Back
Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation II
480 - Hospital and Neurodevelopmental Outcomes in Nano-Preemie Infants Receiving Invasive Vs. Non-invasive Ventilation at Birth
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 480
Publication Number: 480.231
Publication Number: 480.231
Vivek V. Shukla, University of Alabama at Birmingham, Birmingham, AL, United States; Jaclyn P. Souder, University of Colorado School of Medicine, Aurora, CO, United States; Grant Imbrock, University of Alabama, Gardendale, AL, United States; Muhan Hu, University of Alabama School of Medicine, Birmingham, AL, United States; AKM F. Rahman, University of Alabama at Birmingham, Vestavia, AL, United States; Colm P. Travers, University of Alabama at Birmingham, Birmingham, AL, United States; Namasivayam Ambalavanan, University of Alabama School of Medicine, Birmingham, AL, United States; Waldemar A. Carlo, University of Alabama at Birmingham, Birmingham, AL, United States; Charitharth Vivek Lal, University of Alabama at Birmingham, AL, Birmingham, AL, United States

Vivek Shukla, MD (he/him/his)
Assistant Professor
University of Alabama at Birmingham
Birmingham, Alabama, United States
Presenting Author(s)
Background: Infants with gestational age between 22 0/7 to 23 6/7 weeks (referred herein as nano-preemie infants) are at very high risk of adverse outcomes. Non-invasive respiratory support at birth improves outcomes in infants born at 24 0/7 to 27 6/7 weeks gestational age. There is limited evidence on whether similar benefits of non-invasive respiratory support at birth extend to nano-preemie infants.
Objective: To evaluate the hypothesis that intubation ≤10 minutes after birth is associated with a higher incidence of bronchopulmonary dysplasia (BPD) or death by 36 weeks post-menstrual age (PMA) in nano-preemie infants.
Design/Methods: Design: Observational cohort study Setting: Level IV neonatal intensive care unit at University of Alabama at Birmingham Participants: All nano-preemie infants delivered from January 2014 to June 2021 were included. Infants receiving palliative/comfort care at birth were excluded. Main Outcome(s) and Measure(s): The primary outcome was the composite outcome of BPD (physiological definition) or death by 36 weeks PMA. Infants were grouped based on intubation timing after birth ( >10 minutes and ≤10 minutes after birth, as non-invasive and invasive respiratory support at birth groups, respectively).
Results: A total of 230 consecutively born eligible nano-preemie infants were included. The incidence of BPD or death by 36 weeks PMA did not differ between non-invasive and invasive respiratory support groups (83/88 (94.3%) non-invasive versus 129/142 (90.9%) invasive; adjusted (for antenatal corticosteroids, birthweight, and gestational age, aOR=2.09, 95% CI=0.60-7.25, p-value=0.24). Severe intraventricular hemorrhage or death by 36 weeks PMA was lower in the invasive respiratory support at birth group (aOR=2.20, 95% CI=1.07-4.51, p-value=0.03). All other secondary outcomes were not significantly different.Conclusion(s): Non-invasive respiratory support in the first 10 minutes after birth is feasible but is not associated with a decrease in the risk of BPD or death compared to intubation and early surfactant in nano-preemie infants.
Table 1: Baseline Characteristics by Group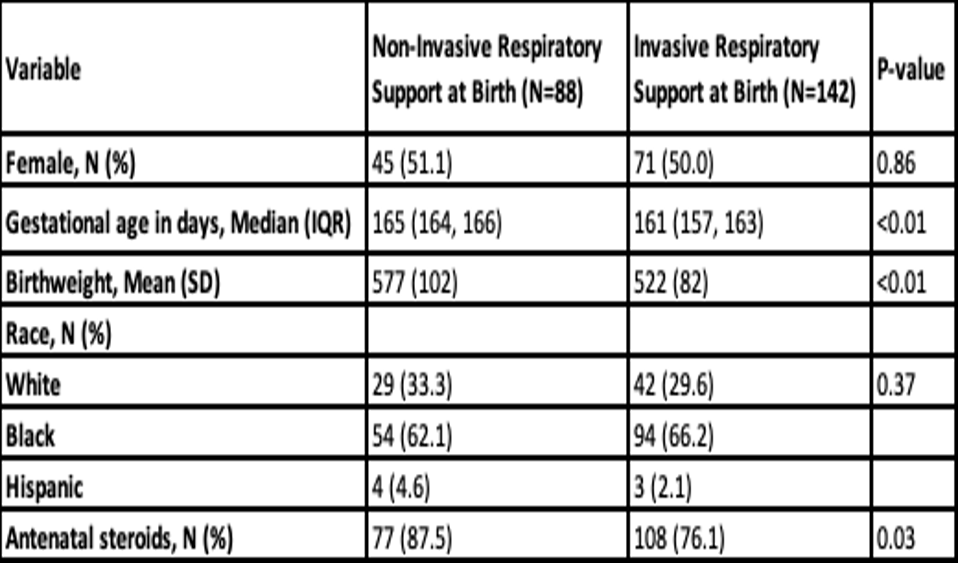
Table 2: Outcome Analyses by Group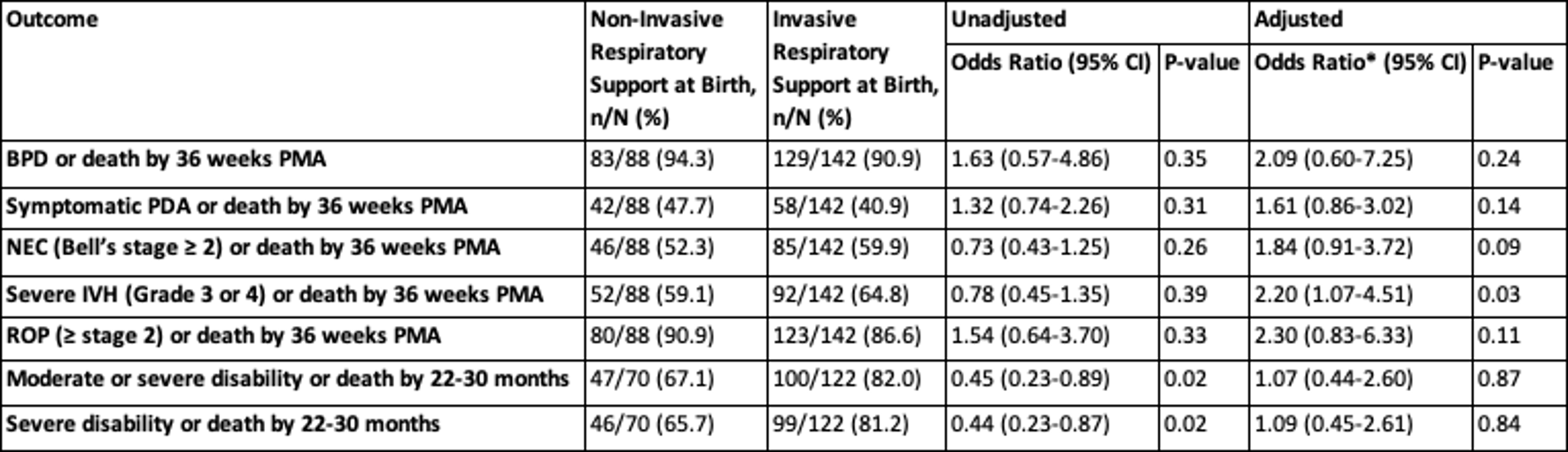 *Adjusted for antenatal corticosteroids, birth weight, gestational age by logistic regression analyses. The adjusted odds ratios represented in the table are for non-Invasive respiratory support at birth group. BPD = bronchopulmonary dysplasia, PMA = post-menstrual age, PDA = patent ductus arteriosus, NEC = necrotizing enterocolitis, IVH = intraventricular hemorrhage, ROP = retinopathy of prematurity.
*Adjusted for antenatal corticosteroids, birth weight, gestational age by logistic regression analyses. The adjusted odds ratios represented in the table are for non-Invasive respiratory support at birth group. BPD = bronchopulmonary dysplasia, PMA = post-menstrual age, PDA = patent ductus arteriosus, NEC = necrotizing enterocolitis, IVH = intraventricular hemorrhage, ROP = retinopathy of prematurity.
Objective: To evaluate the hypothesis that intubation ≤10 minutes after birth is associated with a higher incidence of bronchopulmonary dysplasia (BPD) or death by 36 weeks post-menstrual age (PMA) in nano-preemie infants.
Design/Methods: Design: Observational cohort study Setting: Level IV neonatal intensive care unit at University of Alabama at Birmingham Participants: All nano-preemie infants delivered from January 2014 to June 2021 were included. Infants receiving palliative/comfort care at birth were excluded. Main Outcome(s) and Measure(s): The primary outcome was the composite outcome of BPD (physiological definition) or death by 36 weeks PMA. Infants were grouped based on intubation timing after birth ( >10 minutes and ≤10 minutes after birth, as non-invasive and invasive respiratory support at birth groups, respectively).
Results: A total of 230 consecutively born eligible nano-preemie infants were included. The incidence of BPD or death by 36 weeks PMA did not differ between non-invasive and invasive respiratory support groups (83/88 (94.3%) non-invasive versus 129/142 (90.9%) invasive; adjusted (for antenatal corticosteroids, birthweight, and gestational age, aOR=2.09, 95% CI=0.60-7.25, p-value=0.24). Severe intraventricular hemorrhage or death by 36 weeks PMA was lower in the invasive respiratory support at birth group (aOR=2.20, 95% CI=1.07-4.51, p-value=0.03). All other secondary outcomes were not significantly different.Conclusion(s): Non-invasive respiratory support in the first 10 minutes after birth is feasible but is not associated with a decrease in the risk of BPD or death compared to intubation and early surfactant in nano-preemie infants.
Table 1: Baseline Characteristics by Group
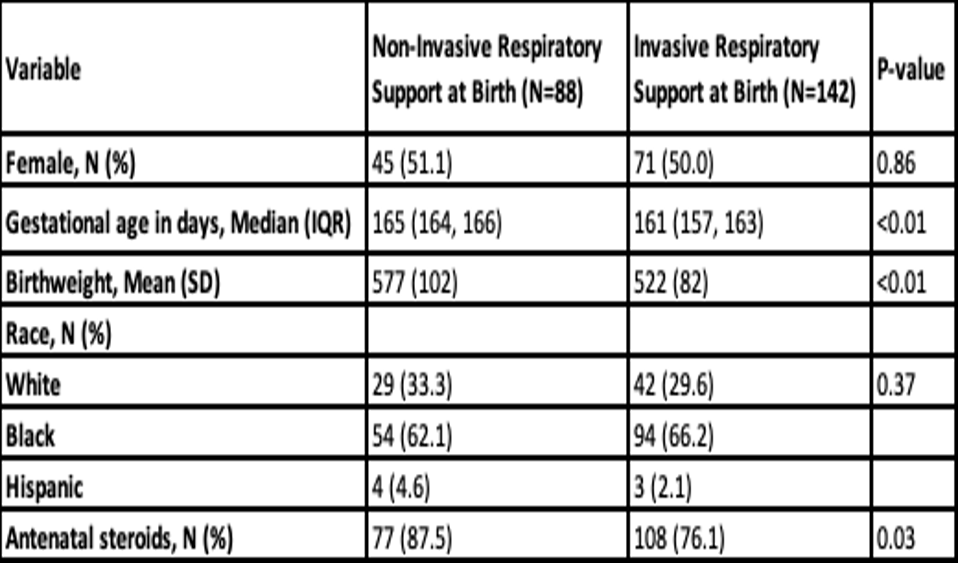
Table 2: Outcome Analyses by Group
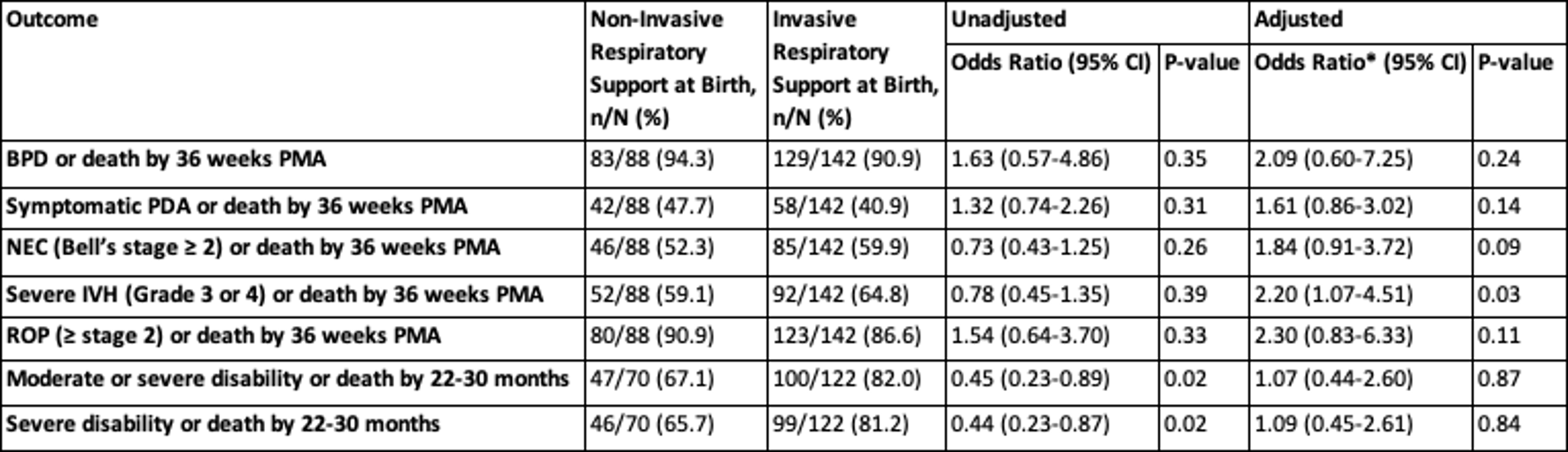 *Adjusted for antenatal corticosteroids, birth weight, gestational age by logistic regression analyses. The adjusted odds ratios represented in the table are for non-Invasive respiratory support at birth group. BPD = bronchopulmonary dysplasia, PMA = post-menstrual age, PDA = patent ductus arteriosus, NEC = necrotizing enterocolitis, IVH = intraventricular hemorrhage, ROP = retinopathy of prematurity.
*Adjusted for antenatal corticosteroids, birth weight, gestational age by logistic regression analyses. The adjusted odds ratios represented in the table are for non-Invasive respiratory support at birth group. BPD = bronchopulmonary dysplasia, PMA = post-menstrual age, PDA = patent ductus arteriosus, NEC = necrotizing enterocolitis, IVH = intraventricular hemorrhage, ROP = retinopathy of prematurity.