Obesity
Category: Abstract Submission
Obesity II
526 - Impact of pandemic related weight gain on youth with presumed NAFLD
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 526
Publication Number: 526.239
Publication Number: 526.239
Rusha Lev, Denver Health, Golden, CO, United States; jeanelle Sheeder, University of Colorado School of Medicine, aurora, CO, United States; Melissa Wong, University of Colorado, Denver, CO, United States; Kathy Love-Osborne, University of Colorado School of Medicine, Denver, CO, United States

Rusha Lev, MD, FAAP
Assistant Professor
Denver Health
Golden, Colorado, United States
Presenting Author(s)
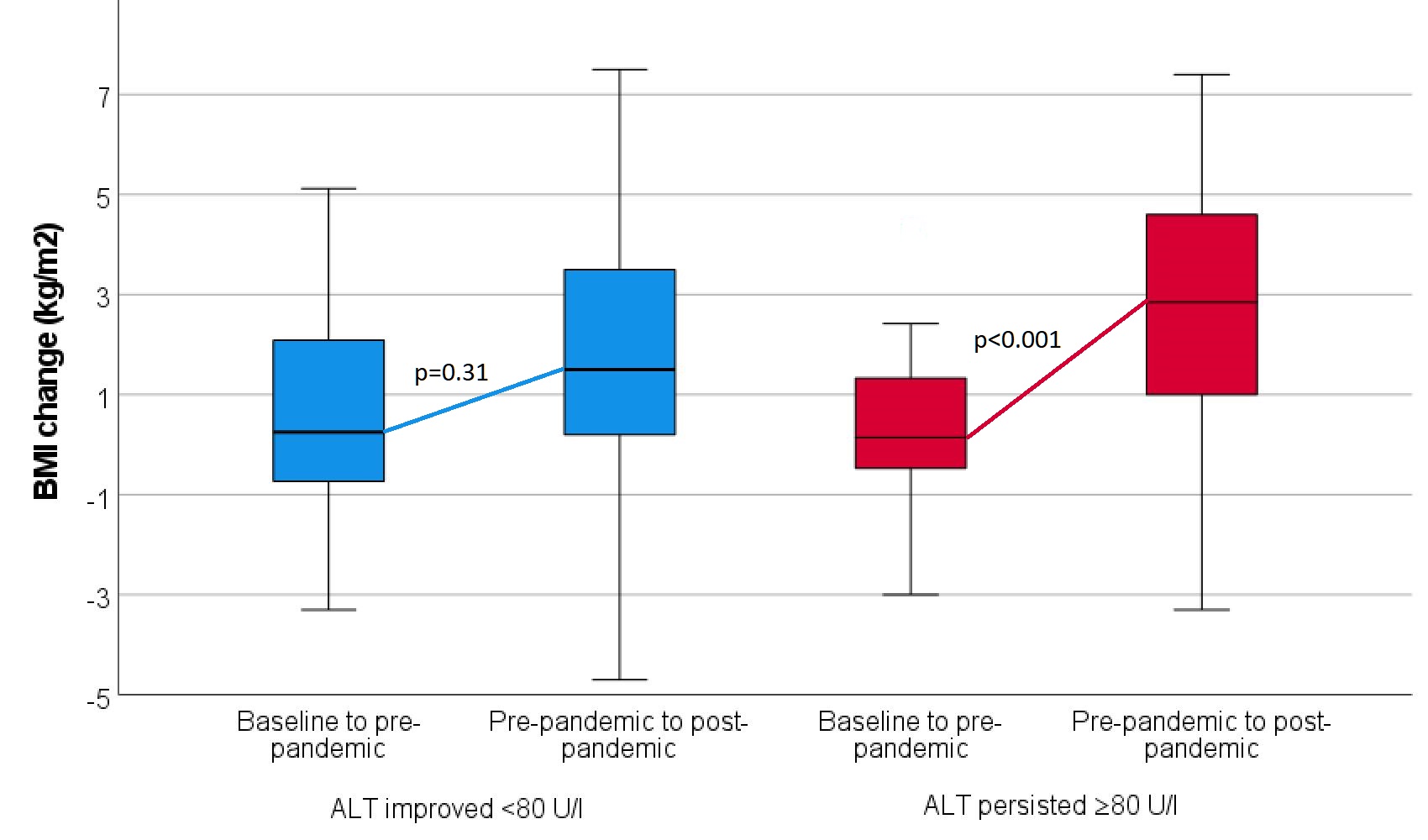
Background: Non-alcoholic fatty liver disease (NAFLD) is associated with obesity and is the leading cause of liver transplant in adults. Persistent elevation of ALT ( >80 U/l for more than 6 months) is associated with increased risk of fibrosis. Previous QI work at our institution showed youth with persistent ALT elevation increased BMI more than youth with improved ALT. Pediatric clinicians have observed BMI increases during the COVID pandemic.
Objective: <11. To evaluate BMI trajectory before and during the COVID 19 pandemic
< !2. To determine if participating in Lifestyle Medicine visits reduced BMI increase and improved ALT outcomes.
Hypothesis:
< !1. Youth identified with elevated ALT pre-pandemic will have increased BMI trajectory during the pandemic
< !2. Youth participating in lifestyle medicine visits will have less BMI increase than those without
Design/Methods: Denver Health is an integrated healthcare system; including 4 pediatric, 6 Family Medicine, and 16 School-based health clinics. Multidisciplinary lifestyle medicine clinics are located at 8 sites. During the pandemic visits were conducted by telephone.
98% of patients are below 200% of the Federal Poverty level and 87% publicly insured or uninsured
Methods:
Participants: 165 youth ages 9-18 with initial ALT ≥80 U/L between 5/18-9/19. Chart review was performed and symptomatic youth or those with other primary diagnoses were excluded.
Results: 93 youth had BMI and ALT measured at baseline (pre-pandemic) and at least one point after the onset of the COVID 19 pandemic in March 2020, with mean follow up of 24 months from first to last ALT. 69 (74%) male, 90 (97%) Hispanic. Median age 12.8 yo (range 7-18). 41 youth improved their ALT to ≤ 80. 50 youth (30% of the original 165 youth) have not been seen in person since the beginning of the pandemic. Table 1 compares youth that improved ALT < 80 U/l with youth that did not. Figure 1 shows the increased BMI trajectory in youth who persisted with elevated ALT. Conclusion(s): Youth with persistent ALT elevation had more pandemic weight gain than those who decreased ALT to < 80 U/l. Many youth in both groups participated in lifestyle medicine visits pre-pandemic, with less participating during the pandemic. It is possible that youth with persistently elevated ALT were more likely to be referred to lifestyle medicine during the pandemic. Effectiveness of lifestyle medicine visits by telephone deserves further study. Of concern, almost a third of this cohort of high-risk youth have not had an in person visit since the beginning of the COVID-19 pandemic.
Table 1: BMI changes and lifestyle visits for youth with and without improved ALT.png)
Figure 1:: BMI trajectory pre- and post-pandemic in youth who improved ALT vs those who did not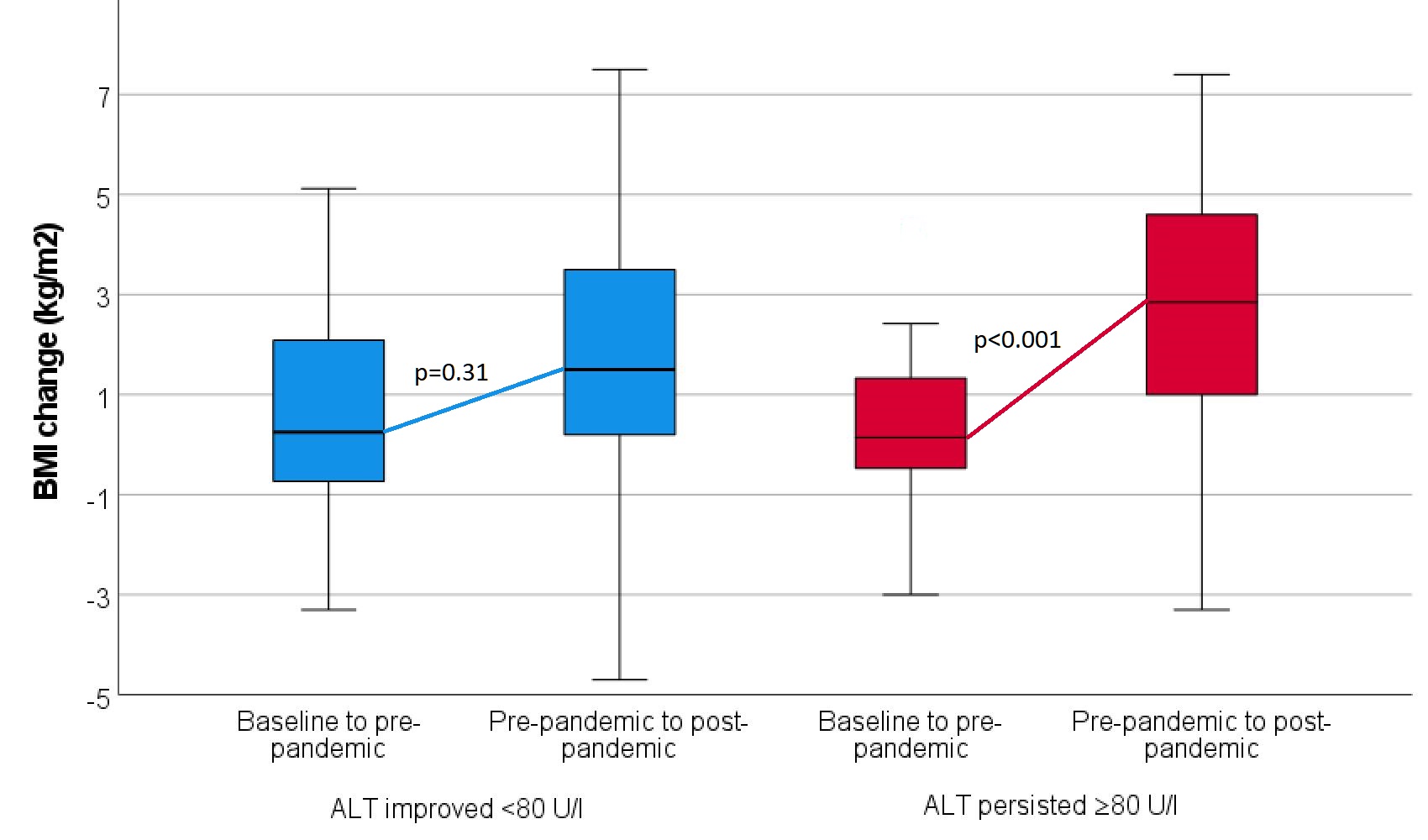
Objective: <11. To evaluate BMI trajectory before and during the COVID 19 pandemic
< !2. To determine if participating in Lifestyle Medicine visits reduced BMI increase and improved ALT outcomes.
Hypothesis:
< !1. Youth identified with elevated ALT pre-pandemic will have increased BMI trajectory during the pandemic
< !2. Youth participating in lifestyle medicine visits will have less BMI increase than those without
Design/Methods: Denver Health is an integrated healthcare system; including 4 pediatric, 6 Family Medicine, and 16 School-based health clinics. Multidisciplinary lifestyle medicine clinics are located at 8 sites. During the pandemic visits were conducted by telephone.
98% of patients are below 200% of the Federal Poverty level and 87% publicly insured or uninsured
Methods:
Participants: 165 youth ages 9-18 with initial ALT ≥80 U/L between 5/18-9/19. Chart review was performed and symptomatic youth or those with other primary diagnoses were excluded.
Results: 93 youth had BMI and ALT measured at baseline (pre-pandemic) and at least one point after the onset of the COVID 19 pandemic in March 2020, with mean follow up of 24 months from first to last ALT. 69 (74%) male, 90 (97%) Hispanic. Median age 12.8 yo (range 7-18). 41 youth improved their ALT to ≤ 80. 50 youth (30% of the original 165 youth) have not been seen in person since the beginning of the pandemic. Table 1 compares youth that improved ALT < 80 U/l with youth that did not. Figure 1 shows the increased BMI trajectory in youth who persisted with elevated ALT. Conclusion(s): Youth with persistent ALT elevation had more pandemic weight gain than those who decreased ALT to < 80 U/l. Many youth in both groups participated in lifestyle medicine visits pre-pandemic, with less participating during the pandemic. It is possible that youth with persistently elevated ALT were more likely to be referred to lifestyle medicine during the pandemic. Effectiveness of lifestyle medicine visits by telephone deserves further study. Of concern, almost a third of this cohort of high-risk youth have not had an in person visit since the beginning of the COVID-19 pandemic.
Table 1: BMI changes and lifestyle visits for youth with and without improved ALT
.png)
Figure 1:: BMI trajectory pre- and post-pandemic in youth who improved ALT vs those who did not