Neonatal General
Category: Abstract Submission
Neonatology General 8: Health Disparities - Health Services Research
218 - How much does a minimum weight at discharge delay discharge from the NICU?
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 218
Publication Number: 218.339
Publication Number: 218.339
Riddhi Desai, UH Rainbow Babies & Children's Hospital, Shaker heights, OH, United States; Monika Bhola, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Rita M. Ryan, Case Western Reserve University, Cleveland, OH, United States

Riddhi Desai, MD MPH (she/her/hers)
Fellow
Akron Children's Hospital
Shaker Heights, Ohio, United States
Presenting Author(s)
Background: Our NICU policy requires a minimum weight (wt) of 1800 grams (g) for discharge regardless of postmenstrual age (PMA). However, current AAP and Canadian guidelines recommend discharge at “physiologic maturity” (PM), regardless of wt.
Objective: Determine if a significant number of hospital days (HD) can be saved for infants who reach PM prior to reaching 1800g.
Design/Methods: We reviewed charts to determine if a clinically relevant number of HD (≥ 20 annually decided a priori) could be saved when discharge occurred at PM even if < 1800g; and to determine whether the difference at PM or “virtual” discharge and actual discharge was greater in small for gestational age (SGA) infants. We studied infants with birthweight (bw) 1300g-1800g to target those most likely to be affected by our minimum wt policy. Sample size calculation indicated 8 babies needed to not miss a difference of 20days (d). PM was defined as: 1) maintaining temperature in an open crib of ≥36.3°C for ≥48h; 2) oral feed volume of ≥120 ml/kg/day; 3) consistent wt gain for 2d without enteric tube; 4) no apnea/bradycardia for 5d; 5) no desaturations for 1d. Infants with major congenital malformation were excluded. Continuous variables were analyzed by t-test, and chi-square or Fisher exact test used for categorical variables.
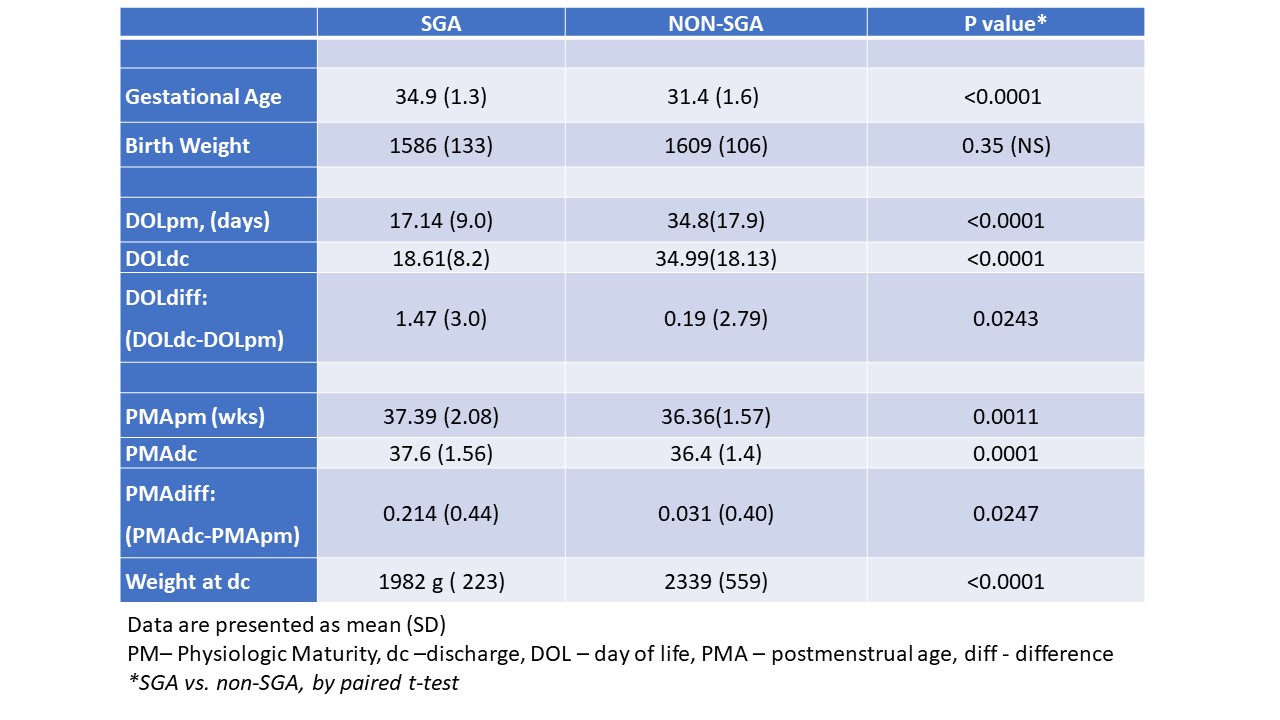
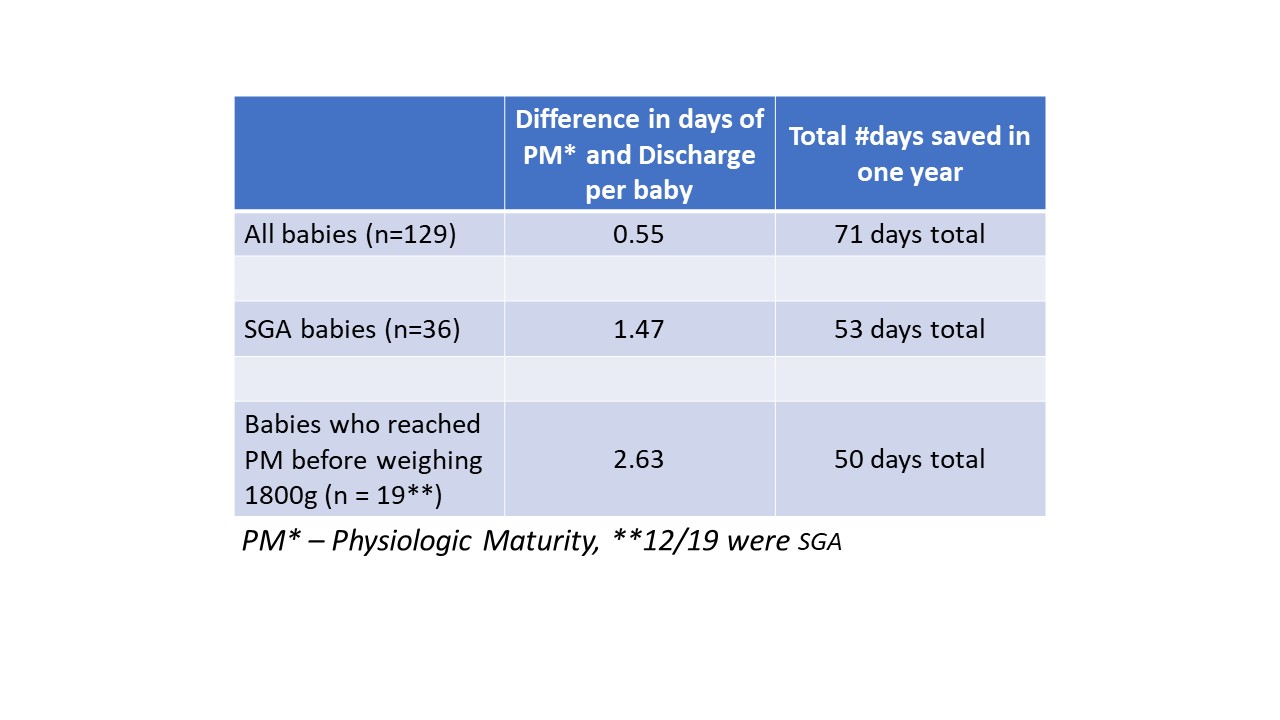
Results: 143 infants with bw 1300g-1800g were discharged in 2019; 14 were excluded (missing information (4), congenital anomalies (10)). Of the remaining 129, 36 (28%) were SGA. There was a significant difference between the day of age at discharge vs. when the infant reached PM of 0.55 days per infant (P-value 0.033) resulting in 71 total HD for the cohort. For SGA babies, this difference was 1.47 days, while it was 0.19 days in the non-SGA babies (P–value 0.0243). For 19 infants who reached PM < 1800g, there was an average of 2.63 days difference between PM and actual discharge (P-value < 0.001), contributing 50 of the 71 HD potentially saved; 63% of these 19 infants were SGA. Conclusion(s): There is a ~0.55 day difference between age at discharge and age at PM. If these infants were discharged when they reached PM, 71 HD per year could have been saved, saving ~$557,350 with discharge at PM. The minimum wt policy could have contributed to 50/71 (65%) of these HD. Our study did not examine if other reasons (e.g. transportation issues) would have precluded discharge at PM. If a QI project were undertaken, the SGA population would be an ideal target.
Table 1 Hospital Days Saved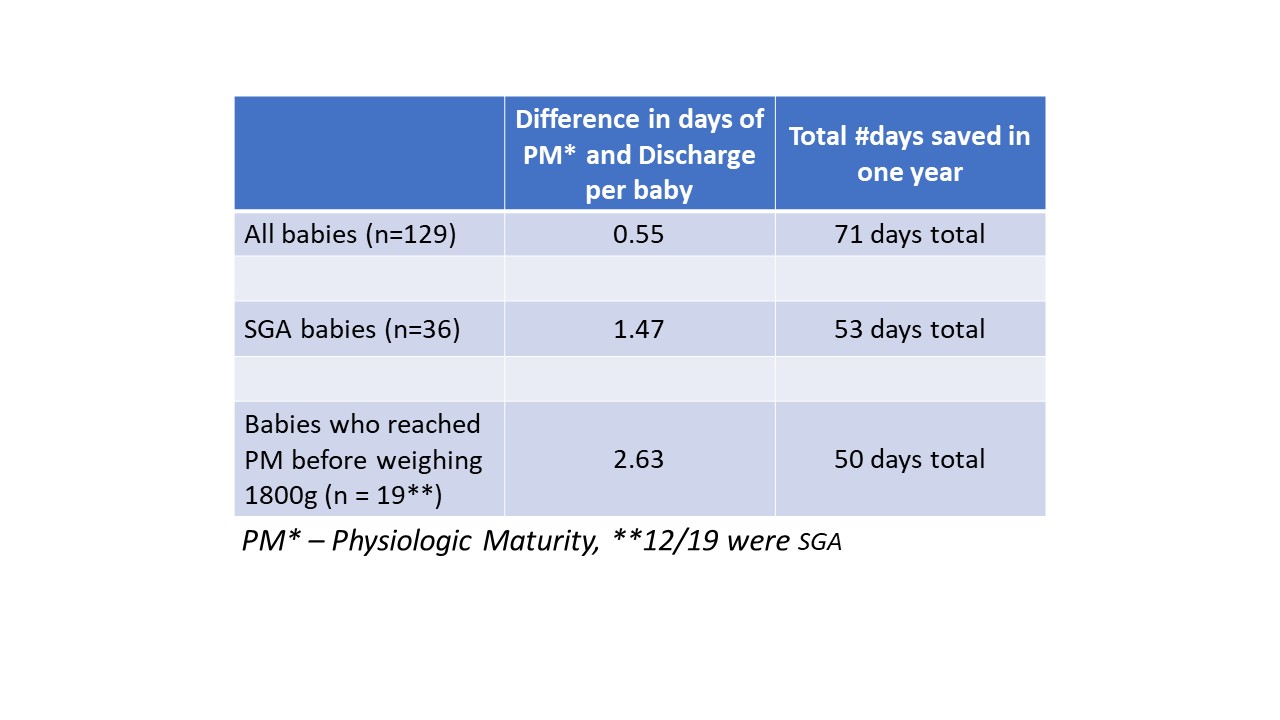
SGA Vs Non-SGA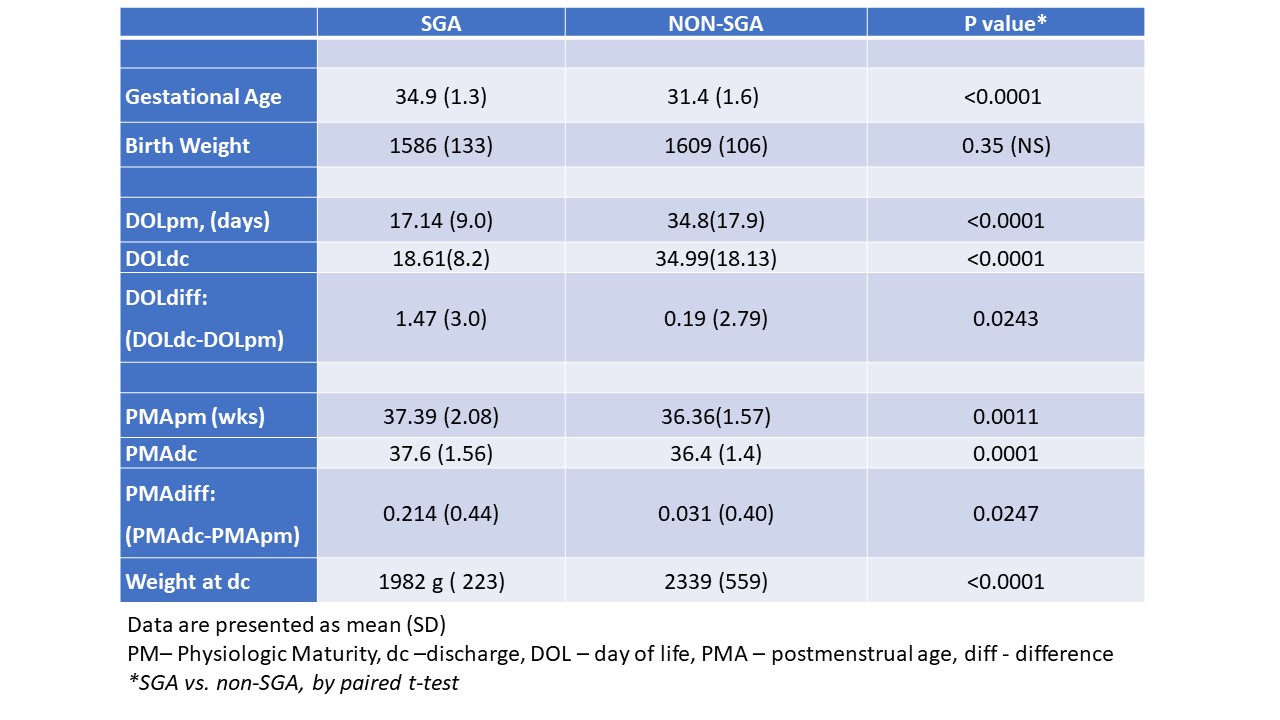
Objective: Determine if a significant number of hospital days (HD) can be saved for infants who reach PM prior to reaching 1800g.
Design/Methods: We reviewed charts to determine if a clinically relevant number of HD (≥ 20 annually decided a priori) could be saved when discharge occurred at PM even if < 1800g; and to determine whether the difference at PM or “virtual” discharge and actual discharge was greater in small for gestational age (SGA) infants. We studied infants with birthweight (bw) 1300g-1800g to target those most likely to be affected by our minimum wt policy. Sample size calculation indicated 8 babies needed to not miss a difference of 20days (d). PM was defined as: 1) maintaining temperature in an open crib of ≥36.3°C for ≥48h; 2) oral feed volume of ≥120 ml/kg/day; 3) consistent wt gain for 2d without enteric tube; 4) no apnea/bradycardia for 5d; 5) no desaturations for 1d. Infants with major congenital malformation were excluded. Continuous variables were analyzed by t-test, and chi-square or Fisher exact test used for categorical variables.
Results: 143 infants with bw 1300g-1800g were discharged in 2019; 14 were excluded (missing information (4), congenital anomalies (10)). Of the remaining 129, 36 (28%) were SGA. There was a significant difference between the day of age at discharge vs. when the infant reached PM of 0.55 days per infant (P-value 0.033) resulting in 71 total HD for the cohort. For SGA babies, this difference was 1.47 days, while it was 0.19 days in the non-SGA babies (P–value 0.0243). For 19 infants who reached PM < 1800g, there was an average of 2.63 days difference between PM and actual discharge (P-value < 0.001), contributing 50 of the 71 HD potentially saved; 63% of these 19 infants were SGA. Conclusion(s): There is a ~0.55 day difference between age at discharge and age at PM. If these infants were discharged when they reached PM, 71 HD per year could have been saved, saving ~$557,350 with discharge at PM. The minimum wt policy could have contributed to 50/71 (65%) of these HD. Our study did not examine if other reasons (e.g. transportation issues) would have precluded discharge at PM. If a QI project were undertaken, the SGA population would be an ideal target.
Table 1 Hospital Days Saved
SGA Vs Non-SGA