Public Health & Prevention
Category: Abstract Submission
Public Health & Prevention II
577 - An Ethnographic Survey of Maternal Stress in a Ugandan Neonatal Hospital Unit
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 577
Publication Number: 577.241
Publication Number: 577.241
Delaney Barth, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Jessica Duby, McGill University Health Center, Montreal, PQ, Canada; Abner v. Tagoola, jinnja regional referral hospital, jinja, Jinja, Uganda; Olive Kabajaasi, Walimu Kampala Uganda, Kampala, Kampala, Uganda; Matthew O. Wiens, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Nancy Feeley, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada

Delaney A. Barth
Junior Research Assistant
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Presenting Author(s)
Background: Disruption of maternal-infant bonding, the hospital environment, and the appearance of an unwell child are common triggers of maternal stress in Neonatal Intensive Care Units (NICUs) in high-income countries. However, descriptions of maternal stress in low-income countries are lacking and may vary based on cultural differences or the scarcity of healthcare workers, equipment, and other resources.
Objective: We aimed to evaluate maternal stress and its contributing factors in a Ugandan neonatal hospital unit.
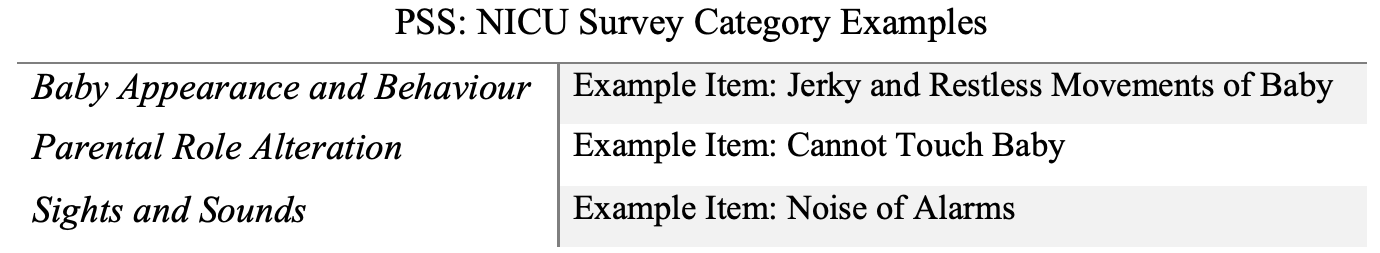
Design/Methods: The study was conducted at Jinja Regional Referral Hospital with a sample from the baseline cohort of a larger interventional trial. Inclusion was restricted to full-term infants requiring hospitalization in the Special Care Neonatal Unit. Demographic data was collected by chart review and surveys. Maternal stress was evaluated with the Parental Stressor Scale: Neonatal Intensive Unit (PSS:NICU) survey 48-96 hours after admission. Responses are scored from not stressful (1) to extremely stressful (5), in 3 subscales: Baby Appearance and Behaviour, Parental Role Alteration, and Sights and Sounds (Figure 1). Hierarchical linear regression models were used to determine demographic factors associated with PSS: NICU scores.
Results: Forty-nine mother-baby dyads were included. Thirty-four mothers (69%) had received secondary or higher education, and 21 (43%) were first-time mothers (Table 1). Asphyxia was the most frequent (n=31, 62%) reason for hospitalization, and the median length of stay was seven days (IQR: 6-8 days). The mean maternal stress level on the PSS:NICU was 3.41±0.40, and subscales with the highest and lowest scores were Baby Appearance and Behaviour (3.91±0.39), and Sights and Sounds (2.66±0.75) respectively. No maternal or infant factors were associated with the overall PSS:NICU score. However, older mothers with higher education (r=1.37, p=0.018) had elevated Sights and Sounds scores. Female infants at an older gestational age (r=-0.33, p=0.024) were associated with lower Parental Role Alteration scores.Conclusion(s): The mean PSS:NICU score of 3.41 represents moderate to high maternal stress. While the mean score is comparable to that of high-income countries, Parental Role Alteration, which is typically the largest source of stress, was second to the Baby Appearance and Behaviour subscale. Interventions that reduce maternal stress in high-income countries may also be effective for Ugandan mothers. We suggest that efforts to reduce maternal stress begin at admission, as the median stay is only a week, and should include maternal education about typical baby appearance.
Delaney Barth - CV - LabsFinal.pdf
Figure 1: Examples of items in each PSS: NICU subscale.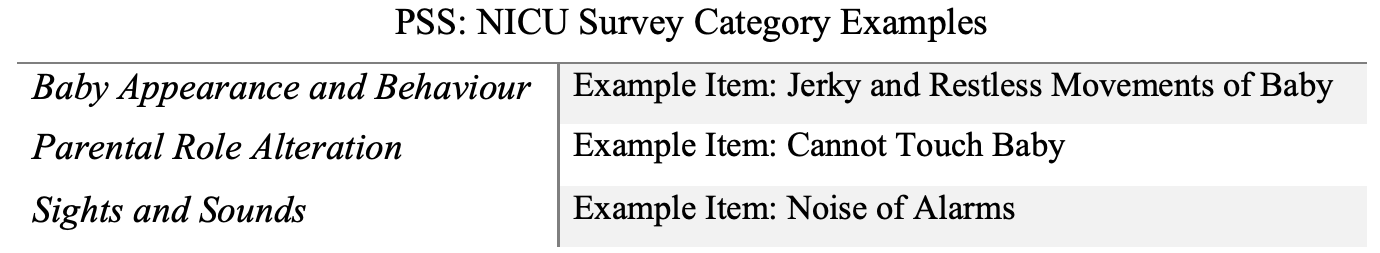
Objective: We aimed to evaluate maternal stress and its contributing factors in a Ugandan neonatal hospital unit.
Design/Methods: The study was conducted at Jinja Regional Referral Hospital with a sample from the baseline cohort of a larger interventional trial. Inclusion was restricted to full-term infants requiring hospitalization in the Special Care Neonatal Unit. Demographic data was collected by chart review and surveys. Maternal stress was evaluated with the Parental Stressor Scale: Neonatal Intensive Unit (PSS:NICU) survey 48-96 hours after admission. Responses are scored from not stressful (1) to extremely stressful (5), in 3 subscales: Baby Appearance and Behaviour, Parental Role Alteration, and Sights and Sounds (Figure 1). Hierarchical linear regression models were used to determine demographic factors associated with PSS: NICU scores.
Results: Forty-nine mother-baby dyads were included. Thirty-four mothers (69%) had received secondary or higher education, and 21 (43%) were first-time mothers (Table 1). Asphyxia was the most frequent (n=31, 62%) reason for hospitalization, and the median length of stay was seven days (IQR: 6-8 days). The mean maternal stress level on the PSS:NICU was 3.41±0.40, and subscales with the highest and lowest scores were Baby Appearance and Behaviour (3.91±0.39), and Sights and Sounds (2.66±0.75) respectively. No maternal or infant factors were associated with the overall PSS:NICU score. However, older mothers with higher education (r=1.37, p=0.018) had elevated Sights and Sounds scores. Female infants at an older gestational age (r=-0.33, p=0.024) were associated with lower Parental Role Alteration scores.Conclusion(s): The mean PSS:NICU score of 3.41 represents moderate to high maternal stress. While the mean score is comparable to that of high-income countries, Parental Role Alteration, which is typically the largest source of stress, was second to the Baby Appearance and Behaviour subscale. Interventions that reduce maternal stress in high-income countries may also be effective for Ugandan mothers. We suggest that efforts to reduce maternal stress begin at admission, as the median stay is only a week, and should include maternal education about typical baby appearance.
Delaney Barth - CV - LabsFinal.pdf
Figure 1: Examples of items in each PSS: NICU subscale.