Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VII
367 - Burden of Infectious Disease Outbreaks on Pediatric Emergency Department Visits in New York City
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 367
Publication Number: 367.206
Publication Number: 367.206
Yurhee Lee, New York Presbyterian Weill Medical Cornell Medical Center, New York, NY, United States; Alexandra Licona-Freudenstein, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Alan Wu, Weill Cornell Medicine, Harrisburg, NC, United States; Shravya Pant, Weill Cornell Medicine, New York, NY, United States; Zachary M. Grinspan, Weill Cornell Medicine, New York, NY, United States; Erika Abramson, Weill Cornell Medicine, New York, NY, United States; Susan Fraymovich, Weill Cornell Medicine, New York, NY, United States; Shari Platt, Weill Cornell Medicine, New York, NY, United States; Deborah A. Levine, Weill Cornell Medical College - New York, NY, Port Washington, NY, United States

Yurhee Lee, MD
Resident
New York Presbyterian Weill Medical Cornell Medical Center
New York, New York, United States
Presenting Author(s)
Background: Infectious disease outbreaks such as the current COVID-19 pandemic impact emergency department volume, hospitalizations, and critical care services for children. Understanding how this pandemic compares with prior outbreaks may provide important insights to guide future preparedness.
Objective: We compared the clinical presentation and acuity of pediatric emergency department (PED) visits during three infectious disease outbreaks: pandemic H1N1 influenza, severe seasonal influenza, and two peaks of pandemic COVID-19 in New York City (NYC).
Design/Methods: We conducted a cross-sectional study using the INSIGHT Clinical Research Network, a large multicenter database comprised from five major health systems in NYC. We included children aged 0-18 years who presented to the PED during four study periods (dates determined by NYC Department of Health data trends and study investigator consensus): pandemic H1N1 influenza (1/1/09 to 8/31/10), severe seasonal influenza (11/1/17 to 3/31/18), COVID-19 peak 1 (3/1/20 to 7/31/20), COVID-19 peak 2 (8/1/20 to 2/1/21). We compared patient demographics, clinical diagnoses, ED visit complexity (by CPT codes), and admission rates. Bivariable analyses comparing key variables across disease phases were conducted with R (version 4.0.2). P-values were generated using two-sided tests and evaluated at the alpha = 0.05 level.
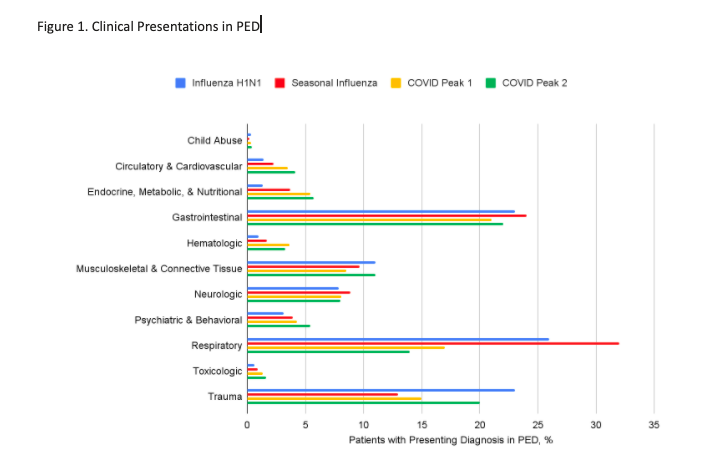
Results: We included 107,690 subjects in the H1N1 influenza group, 74,262 in the severe seasonal influenza group, 30,795 in the COVID-19 peak 1, and 39,583 in the COVID-19 peak 2 (Table 1). A wide distribution of ages was seen across all outbreaks. Respiratory illness was highest during the severe seasonal influenza period, p < 0.001 (Figure 1). Trauma-related emergencies were seen during all periods, and highest during the H1N1 influenza period, p < 0.001. The COVID-19 periods, particularly peak 2, showed the highest rates of psychiatric, toxicologic, and cardiovascular emergencies, p< 0.001. PED visits during COVID-19 resulted in greater rates of ED visit resource utilization, hospitalization, and ICU admission (Table 2).
Conclusion(s): Our study shows the breadth of different diseases and injuries during epidemics. The extensive societal disruption from COVID-19 appears to be fueling non-infectious sequelae of concern. It is important for PEDs to remain prepared for diverse medical, surgical, and psychosocial conditions in children during infectious disease outbreaks.
Table 1: Demographics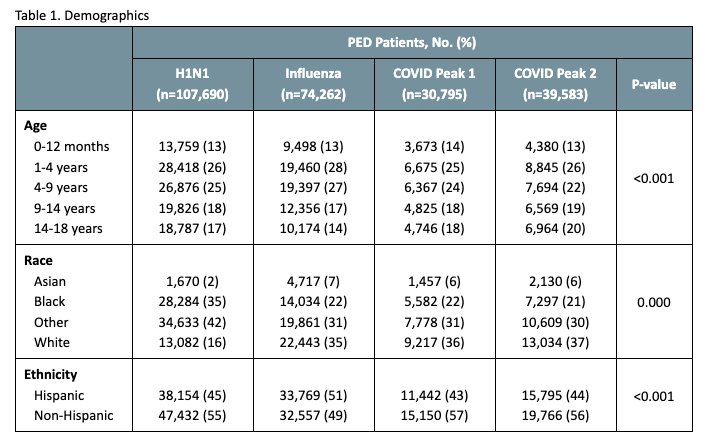 Patient level data
Patient level data
Figure 1: Clinical Presentations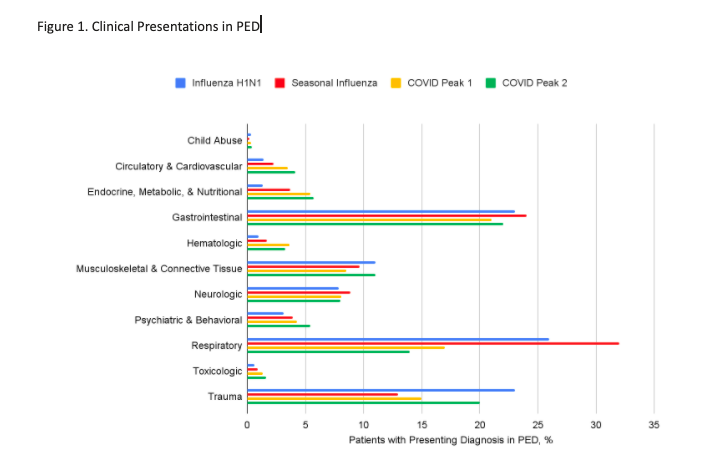
Objective: We compared the clinical presentation and acuity of pediatric emergency department (PED) visits during three infectious disease outbreaks: pandemic H1N1 influenza, severe seasonal influenza, and two peaks of pandemic COVID-19 in New York City (NYC).
Design/Methods: We conducted a cross-sectional study using the INSIGHT Clinical Research Network, a large multicenter database comprised from five major health systems in NYC. We included children aged 0-18 years who presented to the PED during four study periods (dates determined by NYC Department of Health data trends and study investigator consensus): pandemic H1N1 influenza (1/1/09 to 8/31/10), severe seasonal influenza (11/1/17 to 3/31/18), COVID-19 peak 1 (3/1/20 to 7/31/20), COVID-19 peak 2 (8/1/20 to 2/1/21). We compared patient demographics, clinical diagnoses, ED visit complexity (by CPT codes), and admission rates. Bivariable analyses comparing key variables across disease phases were conducted with R (version 4.0.2). P-values were generated using two-sided tests and evaluated at the alpha = 0.05 level.
Results: We included 107,690 subjects in the H1N1 influenza group, 74,262 in the severe seasonal influenza group, 30,795 in the COVID-19 peak 1, and 39,583 in the COVID-19 peak 2 (Table 1). A wide distribution of ages was seen across all outbreaks. Respiratory illness was highest during the severe seasonal influenza period, p < 0.001 (Figure 1). Trauma-related emergencies were seen during all periods, and highest during the H1N1 influenza period, p < 0.001. The COVID-19 periods, particularly peak 2, showed the highest rates of psychiatric, toxicologic, and cardiovascular emergencies, p< 0.001. PED visits during COVID-19 resulted in greater rates of ED visit resource utilization, hospitalization, and ICU admission (Table 2).
Conclusion(s): Our study shows the breadth of different diseases and injuries during epidemics. The extensive societal disruption from COVID-19 appears to be fueling non-infectious sequelae of concern. It is important for PEDs to remain prepared for diverse medical, surgical, and psychosocial conditions in children during infectious disease outbreaks.
Table 1: Demographics
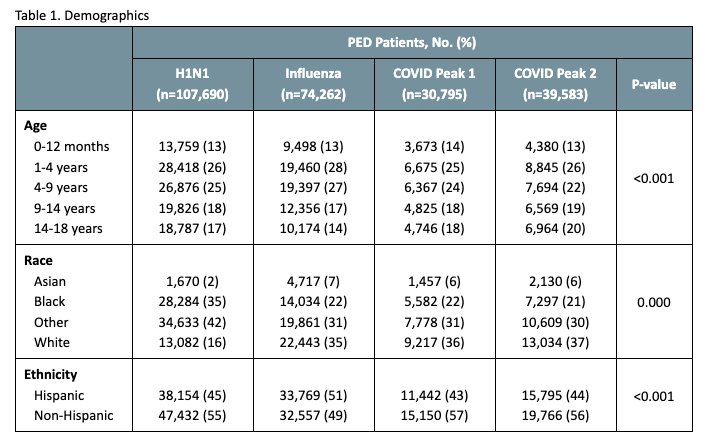 Patient level data
Patient level dataFigure 1: Clinical Presentations