Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation II
487 - The Perinatal Risk Factors Affecting the Newborn Resuscitation in Meconium-stained Deliveries
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 487
Publication Number: 487.231
Publication Number: 487.231
Arpitha Chiruvolu, Baylor University Medical Center, Dallas, TX, United States; Samantha Fine, Texas A&M College of Medicine, Baylor University Medical Center Dallas, DALLAS, TX, United States; Sujata Desai, Baylor University Medical center, Dallas, TX, United States
.jpg)
Samantha Fine, BA
Medical Student
Texas A&M College of Medicine, Baylor University Medical Center Dallas
DALLAS, Texas, United States
Presenting Author(s)
Background:
The presence of meconium-stained amniotic fluid (MSAF) is considered a significant perinatal risk factor that increases the likelihood of newborn resuscitation in the delivery room. Even though the routine intubation and suctioning of meconium-stained newborns is not recommended, the American Heart Association 2020 guidelines suggest that a neonatal team trained in advanced resuscitation is readily available to attend these deliveries especially when additional perinatal risk factors are present. However, these risk factors are not clearly defined.
Objective:
The purpose of this study was to identify the additional perinatal risk factors that increase the odds of a meconium-stained newborn needing resuscitation.
Design/Methods:
This is a multicenter retrospective cohort study. Chart reviews were performed of the deliveries ≥ 35 weeks' gestation associated with MSAF that occurred between January 1, 2017 to December 31, 2019. Intervention was defined as the newborn needing any resuscitation efforts in addition to the initial routine steps such as providing warmth, drying, positioning and clearing the upper airway with a bulb when needed. The intervention included oropharyngeal suctioning of meconium with a catheter, free flow oxygen, continuous positive airway pressure, positive pressure ventilation, intubation, endotracheal suctioning, chest compressions, and/or medications. The newborns needing intervention were compared to those not needing intervention. Logistic regression analysis was performed to define the perinatal factors which significantly increased the odds of a meconium-stained newborn needing intervention.
Results:
Out of 2213 infants born via MSAF, only 491 (22.2%) needed intervention. Utilizing logistic regression analysis correcting for gestational age and birth weight, we assessed the perinatal factors affecting the intervention of the newborn in the delivery room. Primigravida, thick meconium, fetal distress, chorioamnionitis, rupture of membranes ≥ 18 hours, postterm (gestational age > 42 weeks), cesarean section or shoulder dystocia significantly increased the odds of meconium-stained newborn needing intervention. The perinatal factors associated with significantly decreased odds of needing intervention were vaginal delivery and delayed cord clamping. (Table)
Conclusion(s):
By assessing the perinatal risk factors affecting the newborn resuscitation in the delivery room the neonatal teams can be appropriately prioritized and optimally utilized in the deliveries associated with MSAF.
Table: Perinatal factors affecting the intervention in meconium-stained deliveries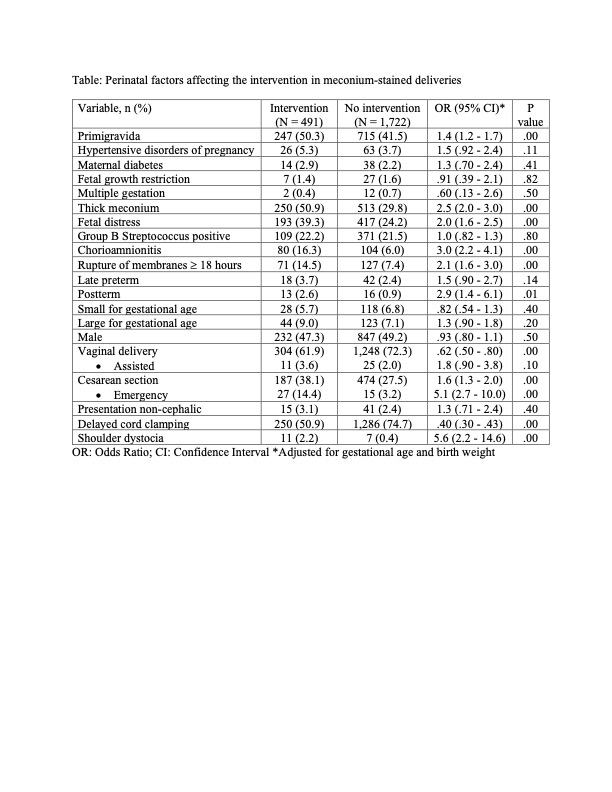 OR: Odds Ratio; CI: Confidence Interval *Adjusted for gestational age and birth weight
OR: Odds Ratio; CI: Confidence Interval *Adjusted for gestational age and birth weight
The presence of meconium-stained amniotic fluid (MSAF) is considered a significant perinatal risk factor that increases the likelihood of newborn resuscitation in the delivery room. Even though the routine intubation and suctioning of meconium-stained newborns is not recommended, the American Heart Association 2020 guidelines suggest that a neonatal team trained in advanced resuscitation is readily available to attend these deliveries especially when additional perinatal risk factors are present. However, these risk factors are not clearly defined.
Objective:
The purpose of this study was to identify the additional perinatal risk factors that increase the odds of a meconium-stained newborn needing resuscitation.
Design/Methods:
This is a multicenter retrospective cohort study. Chart reviews were performed of the deliveries ≥ 35 weeks' gestation associated with MSAF that occurred between January 1, 2017 to December 31, 2019. Intervention was defined as the newborn needing any resuscitation efforts in addition to the initial routine steps such as providing warmth, drying, positioning and clearing the upper airway with a bulb when needed. The intervention included oropharyngeal suctioning of meconium with a catheter, free flow oxygen, continuous positive airway pressure, positive pressure ventilation, intubation, endotracheal suctioning, chest compressions, and/or medications. The newborns needing intervention were compared to those not needing intervention. Logistic regression analysis was performed to define the perinatal factors which significantly increased the odds of a meconium-stained newborn needing intervention.
Results:
Out of 2213 infants born via MSAF, only 491 (22.2%) needed intervention. Utilizing logistic regression analysis correcting for gestational age and birth weight, we assessed the perinatal factors affecting the intervention of the newborn in the delivery room. Primigravida, thick meconium, fetal distress, chorioamnionitis, rupture of membranes ≥ 18 hours, postterm (gestational age > 42 weeks), cesarean section or shoulder dystocia significantly increased the odds of meconium-stained newborn needing intervention. The perinatal factors associated with significantly decreased odds of needing intervention were vaginal delivery and delayed cord clamping. (Table)
Conclusion(s):
By assessing the perinatal risk factors affecting the newborn resuscitation in the delivery room the neonatal teams can be appropriately prioritized and optimally utilized in the deliveries associated with MSAF.
Table: Perinatal factors affecting the intervention in meconium-stained deliveries
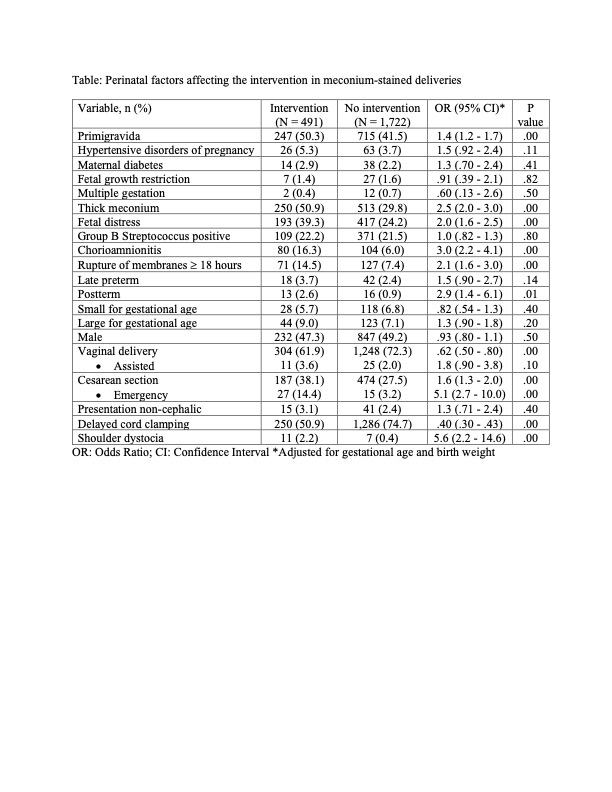 OR: Odds Ratio; CI: Confidence Interval *Adjusted for gestational age and birth weight
OR: Odds Ratio; CI: Confidence Interval *Adjusted for gestational age and birth weight