Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: QI
327 - Capture if you Can: A Quality Improvement Project to Improve Documentation and Coding Accuracy in a Large Multisite Division of Pediatric Hospital Medicine.
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 327
Publication Number: 327.323
Publication Number: 327.323
Douglas A. Dodds, Levine Children's Hospital, Cornelius, NC, United States; Sara Horstmann, Levine Children's Hospital, Cornelius, NC, United States; Melissa Schutt, Levine Children's Hospital, Charlotte, NC, United States; Caroline DSouza, Levine Children's Hospital, Charlotte, NC, United States; Jenna Brooks, Levine Children's Hospital, Charlotte, NC, United States
Douglas A. Dodds, MD
Site based Medical Director
Levine Children's Hospital
Cornelius, North Carolina, United States
Presenting Author(s)
Background: Providers perform poorly in documenting and coding for their care. This problem stems from lack of billing and coding training during medical education. Most practitioners are introduced to the rules of billing and coding during their orientation to a new job, and then receive little feedback on subsequent performance. This process results in erroneous, poorly formed rules of thumb that lead to inaccurate documentation and billing. Documents produced in this manner are less informative, poorly assign medical complexity, underestimate work done, and decrease revenue. All problems with negative impact on the delivery of care for current and future patients.
Objective: 1. Improve discharge documentation to appropriately increase the use of the 99239 code (Discharge >30 minutes). 2. Improve documentation to accurately reflect critical care in the newborn and inpatient setting. 3.Improve documentation to more accurately reflect daily work done by the division.
Design/Methods: A Multidisciplinary Team (MDT) was created including members from Finance, Coding Compliance, Division Administration, and Providers. Baseline data for percentage of discharges greater than 30 minutes, total critical care bills per month, and average wRVU/Encounter were collected. Three interventions were tested 1. Individual real-time education during actual documentation and billing, 2. Simplified coding rules disseminated through group education. 3. Monthly billing updates for data review and feedback were provided. The MDT met monthly to review interventions, create reports, plan educational offerings, and review data. The Model for Improvement was used for these interventions.
Results: After implementation of our project, average wRVU/Encounter increased from 1.73 to 2.39, a 38.2 % Increase over baseline. Our percentage of discharges >30 minutes grew from 25% to 57%, a 128% increase from baseline. The average number of critical care codes per month increased from 7 codes per month to 32, a 357% increase. There were no increases in coding errors or claim rejections during the intervention time. This project brought 1.5 million dollars in net revenue to our division over the study period.Conclusion(s): This project used targeted real time educational opportunities, simplified coding rules, and monthly group report outs to successfully increase valid wRVU/provider, percentage change in discharge >30 minutes codes, and volume of critical care billing. Accurate documentation of billing, and coding, created a more accurate representation of the work performed by our large Pediatric Hospital Medicine Group.
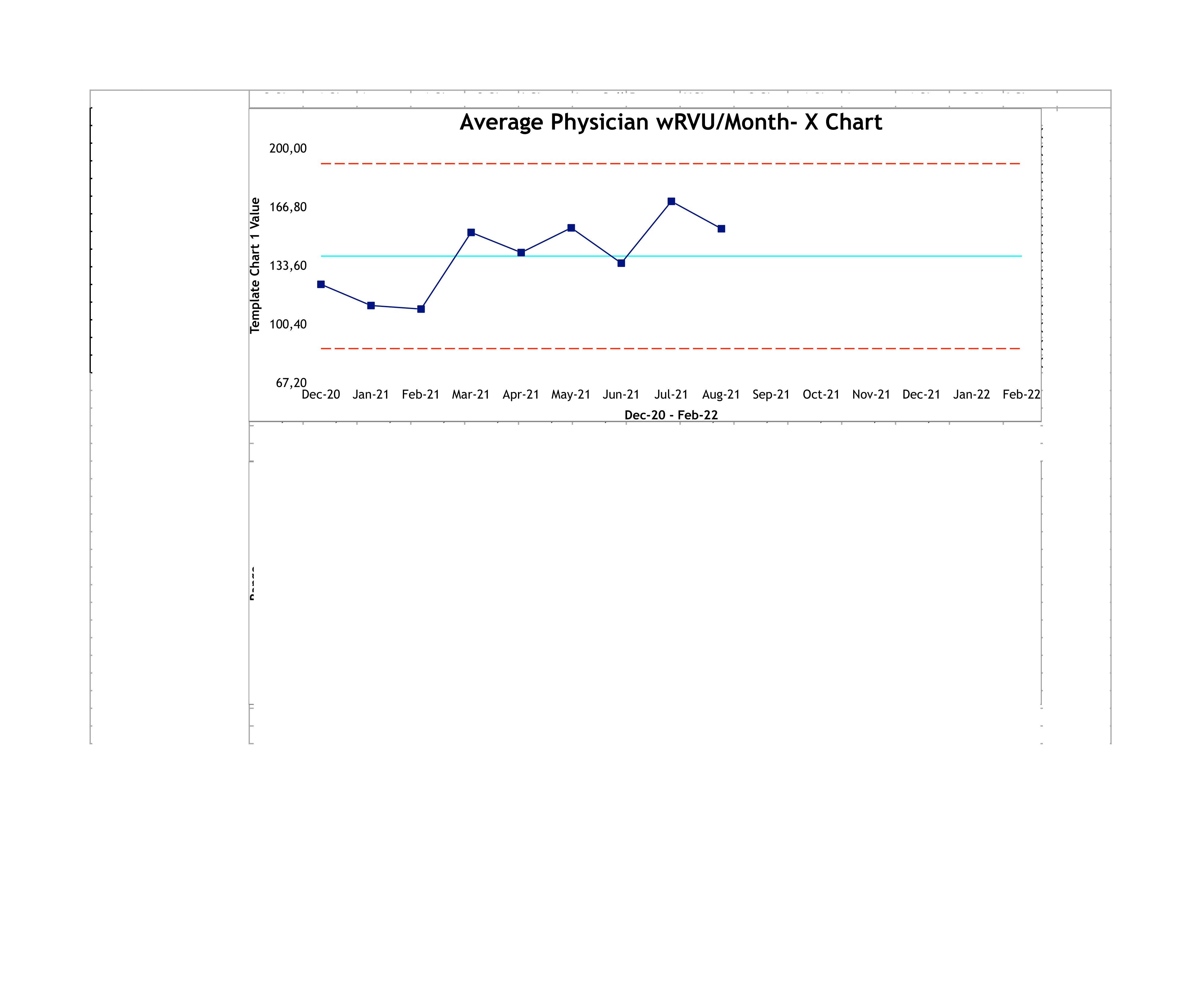
Control Chart for Discharge Greater than 30 Minutes.png)
Control Chart for Average Provider wRVU/Month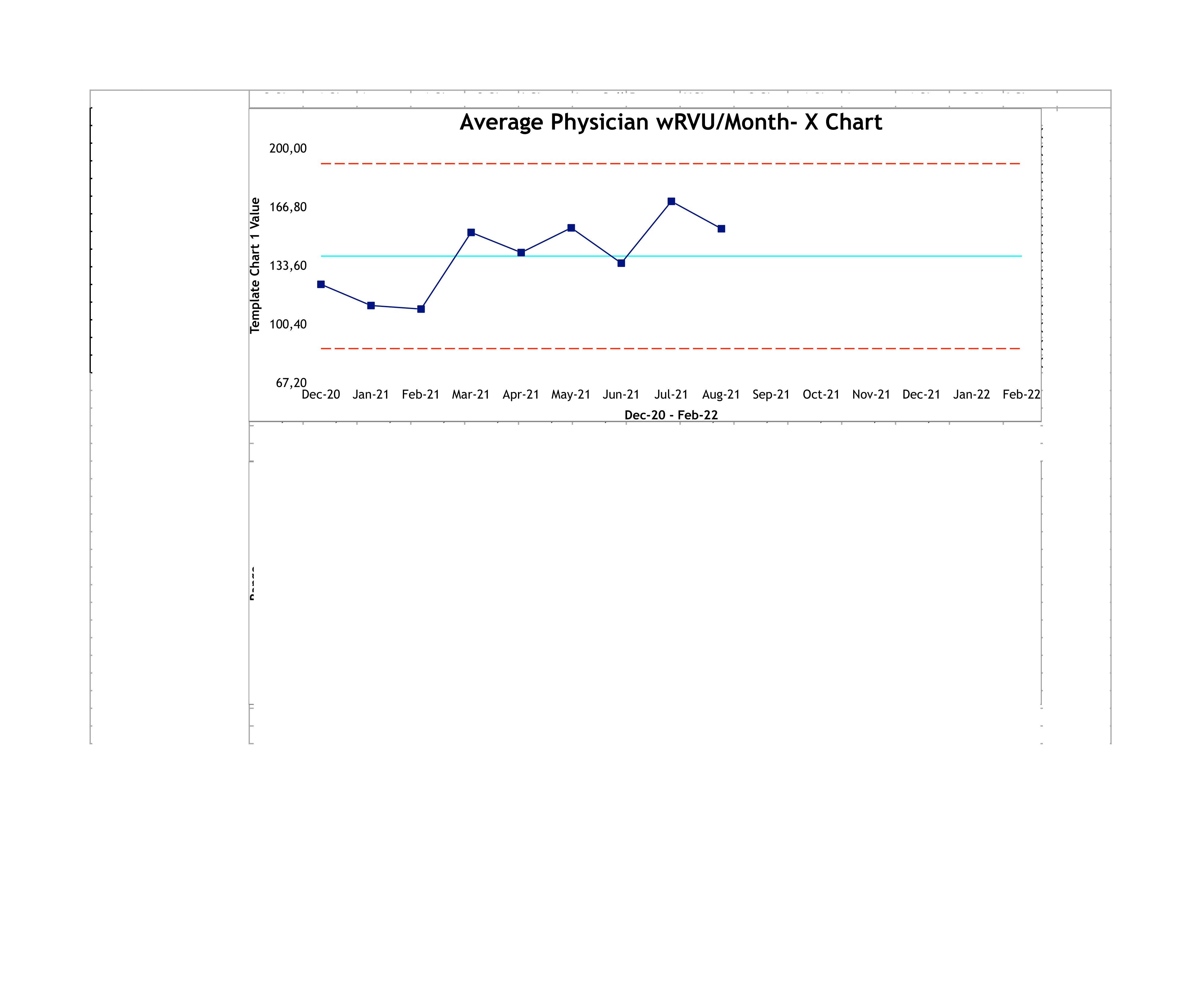
Objective: 1. Improve discharge documentation to appropriately increase the use of the 99239 code (Discharge >30 minutes). 2. Improve documentation to accurately reflect critical care in the newborn and inpatient setting. 3.Improve documentation to more accurately reflect daily work done by the division.
Design/Methods: A Multidisciplinary Team (MDT) was created including members from Finance, Coding Compliance, Division Administration, and Providers. Baseline data for percentage of discharges greater than 30 minutes, total critical care bills per month, and average wRVU/Encounter were collected. Three interventions were tested 1. Individual real-time education during actual documentation and billing, 2. Simplified coding rules disseminated through group education. 3. Monthly billing updates for data review and feedback were provided. The MDT met monthly to review interventions, create reports, plan educational offerings, and review data. The Model for Improvement was used for these interventions.
Results: After implementation of our project, average wRVU/Encounter increased from 1.73 to 2.39, a 38.2 % Increase over baseline. Our percentage of discharges >30 minutes grew from 25% to 57%, a 128% increase from baseline. The average number of critical care codes per month increased from 7 codes per month to 32, a 357% increase. There were no increases in coding errors or claim rejections during the intervention time. This project brought 1.5 million dollars in net revenue to our division over the study period.Conclusion(s): This project used targeted real time educational opportunities, simplified coding rules, and monthly group report outs to successfully increase valid wRVU/provider, percentage change in discharge >30 minutes codes, and volume of critical care billing. Accurate documentation of billing, and coding, created a more accurate representation of the work performed by our large Pediatric Hospital Medicine Group.
Control Chart for Discharge Greater than 30 Minutes
.png)
Control Chart for Average Provider wRVU/Month