Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation III
498 - The Effect of In Situ Simulation on Clinical Outcomes in Preterm Neonates
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 498
Publication Number: 498.232
Publication Number: 498.232
Ritu Chitkara, Stanford University, Menlo Park, CA, United States; Mihoko Bennett, Stanford University, Palo Alto, CA, United States; Janine Bohnert, Stanford University, Stanford, CA, United States; Nicole K. Yamada, Stanford University School of Medicine, Palo Alto, CA, United States; Janene Fuerch, Stanford University School of Medicine, Palo Alto, CA, United States; Louis P. Halamek, Stanford University, Palo Alto, CA, United States; Jenny Quinn, Neonatal Quality Improvement Performance, Martinez, CA, United States; Kimber Padua, Stanford University School of Medicine, San Mateo, CA, United States; Jeffrey B. Gould, Stanford University Medical School, Berkeley, CA, United States; Jochen Profit, Stanford University, Palo Alto, CA, United States; Xiao Xu, Yale University, New Haven, CT, United States; Henry Lee, Stanford University, Stanford, CA, United States

Ritu Chitkara, MD
Clinical Associate Professor of Pediatrics; Neonatology
Stanford University
Menlo Park, California, United States
Presenting Author(s)
Background: Neonatal resuscitation is a high acuity event that is often required following the birth of preterm infants. Simulation in neonatal resuscitation has been shown to improve teamwork and increase efficiency of resuscitation. It is unclear, however, if a concerted program of simulation and debriefing leads to improved clinical outcomes.
Objective: To evaluate the impact of a multi-hospital collaborative quality improvement project implementing in situ simulation training for neonatal resuscitation, Simulating Success, on survival without bronchopulmonary dysplasia (BPD) for preterm infants.
Design/Methods: Fourteen neonatal intensive care units (NICUs) were enrolled into the study and divided into 4 cohorts. Each center completed a 15-month long program, including 3 months of preparatory training followed by 12 months of running simulations and debriefings. Simulating Success was conducted as a stepped wedge trial whereby each hospital served as its own control. NICU data from California Perinatal Quality Care Collaborative to evaluate the impact of the program on clinical outcomes. Very low birthweight (VLBW) infants born between 22-29 weeks without major congenital anomalies who survived greater than 12 hours were included. Primary outcome was survival without BPD; secondary measures included the effect of in situ simulation on intubation in the delivery room (DR), CPAP in the DR, hypothermia ( < 36C) upon NICU admission, severe intraventricular hemorrhage, mortality prior to hospital discharge. The intervention effect was examined based on statistical process control charts.
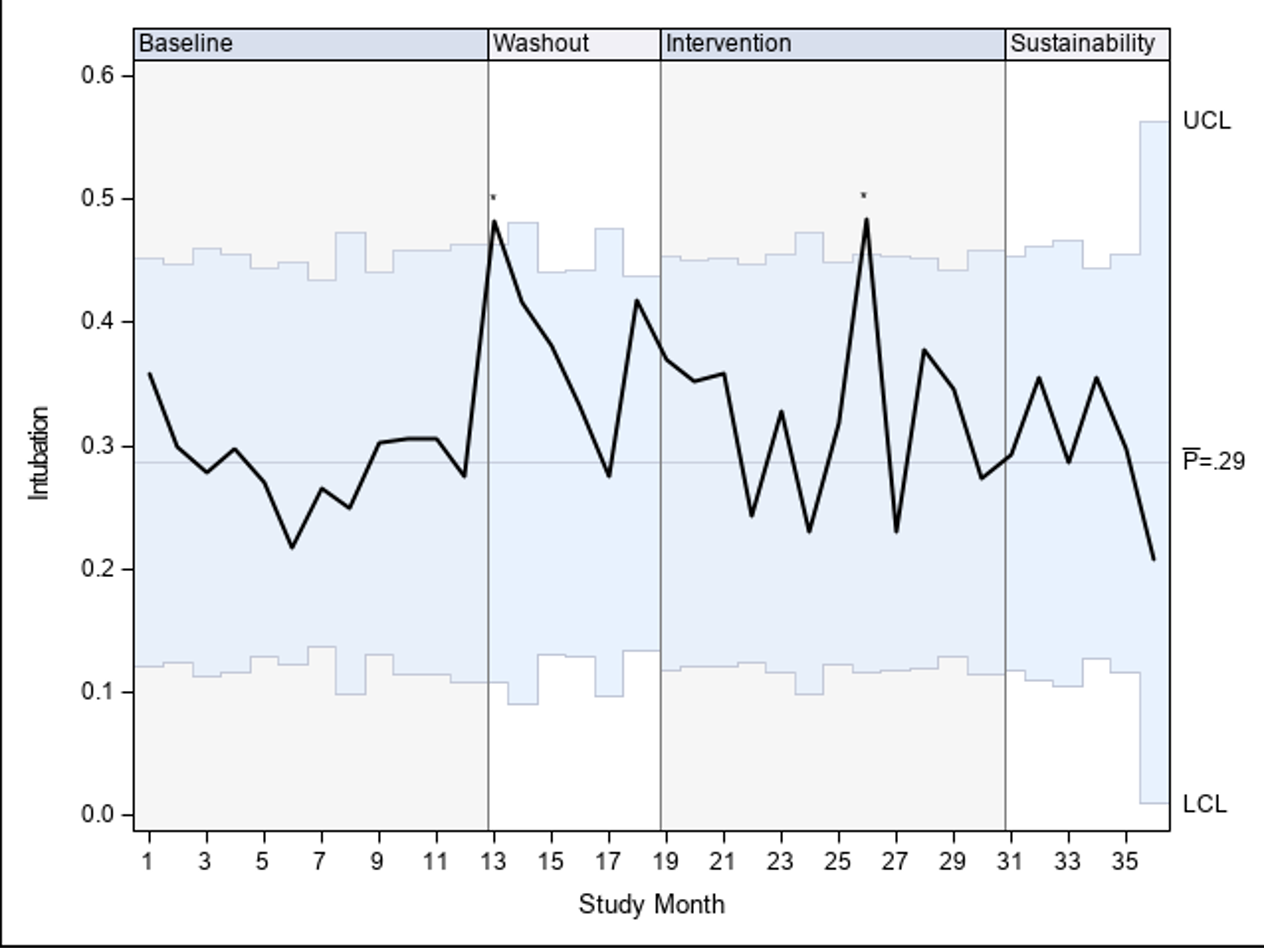
Results: A total of 1,961 VLBW births occurred between the 12 months prior to training (baseline) through 6 months after completion of training among participating centers. The rate of survival without BPD slightly decreased from 78.7% (95% CI: 75.9%-81.6%) at baseline to 76.2% (95% CI: 73.8%-78.7%) after the intervention (RR 0.97 (0.92, 1.02)); no significant improvement occurred. [Figure 1] The rate of intubation in the DR increased from 28.6% to 32.8% (RR 1.15 (1.01-1.28)), and special cause variation above the upper control limit was observed during the intervention period. [Figure 2] All other secondary outcomes were stable.Conclusion(s): Implementation of a multi-hospital collaborative providing in situ training for neonatal resuscitation did not result in significant improvement in survival without BPD. While this work may not have immediately translatable findings, ongoing in situ simulations may have impact on unit practice and unmeasured outcomes.
Figure 1. Rate of Survival without BPD for centers participating in Simulating Success.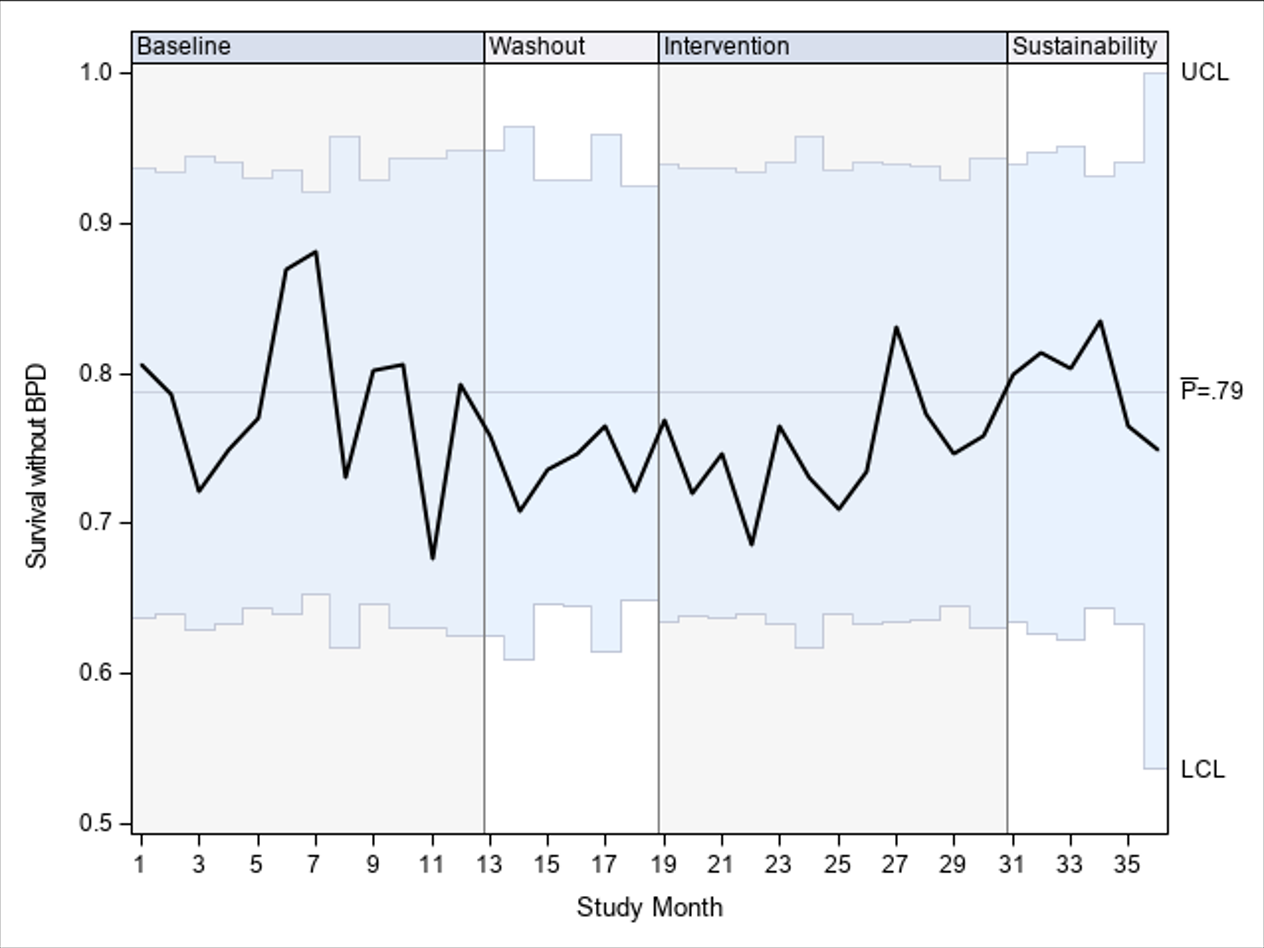
Figure 2. Rate of intubation in the delivery room for centers participating in Simulating Success.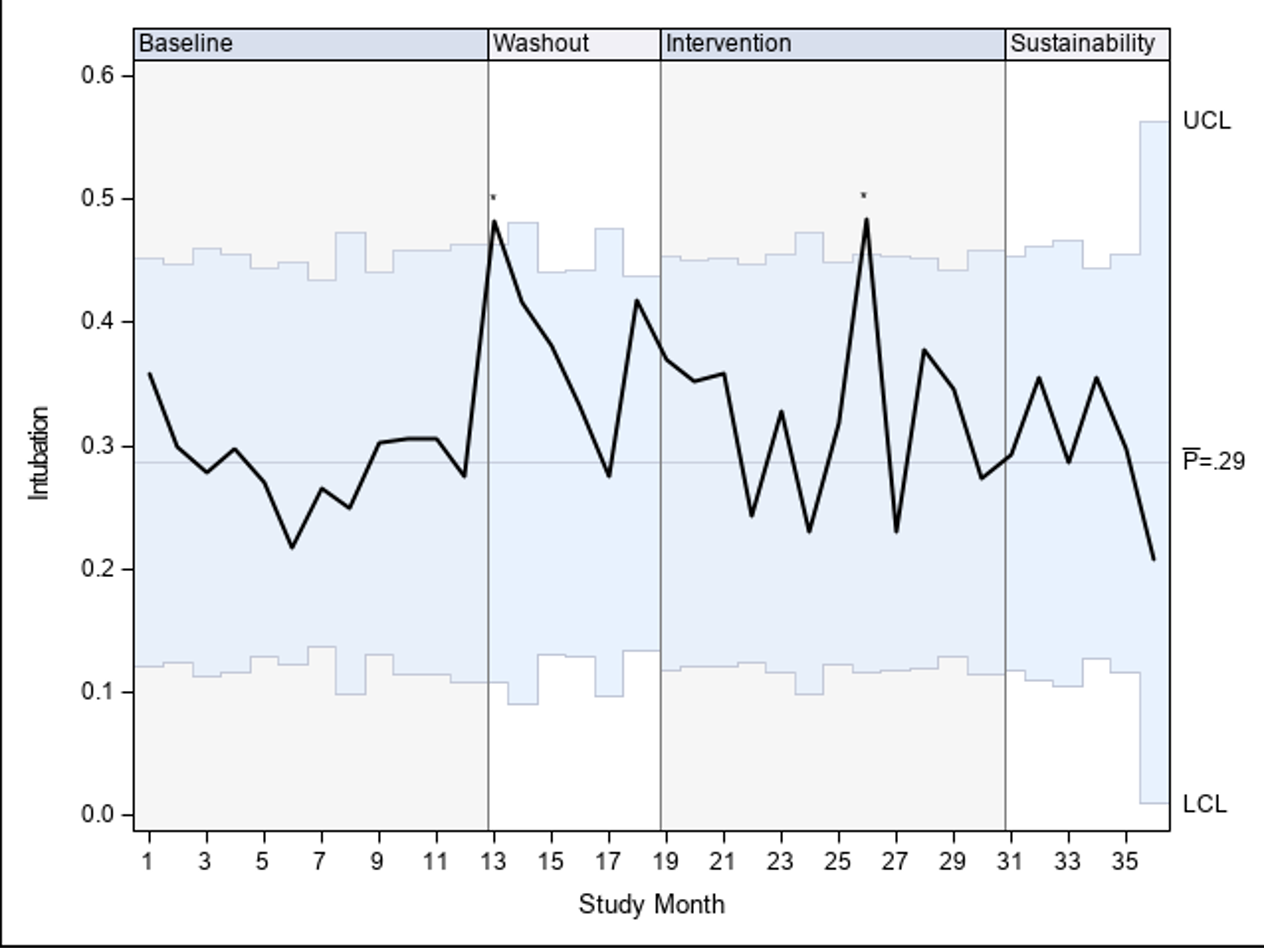
Objective: To evaluate the impact of a multi-hospital collaborative quality improvement project implementing in situ simulation training for neonatal resuscitation, Simulating Success, on survival without bronchopulmonary dysplasia (BPD) for preterm infants.
Design/Methods: Fourteen neonatal intensive care units (NICUs) were enrolled into the study and divided into 4 cohorts. Each center completed a 15-month long program, including 3 months of preparatory training followed by 12 months of running simulations and debriefings. Simulating Success was conducted as a stepped wedge trial whereby each hospital served as its own control. NICU data from California Perinatal Quality Care Collaborative to evaluate the impact of the program on clinical outcomes. Very low birthweight (VLBW) infants born between 22-29 weeks without major congenital anomalies who survived greater than 12 hours were included. Primary outcome was survival without BPD; secondary measures included the effect of in situ simulation on intubation in the delivery room (DR), CPAP in the DR, hypothermia ( < 36C) upon NICU admission, severe intraventricular hemorrhage, mortality prior to hospital discharge. The intervention effect was examined based on statistical process control charts.
Results: A total of 1,961 VLBW births occurred between the 12 months prior to training (baseline) through 6 months after completion of training among participating centers. The rate of survival without BPD slightly decreased from 78.7% (95% CI: 75.9%-81.6%) at baseline to 76.2% (95% CI: 73.8%-78.7%) after the intervention (RR 0.97 (0.92, 1.02)); no significant improvement occurred. [Figure 1] The rate of intubation in the DR increased from 28.6% to 32.8% (RR 1.15 (1.01-1.28)), and special cause variation above the upper control limit was observed during the intervention period. [Figure 2] All other secondary outcomes were stable.Conclusion(s): Implementation of a multi-hospital collaborative providing in situ training for neonatal resuscitation did not result in significant improvement in survival without BPD. While this work may not have immediately translatable findings, ongoing in situ simulations may have impact on unit practice and unmeasured outcomes.
Figure 1. Rate of Survival without BPD for centers participating in Simulating Success.
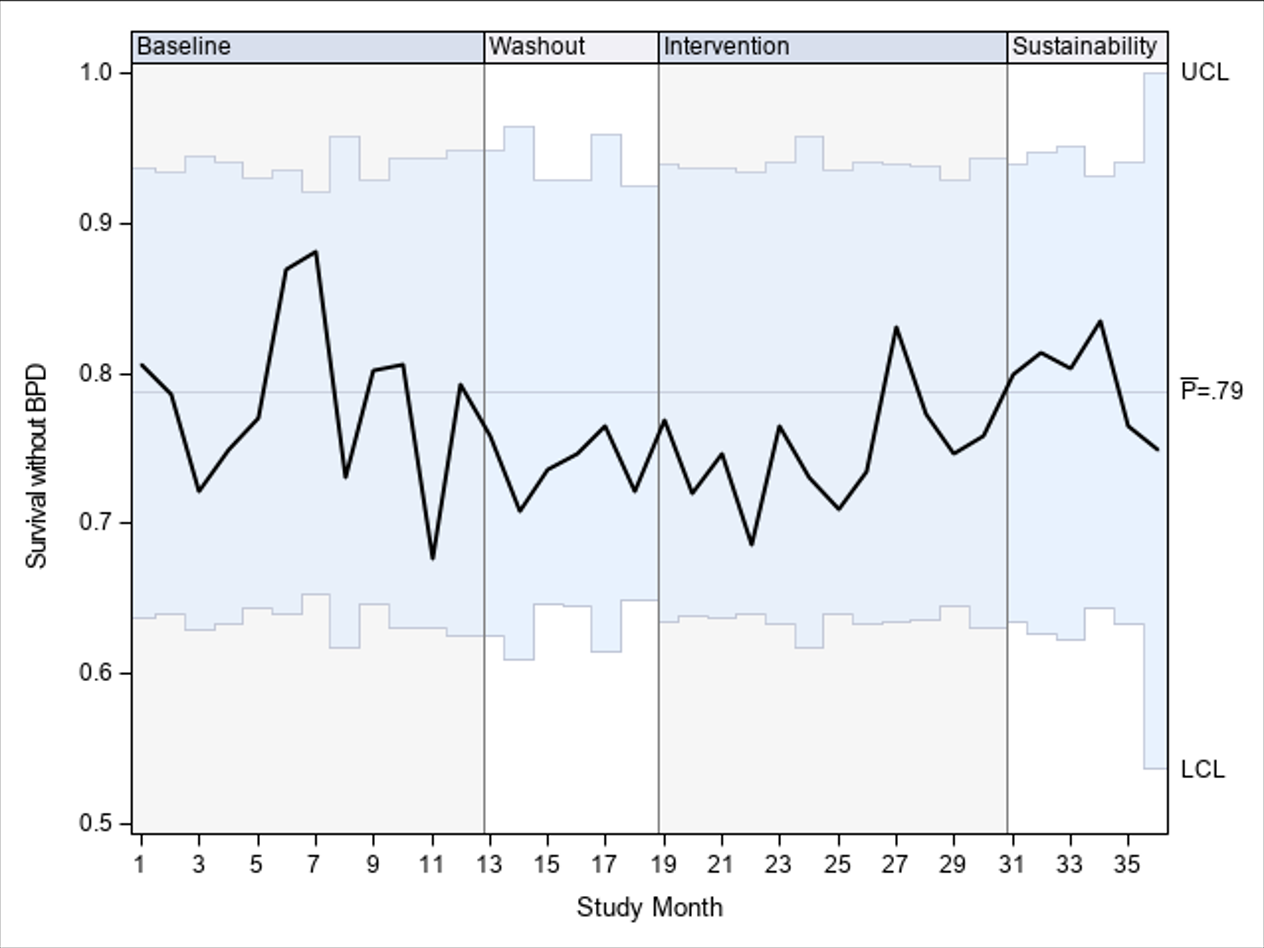
Figure 2. Rate of intubation in the delivery room for centers participating in Simulating Success.