Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up II
256 - NICU Nights and Back to Sleep: An Examination of NICU Graduate Sleep Environments for Safe Sleep
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 256
Publication Number: 256.224
Publication Number: 256.224
Jamie P. Sklar, Cohen Children's Medical Center, Lake Success, NY, United States; Duy Q. Pham, Cohen Children's Medical Center, New York, NY, United States; Ruth Milanaik, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Great Neck, NY, United States

Jamie P. Sklar, MD
Fellow in Developmental and Behavioral Pediatrics
Cohen Children's Medical Center
Lake Success, New York, United States
Presenting Author(s)
Background: The Back to Sleep campaign provides AAP supported sleep safety guidelines for infants < 1 year to prevent Sudden Unexpected Infant Death (SUID). Monitored NICU babies often sleep prone and with items in the sleep area, contrary to home guidelines. Babies discharged from the NICU care are at higher SUID risk.
Objective: To help guide NICU practice/discharge education by determining if demographic factors and observation of NICU conditions not consistent with Back to Sleep increase the risk of unsafe home sleep practices.
Design/Methods: Original surveys were emailed to parents of infants < 13 months after NICU discharge. 400 parents responded, 225 completed the survey. Only singleton children were included. Data included demographics, parent-observed NICU sleep environment(SE), and parent-reported home SE. 𝝌2 analyses were used to determine differences in sleep practices between various demographic groups. Logistic regression was used to analyze likelihood of unsafe sleeping practices at home
Results: The sample included 212 respondents; median infant age =8.2 months.
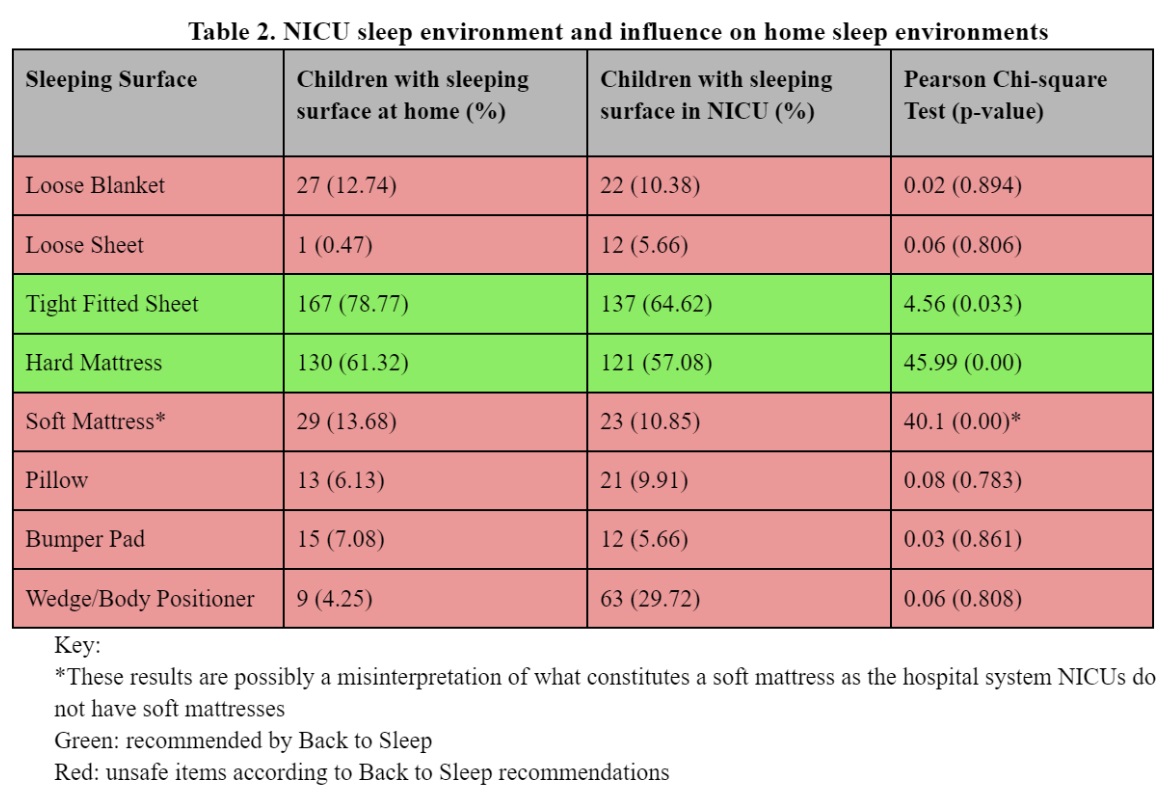
NICU exposure to non-recommended conditions did not influence home SEs for loose blankets/sheets, pillows, bumpers, or positioners(p >0.05). Sleep position (SP) in the NICU was not a factor for increased risk of unsafe SP (Table 2).
Overall, at home, 43 respondents (20%) indicated unsafe SPs and 116 (55%) had unsafe sleep items.
Placement of babies in unsafe SPs was influenced by race(𝝌2=18.76, p< 0.01), household income(𝝌2=23.83, p< 0.01), and highest level of parental education(𝝌2=19.15, p< 0.01). Black and Asian babies were at increased risk. Lower income and those who did not complete college were at higher risk.
Cosleeping was influenced by race(𝝌2=21.39, p< 0.01), but not by household income(𝝌2=4.36, p=0.49) or highest level of parental education(𝝌2=8.84, p=0.06)(Table 1). Black and Asian babies were at increased risk.
Over 88% of parents using unsafe SPs had been educated on safe sleep practices in the NICU and/or by their pediatrician, as were over 90% of parents using unsafe sleep locations.Conclusion(s): NICU SE exposures that were not compliant with Back to Sleep guidelines did not influence the likelihood of unsafe home sleep conditions. Despite receiving safe sleep guidance, the majority of respondents reported unsafe home sleep practices. Black or Asian race, lower income, and lower education level increased the risk of unsafe sleep practices.
Safe sleep education was common, but ineffective; it is essential that all families understand sleep safety prior to NICU discharge and it be reinforced at all well visits.
Table 1. Demographics and home sleep conditions.jpg)
Table 2. NICU sleep environment and influence on home sleep environments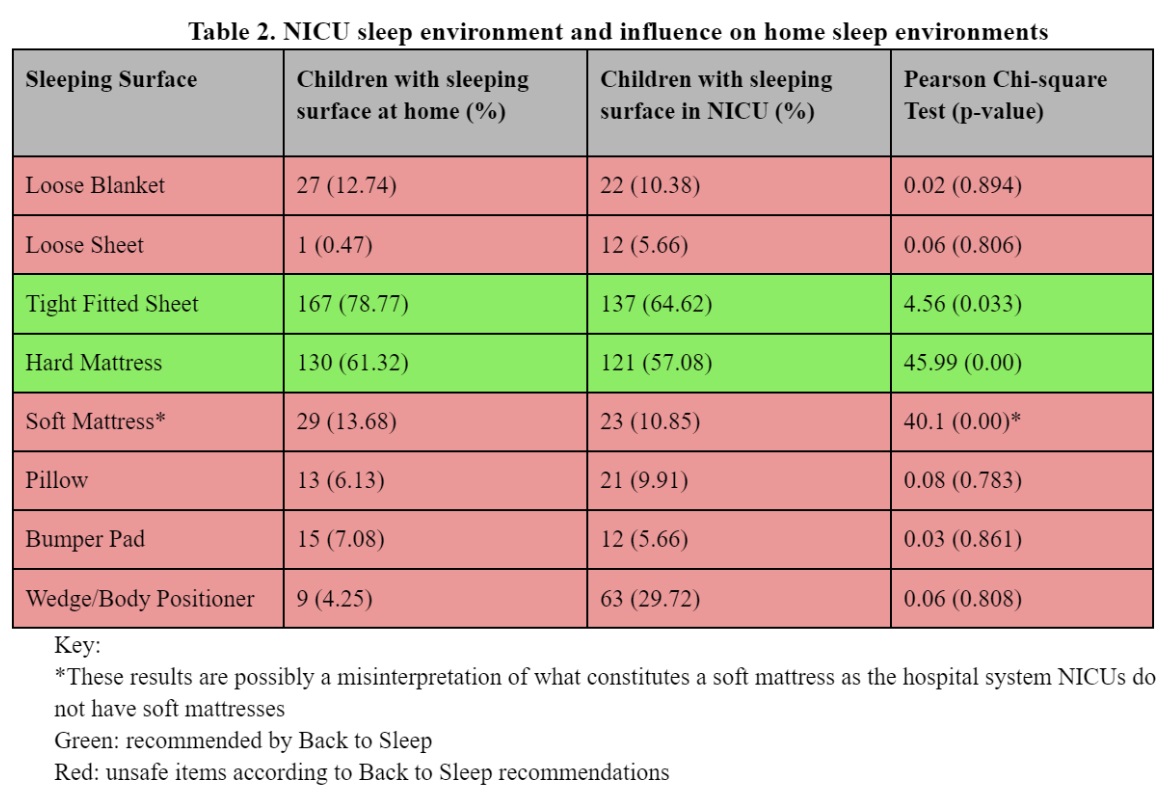
Objective: To help guide NICU practice/discharge education by determining if demographic factors and observation of NICU conditions not consistent with Back to Sleep increase the risk of unsafe home sleep practices.
Design/Methods: Original surveys were emailed to parents of infants < 13 months after NICU discharge. 400 parents responded, 225 completed the survey. Only singleton children were included. Data included demographics, parent-observed NICU sleep environment(SE), and parent-reported home SE. 𝝌2 analyses were used to determine differences in sleep practices between various demographic groups. Logistic regression was used to analyze likelihood of unsafe sleeping practices at home
Results: The sample included 212 respondents; median infant age =8.2 months.
NICU exposure to non-recommended conditions did not influence home SEs for loose blankets/sheets, pillows, bumpers, or positioners(p >0.05). Sleep position (SP) in the NICU was not a factor for increased risk of unsafe SP (Table 2).
Overall, at home, 43 respondents (20%) indicated unsafe SPs and 116 (55%) had unsafe sleep items.
Placement of babies in unsafe SPs was influenced by race(𝝌2=18.76, p< 0.01), household income(𝝌2=23.83, p< 0.01), and highest level of parental education(𝝌2=19.15, p< 0.01). Black and Asian babies were at increased risk. Lower income and those who did not complete college were at higher risk.
Cosleeping was influenced by race(𝝌2=21.39, p< 0.01), but not by household income(𝝌2=4.36, p=0.49) or highest level of parental education(𝝌2=8.84, p=0.06)(Table 1). Black and Asian babies were at increased risk.
Over 88% of parents using unsafe SPs had been educated on safe sleep practices in the NICU and/or by their pediatrician, as were over 90% of parents using unsafe sleep locations.Conclusion(s): NICU SE exposures that were not compliant with Back to Sleep guidelines did not influence the likelihood of unsafe home sleep conditions. Despite receiving safe sleep guidance, the majority of respondents reported unsafe home sleep practices. Black or Asian race, lower income, and lower education level increased the risk of unsafe sleep practices.
Safe sleep education was common, but ineffective; it is essential that all families understand sleep safety prior to NICU discharge and it be reinforced at all well visits.
Table 1. Demographics and home sleep conditions
.jpg)
Table 2. NICU sleep environment and influence on home sleep environments