Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation III
495 - Management and outcomes of extremely preterm neonates born at 22 weeks: a single-center experience in Japan
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 495
Publication Number: 495.232
Publication Number: 495.232
Yukiko Motojima, Saitama Medical Center, Saitama Medical University, Kawagoeshi, Saitama, Japan; Eri Nishimura, Saitama Medical Center, Kawagoe, Saitama, Japan; Masayo Kanai, Saitama Medical Center, Kawagoe, Saitama, Japan; Akio Ishiguro, Saitama Medical Center, Saitama Medical University, Kawagoe, Saitama, Japan; Kazuhiko Kabe, Saitama Medical Univ. Saitama Medical Center, Kawagoe City, Saitama, Japan; Fumihiko Namba, Saitama Medical Center, Saitama Medical University, Kawagoe, Saitama, Japan
- YM
Yukiko Motojima
Assistant professor
Saitama Medical Center, Saitama Medical University
Kawagoeshi, Saitama, Japan
Presenting Author(s)
Background: Most international guidelines for resuscitation decisions of extremely preterm infants support comfort care only at 22 weeks of gestation and active care at 25 weeks. However, in Japan, active resuscitation of infants born at 22 weeks has been performed in ~80% of neonatal intensive care units (NICUs).
Objective: To review the management, mortality, and morbidities of infants born at 22 weeks during the last 8 years in our NICU.
Design/Methods: A retrospective observational study was conducted for reviewing maternal information, birth status, resuscitation methods, and posthospitalization management for infants born between 22 weeks 0 days and 22 weeks 6 days of gestation who were admitted to our NICU from 2013 to 2020.
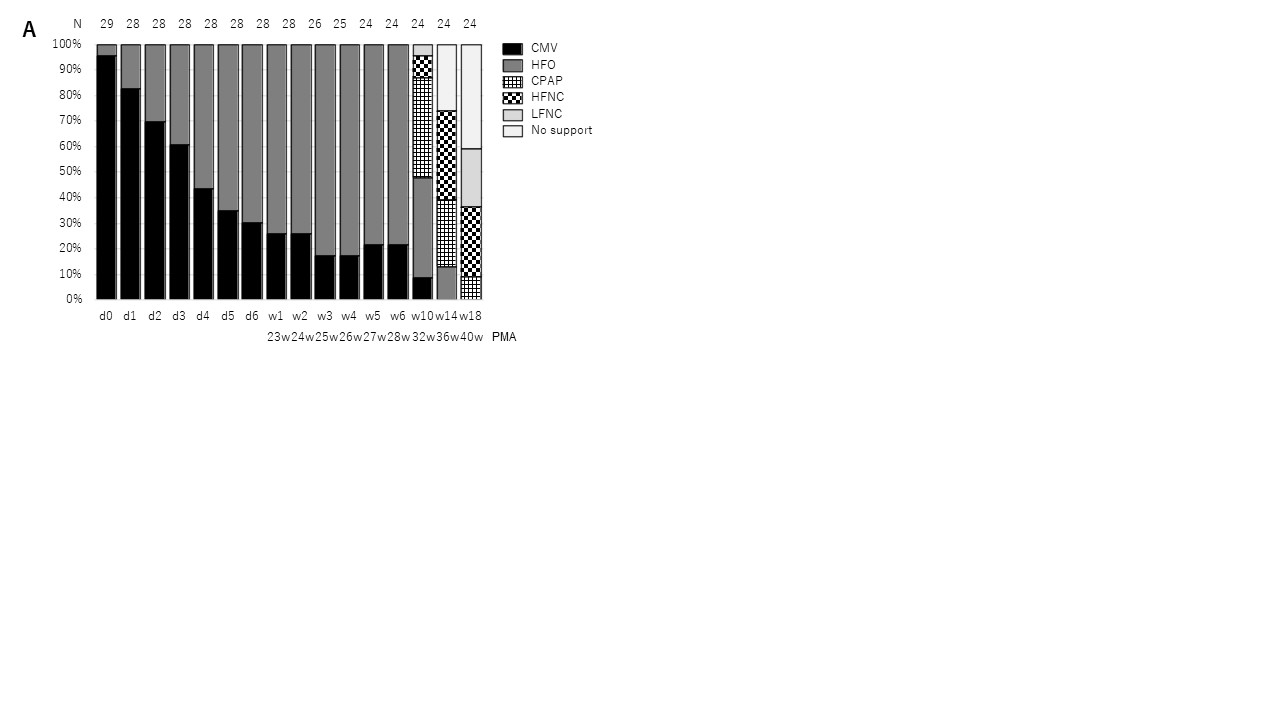
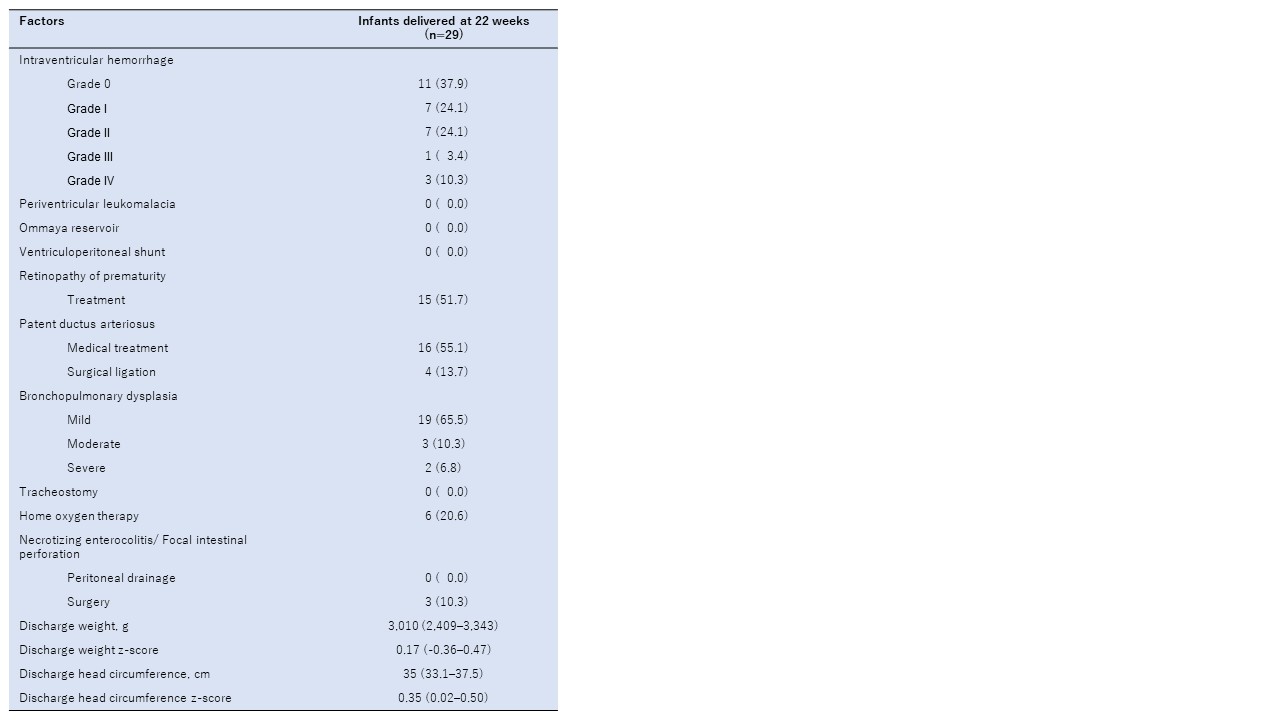
Results: Twenty-nine infants born at 22 weeks were actively resuscitated, and the survival rate was 82.8% (24/29). Five infants (17.2%) died of sepsis within the first month of life. In the delivery room, tracheal intubation was required in all patients, and surfactant replacement therapy was performed for 27 (93.1%) of them. Umbilical catheters in 24 (82.8%) patients and peripherally inserted central catheters in 5 (7.2%) patients were inserted as intravenous lines, whereas umbilical catheters in 27 (93.1%) patients and peripheral arterial lines in 2 (6.9%) patients were inserted as arterial lines. All patients received prophylactic antibiotics. For respiratory management, conventional mechanical ventilation was initially introduced in 27 (93.1%) patients on day 0, and this mode was changed to high-frequency oscillatory ventilation in more than half (62%) of the patients by day 4. The setting of incubator temperature and humidity was initially 39°C and 90%–95% and they gradually dropped to 37.3°C and 81.5% by day 7, respectively. In ~90% of cases, phenobarbital was used for sedation (when necessary) within 5 days after birth. In terms of morbidities, surgical treatment of patent ductus arteriosus, necrotizing enterocolitis, and retinopathy of prematurity were required in 4 (13.7%), 3 (10.3%), and 15 (51.7%) cases, respectively. Six (20.6%) patients required home oxygen therapy, no patient required tracheostomy, four (13.7%) patients had severe intraventricular hemorrhage, and no patient required a ventriculoperitoneal shunt.Conclusion(s): Among infants born at 22 weeks, the overall survival rate and the rate of survival without moderate or severe morbidities were significantly higher than those reported in other countries. Since this was a single-center experience, further studies are needed to clarify whether these managements are optimal for caring for these periviable infants.
Short-term outcomes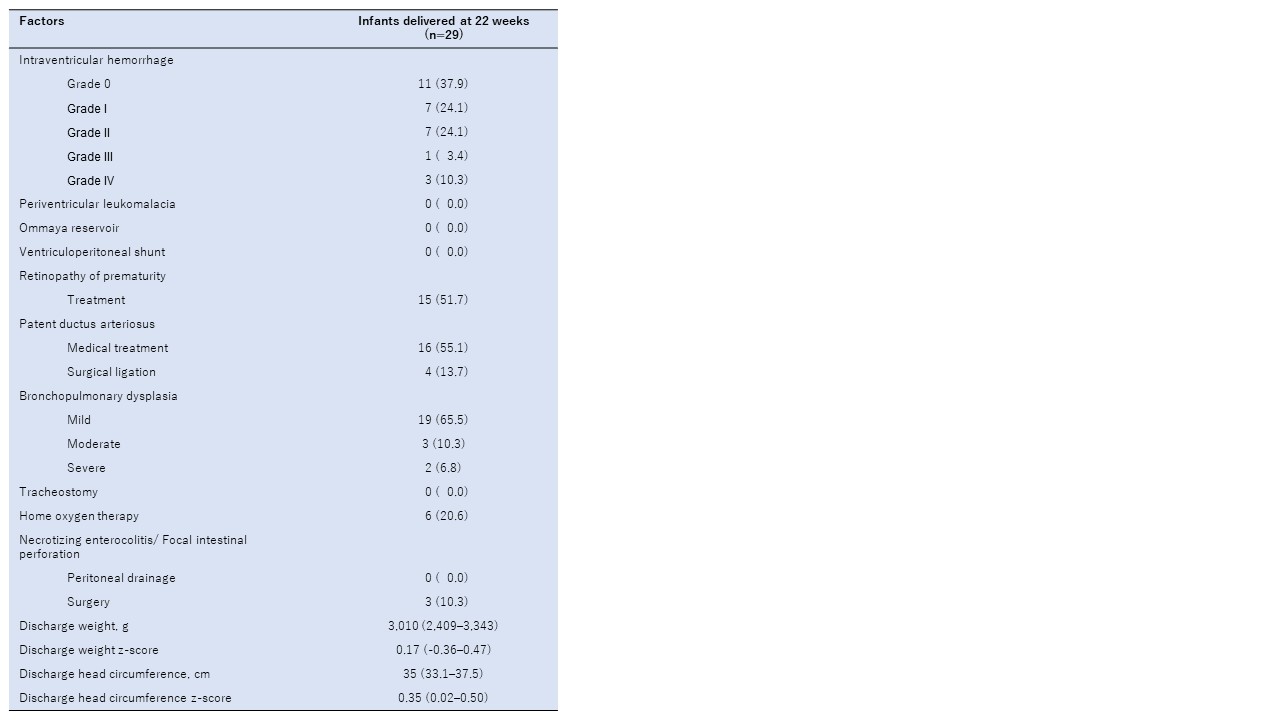
Respiratory Management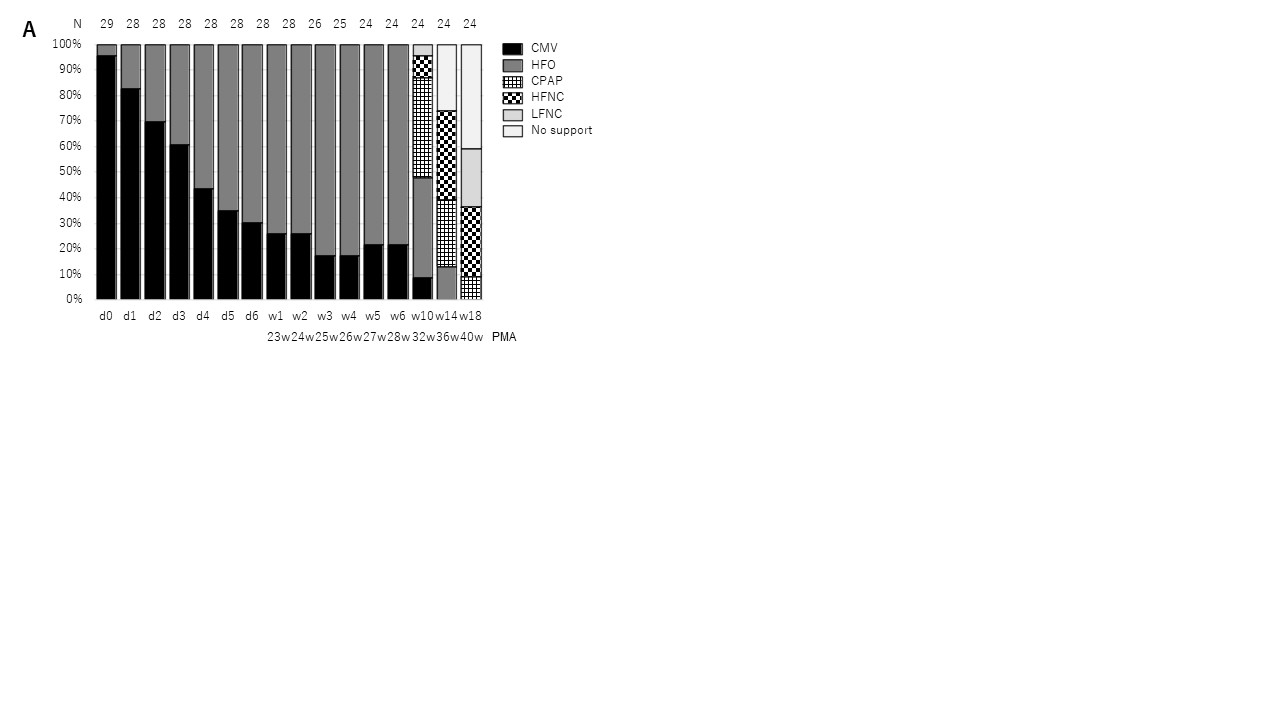
Objective: To review the management, mortality, and morbidities of infants born at 22 weeks during the last 8 years in our NICU.
Design/Methods: A retrospective observational study was conducted for reviewing maternal information, birth status, resuscitation methods, and posthospitalization management for infants born between 22 weeks 0 days and 22 weeks 6 days of gestation who were admitted to our NICU from 2013 to 2020.
Results: Twenty-nine infants born at 22 weeks were actively resuscitated, and the survival rate was 82.8% (24/29). Five infants (17.2%) died of sepsis within the first month of life. In the delivery room, tracheal intubation was required in all patients, and surfactant replacement therapy was performed for 27 (93.1%) of them. Umbilical catheters in 24 (82.8%) patients and peripherally inserted central catheters in 5 (7.2%) patients were inserted as intravenous lines, whereas umbilical catheters in 27 (93.1%) patients and peripheral arterial lines in 2 (6.9%) patients were inserted as arterial lines. All patients received prophylactic antibiotics. For respiratory management, conventional mechanical ventilation was initially introduced in 27 (93.1%) patients on day 0, and this mode was changed to high-frequency oscillatory ventilation in more than half (62%) of the patients by day 4. The setting of incubator temperature and humidity was initially 39°C and 90%–95% and they gradually dropped to 37.3°C and 81.5% by day 7, respectively. In ~90% of cases, phenobarbital was used for sedation (when necessary) within 5 days after birth. In terms of morbidities, surgical treatment of patent ductus arteriosus, necrotizing enterocolitis, and retinopathy of prematurity were required in 4 (13.7%), 3 (10.3%), and 15 (51.7%) cases, respectively. Six (20.6%) patients required home oxygen therapy, no patient required tracheostomy, four (13.7%) patients had severe intraventricular hemorrhage, and no patient required a ventriculoperitoneal shunt.Conclusion(s): Among infants born at 22 weeks, the overall survival rate and the rate of survival without moderate or severe morbidities were significantly higher than those reported in other countries. Since this was a single-center experience, further studies are needed to clarify whether these managements are optimal for caring for these periviable infants.
Short-term outcomes
Respiratory Management