Back
Asthma
Category: Abstract Submission
Pulmonology I
536 - Description of Patient Characteristics and Outcomes for Children with Asthma in Limited English Proficiency Spanish-speaking Households Using a Regional Asthma Registry
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 536
Publication Number: 536.242
Publication Number: 536.242
Hayley T. Sparks, Children's National Health System, Baltimore, MD, United States; Nikita Kachroo, Children's National Health System, Washington, DC, United States; Eduardo Fox, George Washington University School of Medicine and Health Sciences, Washington, DC, United States

Hayley T. Sparks, MD
Resident
Children's National Health System
Baltimore, Maryland, United States
Presenting Author(s)
Background: Children from Spanish-speaking families with limited English proficiency (LEP) are noted to have worse disease specific outcomes and experiences. Asthma is an ideal condition to examine how language barriers affect care given the high prevalence and complexity. The District of Columbia Pediatric Asthma Registry (Asthma Registry) offers a comprehensive survey of asthma care for this population.
Objective: De 1) Describe the population of children with asthma in DC area that reside in Spanish-speaking households with LEP2) Compare rates of ED visits and hospitalizations for children in Spanish-speaking vs English-speaking households
Design/Methods: The Asthma Registry includes all patients who have interfaced with Children’s National AND received an asthma ICD-10 code. Queried patients in the registry from 2017-2019 who met the following criteria: age 2-17 with preferred language indicated and a DC, MD, or VA address. Demographic information included asthma severity, age, and insurance type. Outcome measures were compared by language preference via ANOVA.
Results: The registry identified 88,251 patients who met inclusion criteria, with 13.4% from Spanish-speaking households. Characteristics for children from those households include: mean age 9.8 (4) years, 29.4% with persistent asthma, 26.8% prescribed controller medication, and 4.2% privately insured (Table 1). These Spanish speaking households were concentrated in northeast DC and Maryland suburbs (Figure 1). Compared to children from English-speaking households, slightly fewer children from Spanish-speaking households had at least one ED visit (17.2% vs 19%, p value < 0.001) but slightly more had at least one hospitalization (10.2% vs 8.5%, p value < 0.001) (Table 2). Children from Spanish-speaking households were less likely to have a primary care pediatrician identified than English-speaking counterparts (Table 1).Conclusion(s): The use of a regional pediatric asthma registry enables the analysis of demographic information and outcome measures for a large population of children residing in Spanish-speaking households. Previous studies have been limited to smaller populations or relied on parent surveys. This study finds differences in insurance coverage and rates of healthcare utilization for individuals when compared by language preference, even among the asthma registry’s overall population which is disproportionately nonwhite and publicly insured. Further investigation will be needed to more fully understand the interplay of race, insurance coverage, and LEP as they relate to asthma care and outcomes.
Table 1.png) Demographic information for asthma patients from English-speaking and Spanish-speaking households
Demographic information for asthma patients from English-speaking and Spanish-speaking households
Table 2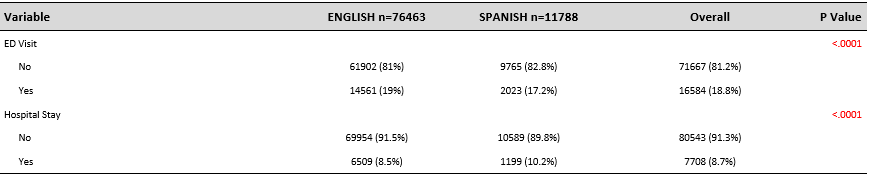 Outcomes for asthma patients from English-speaking and Spanish-speaking households
Outcomes for asthma patients from English-speaking and Spanish-speaking households
Objective: De 1) Describe the population of children with asthma in DC area that reside in Spanish-speaking households with LEP2) Compare rates of ED visits and hospitalizations for children in Spanish-speaking vs English-speaking households
Design/Methods: The Asthma Registry includes all patients who have interfaced with Children’s National AND received an asthma ICD-10 code. Queried patients in the registry from 2017-2019 who met the following criteria: age 2-17 with preferred language indicated and a DC, MD, or VA address. Demographic information included asthma severity, age, and insurance type. Outcome measures were compared by language preference via ANOVA.
Results: The registry identified 88,251 patients who met inclusion criteria, with 13.4% from Spanish-speaking households. Characteristics for children from those households include: mean age 9.8 (4) years, 29.4% with persistent asthma, 26.8% prescribed controller medication, and 4.2% privately insured (Table 1). These Spanish speaking households were concentrated in northeast DC and Maryland suburbs (Figure 1). Compared to children from English-speaking households, slightly fewer children from Spanish-speaking households had at least one ED visit (17.2% vs 19%, p value < 0.001) but slightly more had at least one hospitalization (10.2% vs 8.5%, p value < 0.001) (Table 2). Children from Spanish-speaking households were less likely to have a primary care pediatrician identified than English-speaking counterparts (Table 1).Conclusion(s): The use of a regional pediatric asthma registry enables the analysis of demographic information and outcome measures for a large population of children residing in Spanish-speaking households. Previous studies have been limited to smaller populations or relied on parent surveys. This study finds differences in insurance coverage and rates of healthcare utilization for individuals when compared by language preference, even among the asthma registry’s overall population which is disproportionately nonwhite and publicly insured. Further investigation will be needed to more fully understand the interplay of race, insurance coverage, and LEP as they relate to asthma care and outcomes.
Table 1
.png) Demographic information for asthma patients from English-speaking and Spanish-speaking households
Demographic information for asthma patients from English-speaking and Spanish-speaking householdsTable 2
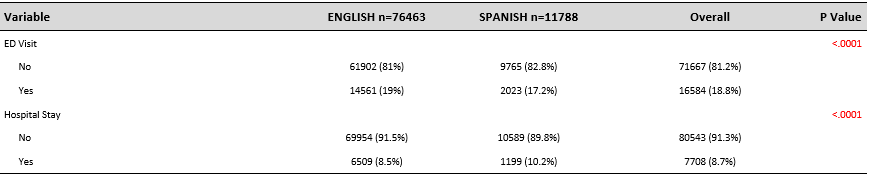 Outcomes for asthma patients from English-speaking and Spanish-speaking households
Outcomes for asthma patients from English-speaking and Spanish-speaking households