Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up III
268 - Long Term Outcome of Necrotizing Enterocolitis and Spontaneous Intestinal Perforation at 10 and 15 years
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 268
Publication Number: 268.225
Publication Number: 268.225
Ruben Vaidya, Baystate Children's Hospital, Springfield, MA, United States; Joe X. Yi, University of North Carolina at Chapel Hill School of Medicine, Cary, NC, United States; Michael O’Shea, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Elizabeth T. Jensen, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Robert Joseph, Boston University, Boston, MA, United States; Semsa Gogcu, Wake Forest Baptist Health - Brenner Children's Hospital, Winston Salem, NC, United States; Kathryn Wagner, Baystate Children's Hospital, Granville,, MA, United States; Jeffrey S. Shenberger, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Michael E. Msal, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Amanda Thompson, UNC Chapel Hill, Chapel Hill, NC, United States; Jean A. Frazier, University of Massachusetts Medical School, Worcester, MA, United States; Rachana Singh, Tufts Childrens Hospital, Boston, MA, United States

Ruben Vaidya, MD
Associate Professor of Pediatrics
UMass Chan Medical School- Baystate
East Longmeadow, Massachusetts, United States
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) and spontaneous intestinal perforation (SIP) are common gastrointestinal complications in preterm infants associated with high degree of morbidity, mortality, impaired neurodevelopmental (ND) and growth outcomes. No study has reported growth or ND outcomes in infants with NEC/SIP beyond early childhood.
Objective: The objective of the study was to compare growth and ND outcome at 10 and 15 years follow-up in school-aged children born extremely preterm who developed NEC or SIP during their NICU stay with gestational age matched controls without NEC nor SIP.
Design/Methods: Participants were identified from an ongoing multicenter prospective longitudinal study of Extremely Low Gestational Age Newborns (ELGAN Study), born between 2002 and 2004, and followed up at age 10 and 15 years. Participants were categorized into 4 groups based on diagnoses made during their NICU hospitalization: medical NEC, surgical NEC, SIP and no NEC/SIP. At follow up visits height, weight and head circumference (HC) were measured. Comprehensive neurobehavioral assessments (ADHD, gross motor, Epilepsy), and standardized tests of intelligence and executive function (EF) were administered. Results from these tests were used to generate latent profiles using IQ and EF measures at age 10 and included neuropsychological measures in addition to EF at age 15. Both crude and adjusted models were used to evaluate associations, adjusting for weight z-score, gestational age, sex as possible confounders.
Results: Of 1222 infants who survived until discharge, 889 (72.2%) were evaluated at 10 years and 694 (56.8%) were evaluated at 15 years [Table 1]. Children with medical NEC had similar weight, body mass index (BMI), height and HC compared to controls at both 10 and 15 years. At 15 years, children with surgical NEC had lower weight z-scores (adjusted effect estimate: -0.78, p=0.003), lower BMI (adjusted effect estimate: -0.54, p=0.05), and lower height z-scores (adjusted effect estimate: -0.73, p=0.005). Children with SIP had lower weight z-score (effect estimate: -0.70, p=0.03) and lower height z-score (effect estimate: -0.65, p=0.003) at age 10 years. There were no differences between the neurodevelopmental outcomes in children who had medical NEC, surgical NEC or SIP when compared to children with no NEC/SIP [Table 2, 3].Conclusion(s): Growth impairment associated with surgical NEC and SIP may persist through late childhood. ND outcomes among school-aged children born extremely preterm with any NEC or SIP were no different from children with no NEC or SIP.
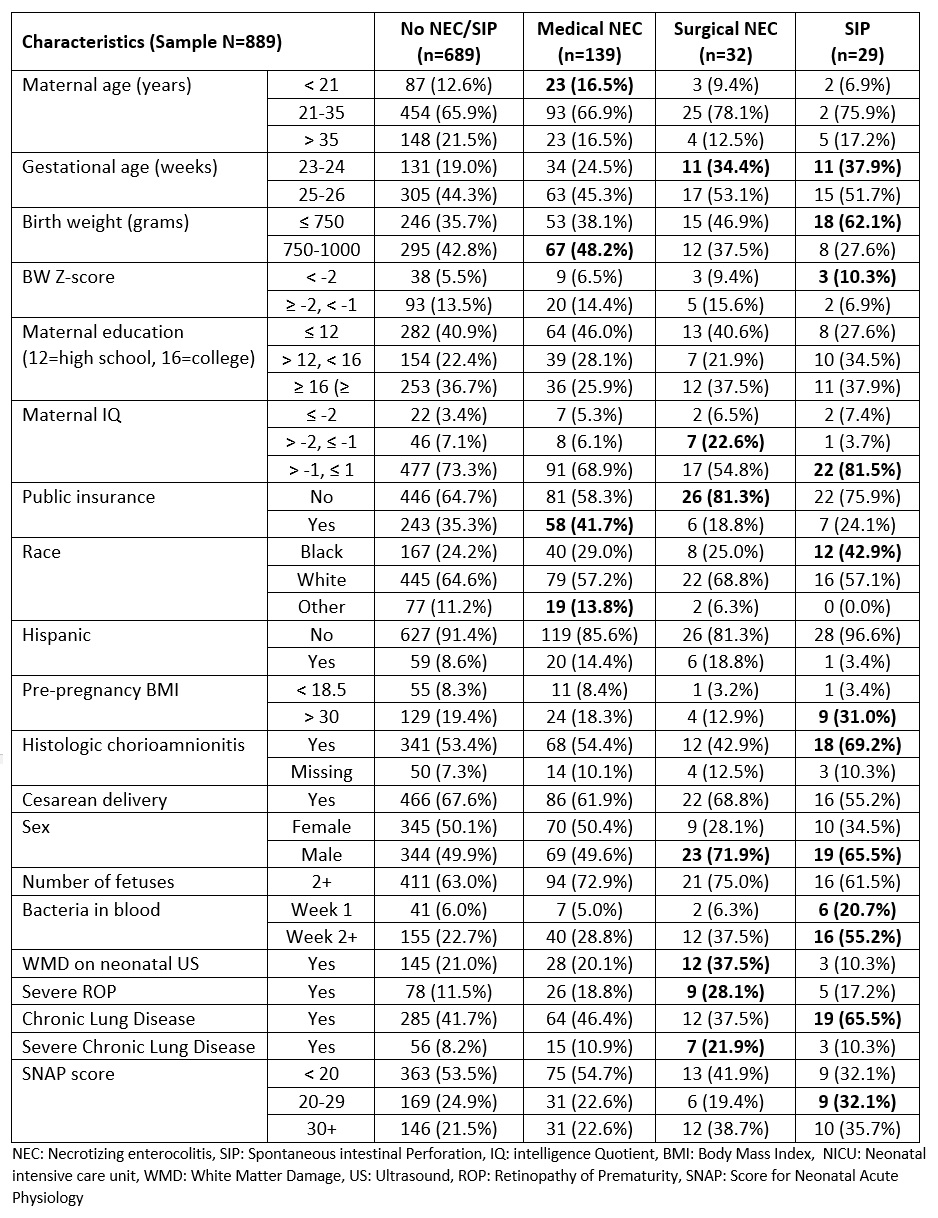
Baseline Demographic Characteristics of the Study Cohorts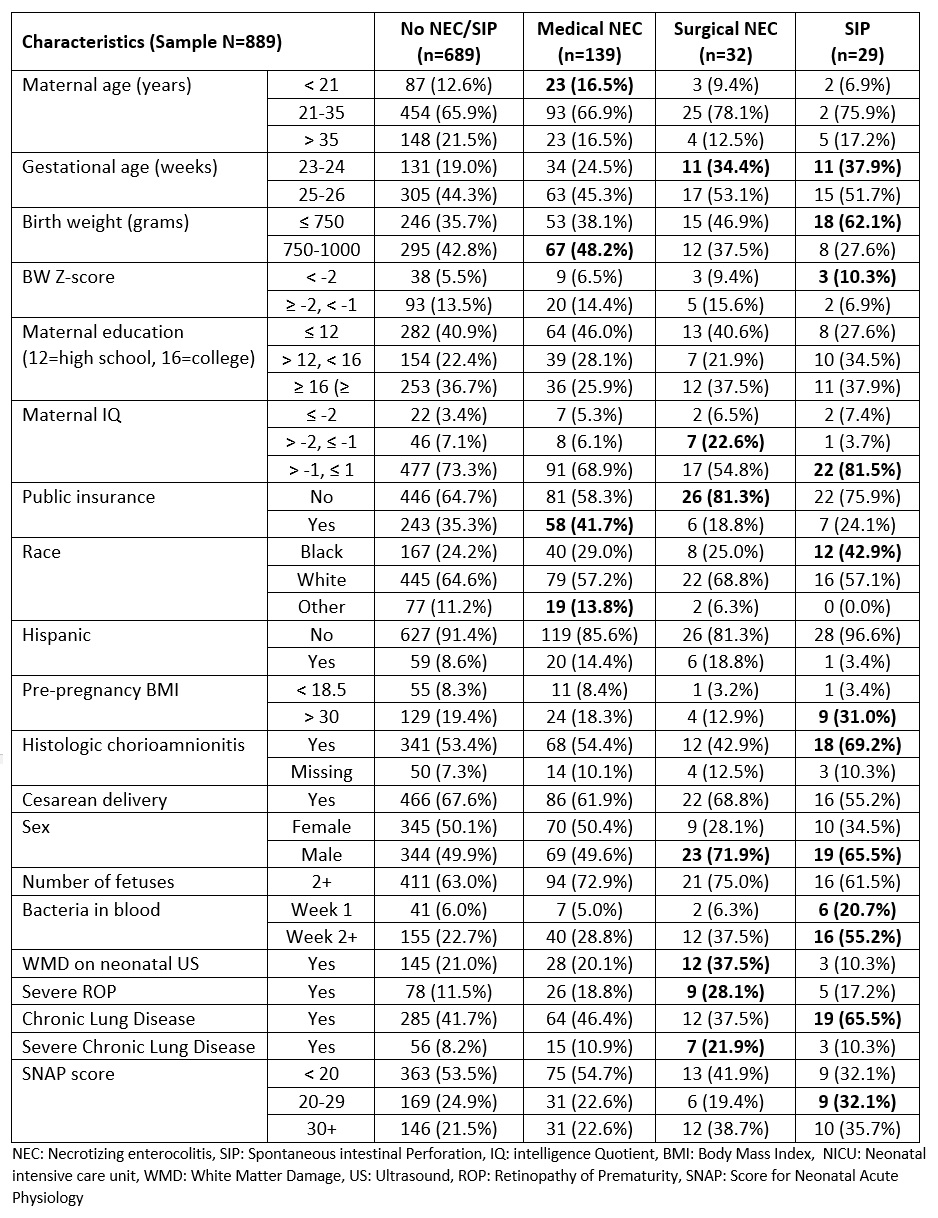
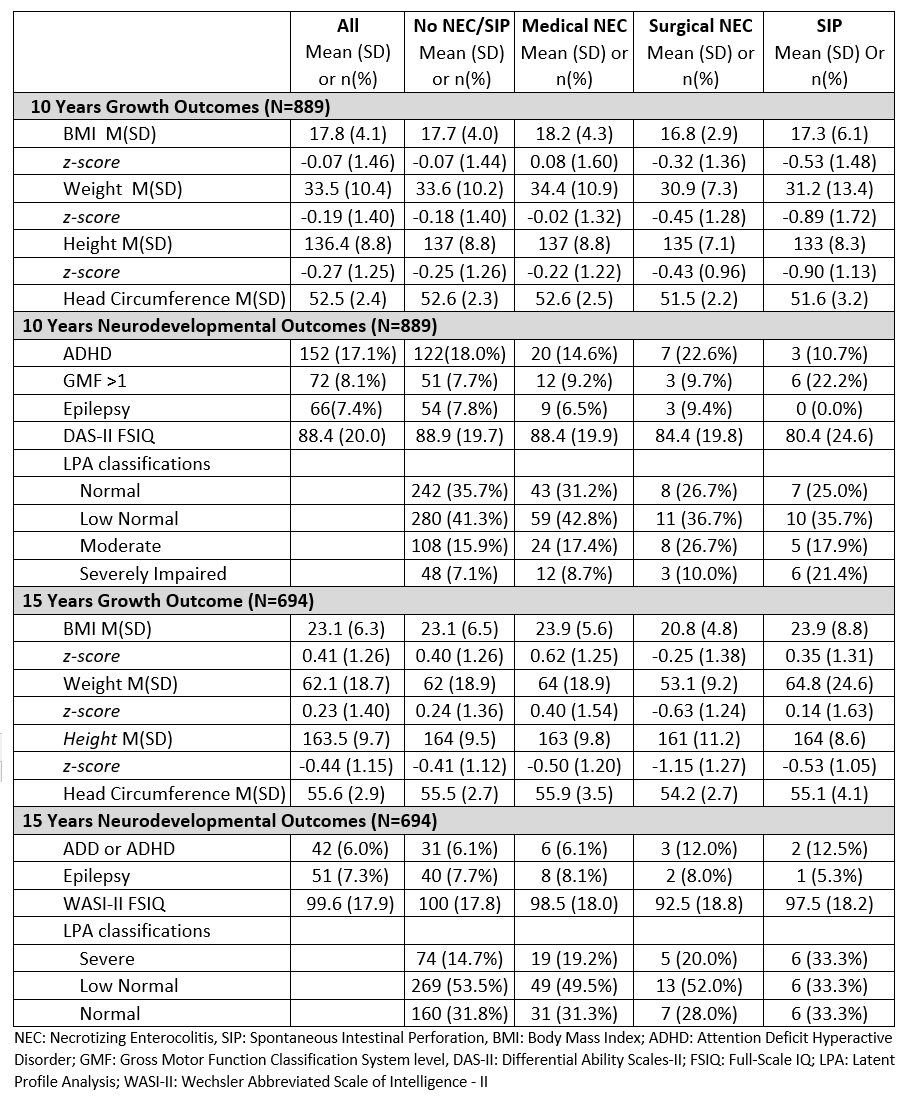
10- and 15-Year Growth and Neurodevelopmental Outcomes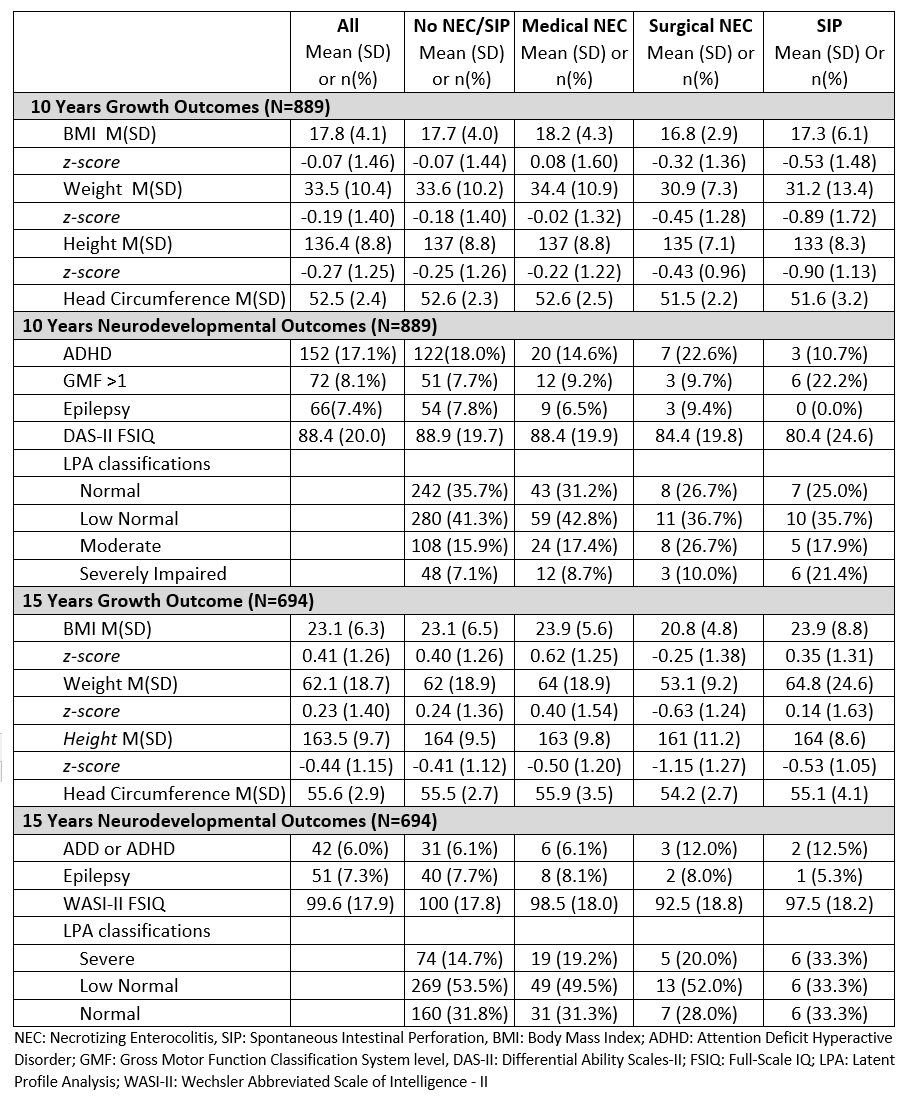
Objective: The objective of the study was to compare growth and ND outcome at 10 and 15 years follow-up in school-aged children born extremely preterm who developed NEC or SIP during their NICU stay with gestational age matched controls without NEC nor SIP.
Design/Methods: Participants were identified from an ongoing multicenter prospective longitudinal study of Extremely Low Gestational Age Newborns (ELGAN Study), born between 2002 and 2004, and followed up at age 10 and 15 years. Participants were categorized into 4 groups based on diagnoses made during their NICU hospitalization: medical NEC, surgical NEC, SIP and no NEC/SIP. At follow up visits height, weight and head circumference (HC) were measured. Comprehensive neurobehavioral assessments (ADHD, gross motor, Epilepsy), and standardized tests of intelligence and executive function (EF) were administered. Results from these tests were used to generate latent profiles using IQ and EF measures at age 10 and included neuropsychological measures in addition to EF at age 15. Both crude and adjusted models were used to evaluate associations, adjusting for weight z-score, gestational age, sex as possible confounders.
Results: Of 1222 infants who survived until discharge, 889 (72.2%) were evaluated at 10 years and 694 (56.8%) were evaluated at 15 years [Table 1]. Children with medical NEC had similar weight, body mass index (BMI), height and HC compared to controls at both 10 and 15 years. At 15 years, children with surgical NEC had lower weight z-scores (adjusted effect estimate: -0.78, p=0.003), lower BMI (adjusted effect estimate: -0.54, p=0.05), and lower height z-scores (adjusted effect estimate: -0.73, p=0.005). Children with SIP had lower weight z-score (effect estimate: -0.70, p=0.03) and lower height z-score (effect estimate: -0.65, p=0.003) at age 10 years. There were no differences between the neurodevelopmental outcomes in children who had medical NEC, surgical NEC or SIP when compared to children with no NEC/SIP [Table 2, 3].Conclusion(s): Growth impairment associated with surgical NEC and SIP may persist through late childhood. ND outcomes among school-aged children born extremely preterm with any NEC or SIP were no different from children with no NEC or SIP.
Baseline Demographic Characteristics of the Study Cohorts
10- and 15-Year Growth and Neurodevelopmental Outcomes