Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Potpourri
554 - Antimicrobial Therapy for LRTI is Associated with Improved Respiratory Severity Scores in Infants with severe BPD
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 554
Heidi Morris, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Joseph Piccione, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Erik A. Jensen, Children's Hospital of Philadelphia, haddonfield, NJ, United States; Huayan Zhang, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Kathleen Gibbs, Children's Hospital of Philadelphia, Philadelphia, PA, United States
.jpg)
Heidi Morris, MMS, PA-C
Physician Assistant
Children’s Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Infants with severe bronchopulmonary dysplasia (sBPD) are at risk for lower respiratory tract infection (LRTI) due to prolonged intubation/mechanical ventilation, disordered respiratory mechanics, and impaired airway mucus clearance. Rates of LRTI in infants with sBPD may be underrecognized, and treatment might reduce disease severity.
Objective: To determine if treatment with varying durations of antibiotics is associated with improved respiratory status in infants with sBPD and LRTI diagnosed by bronchioalveolar lavage (BAL).
Design/Methods: We performed a retrospective cohort study of neonates with sBPD (based on 2001 NIH Consensus Definition) requiring invasive mechanical ventilation at Children’s Hospital of Philadelphia between 2013 and 2021 in whom LRTI was confirmed based on bedside flexible bronchoscopy with bronchoalveolar lavage. LRTI was defined as growth of a single bacterial isolate at >10,000 CFU/mL and elevated BAL neutrophil count. Respiratory severity score (RSS), the product of mean airway pressure (MAP) and fraction of inspired oxygen (FiO2), was compared before antibiotics, and 7 and 14 days after initiation of antibiotics. Paired T-tests were used to compare changes within individuals and unpaired T-tests were used to compared differences between those receiving 7 and at least 14 days of antibiotics.
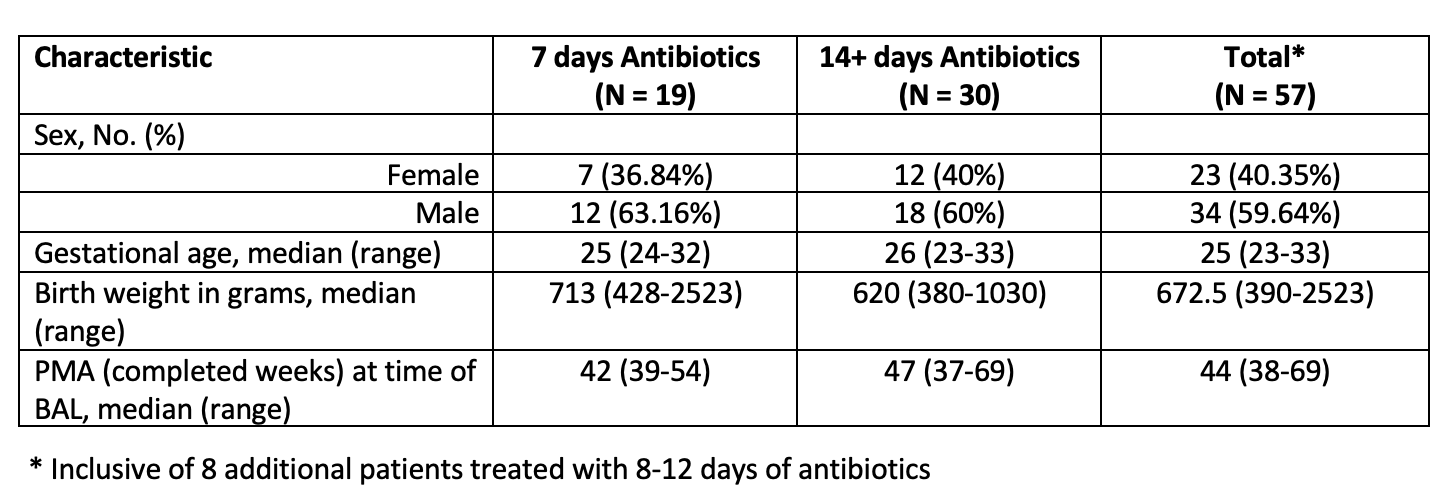
Results: Fifty-seven neonates met inclusion criteria. Approximately 60% were male. The median gestational age, birth weight and post-menstrual age at time of bronchoscopy was 25 weeks (23-34), 673 g, and 44 weeks respectively. Nineteen infants were treated for 7 days and 30 were treated with at least 14 days of antibiotics. Clinical characteristics were similar in both groups (Table 1). Eight additional patients were treated for 8 to 12 days. Overall RSS improved by 11.8% from a mean of 9.02 at Day 0 to 7.73 following 7 days of antibiotics (p = < 0.00001). Those treated with at least 14 days of antibiotics had an additional 9.7% reduction in RSS, while there was a 2.0% reduction seen on Day 14 in those receiving 7 days of antibiotics, however this difference was not statistically significant (p=0.44).Conclusion(s): Infants with sBPD requiring invasive mechanical ventilation are at risk for bacterial LRTI and treatment with antibiotics is associated with a significant reduction in RSS. Flexible bronchoscopy with bronchoalveolar lavage can be utilized to identify patients who may benefit from antibiotic therapy. Further study is needed to determine the optimal duration of antibiotic therapy.
Table 1. Cohort Characteristics by Length of Antibiotic Course & Totals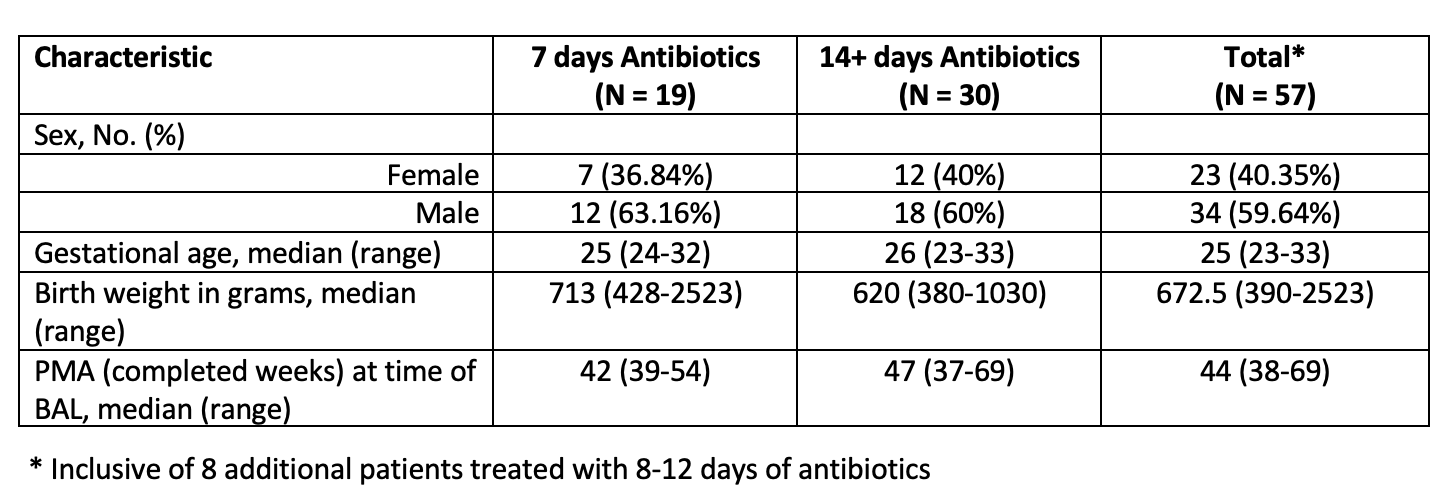
Objective: To determine if treatment with varying durations of antibiotics is associated with improved respiratory status in infants with sBPD and LRTI diagnosed by bronchioalveolar lavage (BAL).
Design/Methods: We performed a retrospective cohort study of neonates with sBPD (based on 2001 NIH Consensus Definition) requiring invasive mechanical ventilation at Children’s Hospital of Philadelphia between 2013 and 2021 in whom LRTI was confirmed based on bedside flexible bronchoscopy with bronchoalveolar lavage. LRTI was defined as growth of a single bacterial isolate at >10,000 CFU/mL and elevated BAL neutrophil count. Respiratory severity score (RSS), the product of mean airway pressure (MAP) and fraction of inspired oxygen (FiO2), was compared before antibiotics, and 7 and 14 days after initiation of antibiotics. Paired T-tests were used to compare changes within individuals and unpaired T-tests were used to compared differences between those receiving 7 and at least 14 days of antibiotics.
Results: Fifty-seven neonates met inclusion criteria. Approximately 60% were male. The median gestational age, birth weight and post-menstrual age at time of bronchoscopy was 25 weeks (23-34), 673 g, and 44 weeks respectively. Nineteen infants were treated for 7 days and 30 were treated with at least 14 days of antibiotics. Clinical characteristics were similar in both groups (Table 1). Eight additional patients were treated for 8 to 12 days. Overall RSS improved by 11.8% from a mean of 9.02 at Day 0 to 7.73 following 7 days of antibiotics (p = < 0.00001). Those treated with at least 14 days of antibiotics had an additional 9.7% reduction in RSS, while there was a 2.0% reduction seen on Day 14 in those receiving 7 days of antibiotics, however this difference was not statistically significant (p=0.44).Conclusion(s): Infants with sBPD requiring invasive mechanical ventilation are at risk for bacterial LRTI and treatment with antibiotics is associated with a significant reduction in RSS. Flexible bronchoscopy with bronchoalveolar lavage can be utilized to identify patients who may benefit from antibiotic therapy. Further study is needed to determine the optimal duration of antibiotic therapy.
Table 1. Cohort Characteristics by Length of Antibiotic Course & Totals