC: tetrahydrocannabinol. CPS: Child protective services.
*p < 0.05. Categorical variables compared using chi-square test or Fisher exact test as appropriate. Continuous variables compared using unpaired t test. Data presented as mean (standard deviation) or median (interquartile range) unless otherwise specified.
Objective: To compare the prevalence of MA use among women delivering at an urban university hospital and a rural community hospital in Northern California, and to assess short-term neonatal outcomes.
Design/Methods: We performed a retrospective study of women who delivered at the University of California Davis Children’s (Urban University) Hospital and Adventist Health-Rideout (Rural Community) Hospital to identify prenatal MA use during August 2020 to November 2021. We collected maternal demographics (age, self-reported Race), social and obstetrical history, health insurance, urine toxicology results, infant’s gestational age at birth, birth weight, need for intensive care (NICU) admission, and disposition at discharge.
Results: Among 2229 (29% non-Hispanic White, 38% Medicaid) and 2446 (33.5% non-Hispanic White, 63% Medicaid) deliveries during the 16-month study period, 45 (2.0%) and 42 (1.7%) mothers tested positive for MA at the university and community hospitals respectively (p=0.1). Age and mode of delivery were similar between the two settings, but ethnicity/race and health insurance were different with higher prevalence of MA use among non-Hispanic White (71%, p=0.04) and mothers on Medicaid (93%, p< 0.001) in the rural hospital (Table 1). Eighty-two percent (urban) and 88% (rural) of mothers had limited or no prenatal care, and more than a third were homeless (Table 1). Maternal comorbidities identified (Table 1) included history of hypertension, preeclampsia, heart failure, stroke, and mental illness. More than half of the infants required NICU care (Table 2). Three-quarters of the infants were discharged to foster care (Table 2).Conclusion(s): Prenatal MA use is prevalent in urban and rural areas, is associated with limited prenatal care, homelessness, significant maternal and neonatal comorbidities, and adverse short-term neonatal outcomes. Over half of the newborns required NICU admission and majority were discharged to foster care. Significant gaps exist in healthcare access and delivery for pregnant women using MA. Targeted antenatal interventions for high-risk groups in urban and rural areas may improve maternal and neonatal outcomes.
Table 1: Comparison of maternal characteristics between mothers testing positive for methamphetamine delivering at the urban University hospital and rural Community hospital
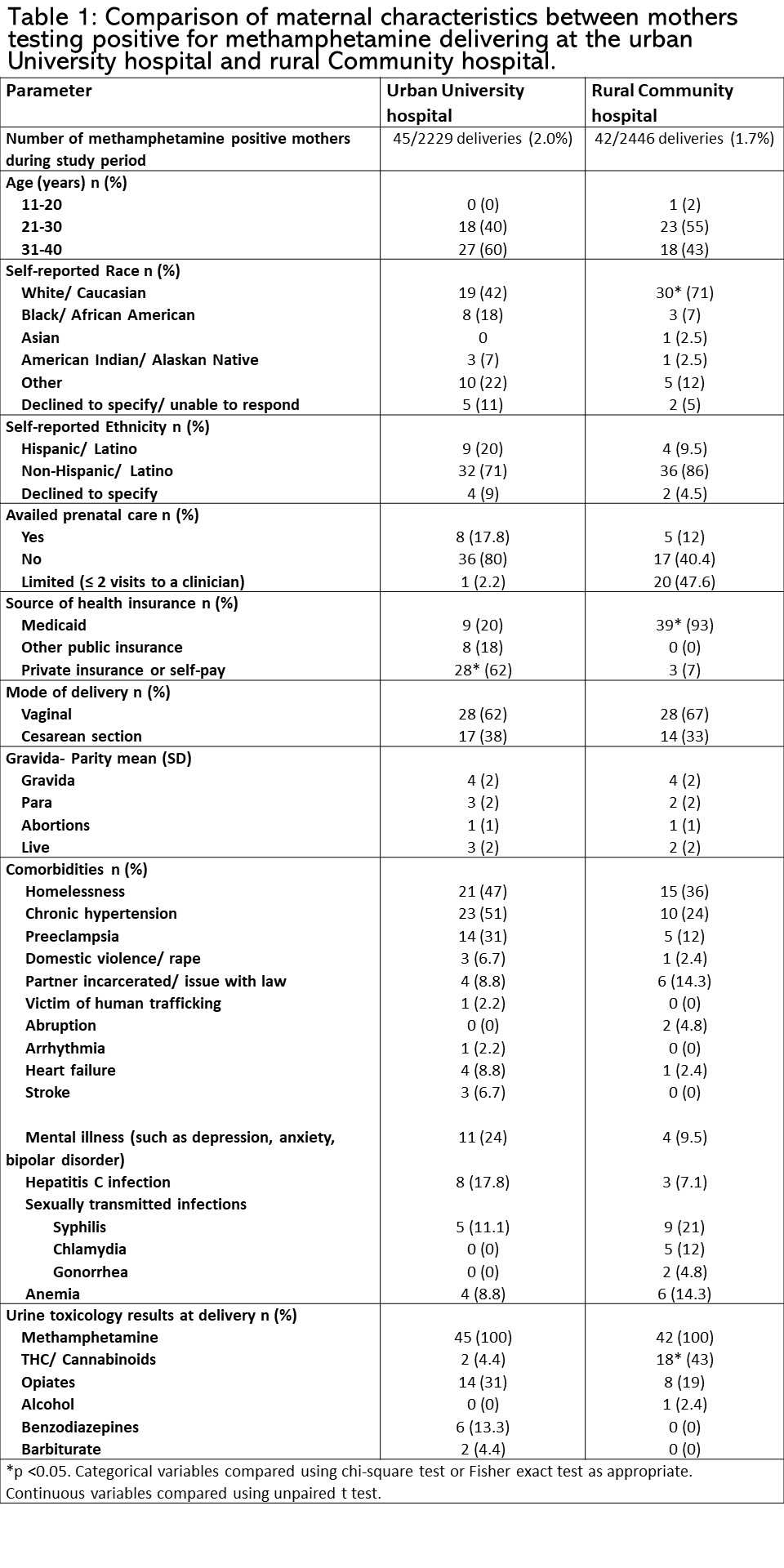 *p < 0.05. Categorical variables compared using chi-square test or Fisher exact test as appropriate. Continuous variables compared using unpaired t test.
*p < 0.05. Categorical variables compared using chi-square test or Fisher exact test as appropriate. Continuous variables compared using unpaired t test.Table 2: Infant characteristics and short-term outcomes after prenatal methamphetamine exposure
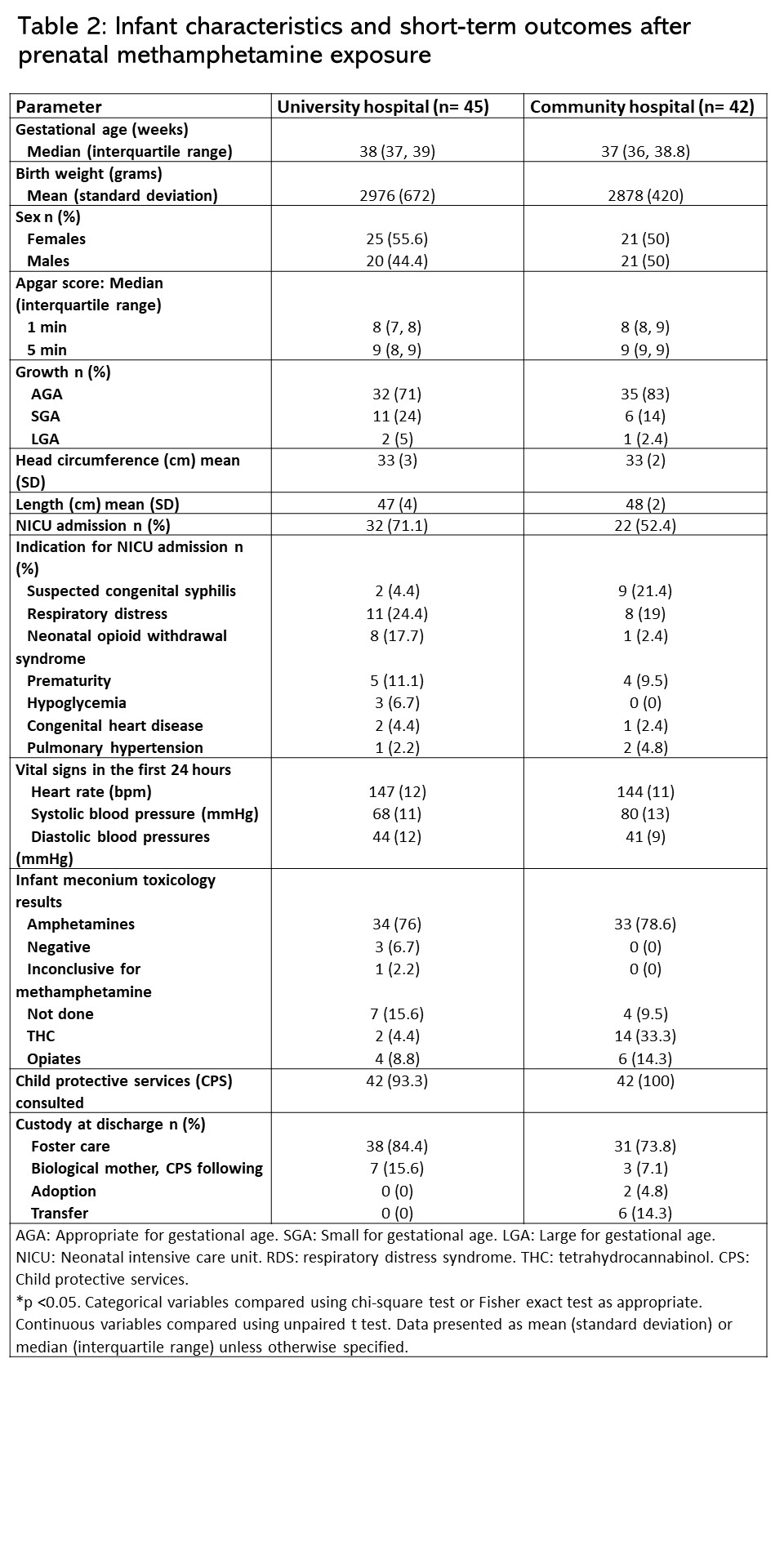 AGA: Appropriate for gestational age. SGA: Small for gestational age. LGA: Large for gestational age. NICU: Neonatal intensive care unit. RDS: respiratory distress syndrome. THC: tetrahydrocannabinol. CPS: Child protective services.
AGA: Appropriate for gestational age. SGA: Small for gestational age. LGA: Large for gestational age. NICU: Neonatal intensive care unit. RDS: respiratory distress syndrome. THC: tetrahydrocannabinol. CPS: Child protective services. *p < 0.05. Categorical variables compared using chi-square test or Fisher exact test as appropriate. Continuous variables compared using unpaired t test. Data presented as mean (standard deviation) or median (interquartile range) unless otherwise specified.
