Neonatal Neurology: Basic
Category: Abstract Submission
Neurology 3: Basic-Translational
419 - Time course of changes in the Neurovascular Unit after hypoxic-ischemic injury in neonatal rats
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 419
Publication Number: 419.237
Publication Number: 419.237
Kazuki Hatayama, Women & Infants Hospital of Rhode Island, providence, RI, United States; Riddick A. Sydney, Women & Infants Hospital of Rhode Island, The Warren Alpert Medical School of Brown University, New Britain, CT, United States; Fares Awa, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Xiaodi Chen, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Barbara Stonestreet, Women & Infants Hospital of Rhode Island, Providence, RI, United States

Kazuki Hatayama, MD, PhD (he/him/his)
clinical fellowship
National Center for Child Health and Development, Tokyo, Japan
Tokyo, Tokyo, Japan
Presenting Author(s)
Background: Hypoxic-ischemic (HI) insults can result in severe neurologic sequela. The mechanism(s) underlying HI related brain injury remain to be determined. The neurovascular unit (NVU) represents a composite of structures that protect the developing brain from the influx of detrimental molecules. Changes in the NVU after exposure to HI are important because they could reveal potential endogenous neuroprotective pathways in the cerebral microvasculature. Moreover, the time course of changes in NVU after HI remains to be determined.
Objective: To determine the time course of changes in the NVU after exposure of neonatal rats to severe HI.
Design/Methods: Brains were collected from rats exposed to right carotid artery ligation and 120 min of hypoxia on postnatal day 7 with recovery for 6 (HI-6h) or 48 h (HI-48h) after exposure to HI or sham treatment (Sham). The right HI and left hypoxic (H) alone sides of the brains were examined for vascular density (laminin), pericyte (PDGFRβ) and astrocyte (GFAP) coverage of the microvasculature in the cerebral cortex, white matter and hippocampus by quantitative immunohistochemistry. Statistical analysis was by two-way analysis of variance (ANOVA) followed by the Tukey’s multiple comparison test.
Results: Exposure to HI was associated with increases in microvascular density (P < 0.05) at 6 and 48 h after HI compared with Sham treatment (Figure 1A) and larger microvascular density at 48 h after HI compared with exposure to hypoxia alone (left side) in the cerebral cortex. Vascular density was also higher in the white matter 6 h after HI compared with Sham (Figure 1B). However, differences in vascular density were not observed in the hippocampus (Figure 1C). Pericyte coverage was lower 6 h after exposure to HI compared with Sham (Figure 2A) and also lower 48 h after H compared with Sham in the cerebral cortex. Differences in pericyte coverage were not observed in white matter or hippocampus (Figure 2B, 2C). Differences in astrocyte vascular coverage were not observed in the cerebral cortex, white matter or hippocampus (Figure 3A, 3B, 3C).Conclusion(s): HI related brain injury in neonatal rat was associated with in increases in vascular density and neurovascular remodeling. The time course in the responses of the different components of the NVU varied after exposure to HI. There were also differential regional responses in the elements of the NVU in response to H and HI. We speculate that these alterations in the NVU could predispose to neuronal injury.
Microvascular density.jpg) Microvessel density. Graphs representing microvessel densities expressed as the percent of the fields segmented on anti-Laminin stained sections in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains.
Microvessel density. Graphs representing microvessel densities expressed as the percent of the fields segmented on anti-Laminin stained sections in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains.
Pericyte coverage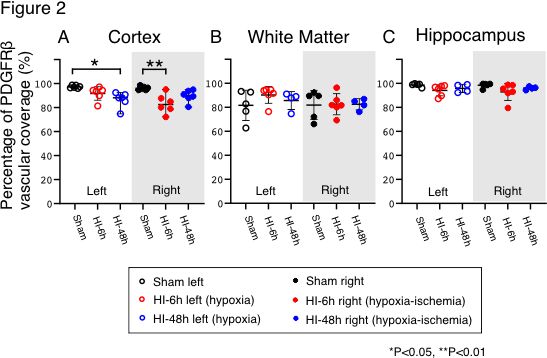 Pericyte coverage surrounding the brain microvessels. Graphs representing the pericyte coverage expressed in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains. Pericyte coverage expressed as the percent of positive PDGFRβ area overlapping with the vessel wall.
Pericyte coverage surrounding the brain microvessels. Graphs representing the pericyte coverage expressed in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains. Pericyte coverage expressed as the percent of positive PDGFRβ area overlapping with the vessel wall.
Objective: To determine the time course of changes in the NVU after exposure of neonatal rats to severe HI.
Design/Methods: Brains were collected from rats exposed to right carotid artery ligation and 120 min of hypoxia on postnatal day 7 with recovery for 6 (HI-6h) or 48 h (HI-48h) after exposure to HI or sham treatment (Sham). The right HI and left hypoxic (H) alone sides of the brains were examined for vascular density (laminin), pericyte (PDGFRβ) and astrocyte (GFAP) coverage of the microvasculature in the cerebral cortex, white matter and hippocampus by quantitative immunohistochemistry. Statistical analysis was by two-way analysis of variance (ANOVA) followed by the Tukey’s multiple comparison test.
Results: Exposure to HI was associated with increases in microvascular density (P < 0.05) at 6 and 48 h after HI compared with Sham treatment (Figure 1A) and larger microvascular density at 48 h after HI compared with exposure to hypoxia alone (left side) in the cerebral cortex. Vascular density was also higher in the white matter 6 h after HI compared with Sham (Figure 1B). However, differences in vascular density were not observed in the hippocampus (Figure 1C). Pericyte coverage was lower 6 h after exposure to HI compared with Sham (Figure 2A) and also lower 48 h after H compared with Sham in the cerebral cortex. Differences in pericyte coverage were not observed in white matter or hippocampus (Figure 2B, 2C). Differences in astrocyte vascular coverage were not observed in the cerebral cortex, white matter or hippocampus (Figure 3A, 3B, 3C).Conclusion(s): HI related brain injury in neonatal rat was associated with in increases in vascular density and neurovascular remodeling. The time course in the responses of the different components of the NVU varied after exposure to HI. There were also differential regional responses in the elements of the NVU in response to H and HI. We speculate that these alterations in the NVU could predispose to neuronal injury.
Microvascular density
.jpg) Microvessel density. Graphs representing microvessel densities expressed as the percent of the fields segmented on anti-Laminin stained sections in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains.
Microvessel density. Graphs representing microvessel densities expressed as the percent of the fields segmented on anti-Laminin stained sections in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains.Pericyte coverage
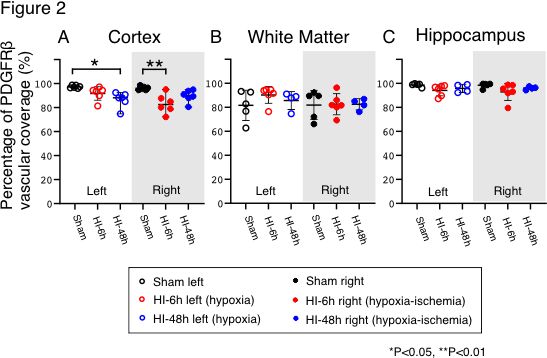 Pericyte coverage surrounding the brain microvessels. Graphs representing the pericyte coverage expressed in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains. Pericyte coverage expressed as the percent of positive PDGFRβ area overlapping with the vessel wall.
Pericyte coverage surrounding the brain microvessels. Graphs representing the pericyte coverage expressed in the cerebral cortex (A), white matter (B) and hippocampus (C) of the hypoxic (left) and hypoxic-ischemic (right) sides of the neonatal rat brains. Pericyte coverage expressed as the percent of positive PDGFRβ area overlapping with the vessel wall.