Critical Care
Category: Abstract Submission
Critical Care II
28 - Trends in Sedative Drug Utilization for Mechanically Ventilated Patients in US Pediatric Intensive Care Units, 2010-20
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 28
Publication Number: 28.201
Publication Number: 28.201
Jennifer J. Lee, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Ann Kim, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; lena Sun, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
- JL
Jennifer J. Lee, MD
Assistant Professor of Anesthesiology
Columbia University Vagelos College of Physicians and Surgeons
New York, New York, United States
Presenting Author(s)
Background: Sedatives are often administered in the pediatric intensive care unit (PICU) to facilitate the tolerance of mechanical ventilation (MV). Sedation management in PICU patients is variable with heterogeneity of clinical environments, patient-, and provider-related factors. To understand the current state of sedation practice in PICU patients, a description of sedative utilization patterns would be valuable, but is lacking.
Objective: To investigate trends in sedative use for MV patients in US PICUs.
Design/Methods: A retrospective analysis was performed using the Pediatric Health Information System Database. Demographic, clinical, and pharmacy data were extracted, and descriptive statistics were summarized. Multivariable logistic regressions were performed to identify significant factors associated with receipt of 4+ sedative classes or neuromuscular blockade (NMB). Sedative classes were defined as opioids (OP), benzodiazepines (BZ), alpha-2 agonists (AA), propofol (PF), barbiturates (BT), and ketamine (KT).
Results: Of 259,702 PICU discharges, there were 212,457 patients aged 2.0+/-10.0 years MV for 2.0+/-5.0 days (Table 1). 80.3% (n=170,652) received OP, 76.1% (n=161,748) BZ, 46.4% (n=98,518) AA, 37.5% (n=79,731) PF, 22.2% (n=47,251) KT, and 8.6% (n=18,167) BT, either alone or in combination with other sedatives. 64.3% (n=136,568) were given NMB. From 2010 to 2020, increased use of AA (+28.7%), KT (+12.3%), PF (+14.4%) was observed, and decreased use was seen with BZ (-14.4%), BT (-9.9%), and OP (-6.7%) (Figure 1). In 12.5% (n=26,469), no sedatives were documented. Only 6.9% (n=14,630) had a single class of sedatives with 17.9% (n=37,980) receiving 2 classes. 27.6% (n=58,561) had 3 classes; 35.2% (n=74,817) had 4+ classes (Table 2). In the 35.2% who had 4+ classes, OP and BZ were administered to nearly all patients (99.6%, n=74,536). Compared to those >12 years, those < 3 years were less likely to receive 4+ classes (OR=0.77, 95% CI 0.75-0.79, pConclusion(s): In this study, OP and BZ were the most commonly administered sedatives to MV PICU patients; both were included when 4+ classes were given. There has been a recent increase in the use of AA, KT, and PF with a reduction in the use of BZ, BT, and OP. Patients < 3 years were more likely to have been paralyzed and less likely to have received 4+ sedative classes.
Figure 1. Drug utilization in MV PICU patients from 2010 to 2020.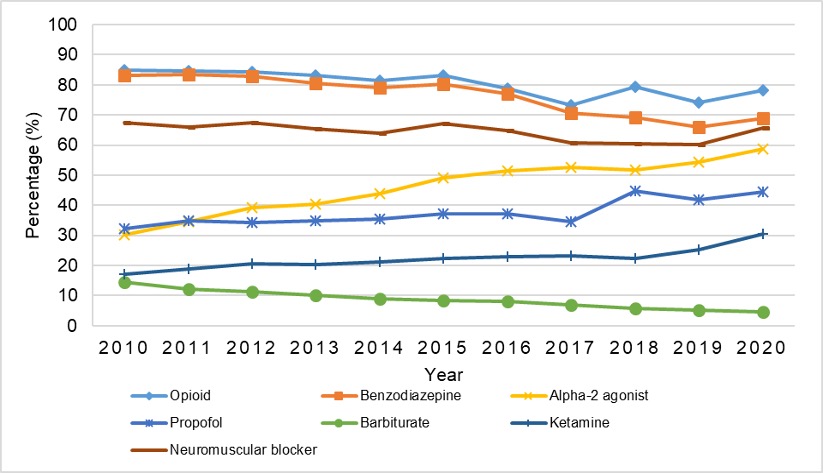
Table 1. Demographic and clinical characteristics of total study cohort, 2010-20..jpg)
Objective: To investigate trends in sedative use for MV patients in US PICUs.
Design/Methods: A retrospective analysis was performed using the Pediatric Health Information System Database. Demographic, clinical, and pharmacy data were extracted, and descriptive statistics were summarized. Multivariable logistic regressions were performed to identify significant factors associated with receipt of 4+ sedative classes or neuromuscular blockade (NMB). Sedative classes were defined as opioids (OP), benzodiazepines (BZ), alpha-2 agonists (AA), propofol (PF), barbiturates (BT), and ketamine (KT).
Results: Of 259,702 PICU discharges, there were 212,457 patients aged 2.0+/-10.0 years MV for 2.0+/-5.0 days (Table 1). 80.3% (n=170,652) received OP, 76.1% (n=161,748) BZ, 46.4% (n=98,518) AA, 37.5% (n=79,731) PF, 22.2% (n=47,251) KT, and 8.6% (n=18,167) BT, either alone or in combination with other sedatives. 64.3% (n=136,568) were given NMB. From 2010 to 2020, increased use of AA (+28.7%), KT (+12.3%), PF (+14.4%) was observed, and decreased use was seen with BZ (-14.4%), BT (-9.9%), and OP (-6.7%) (Figure 1). In 12.5% (n=26,469), no sedatives were documented. Only 6.9% (n=14,630) had a single class of sedatives with 17.9% (n=37,980) receiving 2 classes. 27.6% (n=58,561) had 3 classes; 35.2% (n=74,817) had 4+ classes (Table 2). In the 35.2% who had 4+ classes, OP and BZ were administered to nearly all patients (99.6%, n=74,536). Compared to those >12 years, those < 3 years were less likely to receive 4+ classes (OR=0.77, 95% CI 0.75-0.79, pConclusion(s): In this study, OP and BZ were the most commonly administered sedatives to MV PICU patients; both were included when 4+ classes were given. There has been a recent increase in the use of AA, KT, and PF with a reduction in the use of BZ, BT, and OP. Patients < 3 years were more likely to have been paralyzed and less likely to have received 4+ sedative classes.
Figure 1. Drug utilization in MV PICU patients from 2010 to 2020.
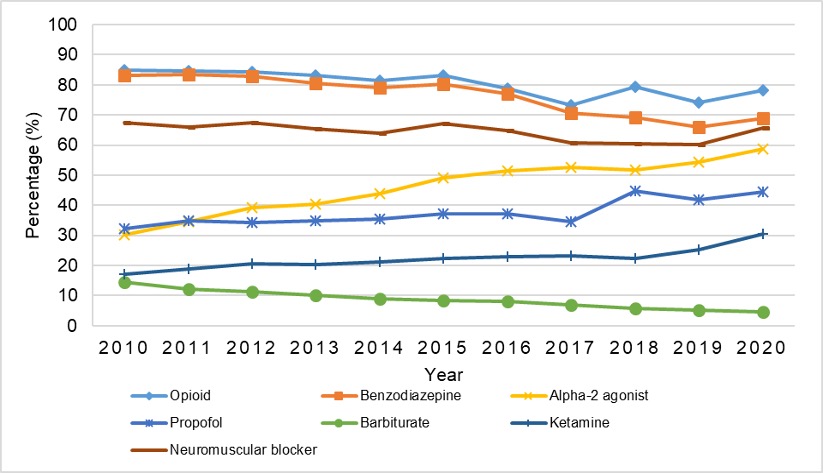
Table 1. Demographic and clinical characteristics of total study cohort, 2010-20.
.jpg)
