Nephrology: Clinical
Category: Abstract Submission
Nephrology III: General Nephrology and Dialysis
51 - Long-term healthcare utilization and associated costs after childhood dialysis-treated acute kidney injury
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 51
Publication Number: 51.340
Publication Number: 51.340
Cal H. Robinson, The Hospital for Sick Children, Toronto, ON, Canada; Nivethika Jeyakumar, ICES Western, London, ON, Canada; Bin Luo, ICES, London, ON, Canada; Danielle M. Nash, ICES, London, ON, Canada; Eric McArthur, ICES, London, ON, Canada; Jason H. Greenberg, Yale School of Medicine, new haven, CT, United States; David Askenazi, UAB, Birmingham, AL, United States; Stuart L. Goldstein, Cincinnati Children's Hospital, Cincinnati, OH, United States; Samuel A. Silver, Queen's University, KINGSTON, ON, Canada; Rahul Chanchlani, McGill University Faculty of Medicine and Health Sciences, Hamilton, ON, Canada

Cal H. Robinson, MD
Pediatric Nephrology Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Acute kidney injury (AKI) is common among hospitalized children and is associated with increased hospital length of stay and inpatient costs. However, there are limited data on post-discharge healthcare utilization and costs after AKI hospitalization.
Objective: To determine long-term healthcare utilization, costs, and physician follow-up patterns after pediatric dialysis-treated AKI hospitalization.
Design/Methods: Using provincial health administrative databases, we performed a retrospective cohort study of all hospitalized pediatric patients (0-18yr) surviving a dialysis-treated AKI episode between 1996-2017 in Ontario, Canada. AKI survivors were matched to four hospitalized comparators without dialysis-treated AKI by age, sex, and admission year. Our primary outcome was post-discharge hospitalizations, emergency department, and outpatient physician visits. We calculated adjusted rate ratios (aRR) using negative binomial regression models. We also evaluated physician follow-up (by specialty) and healthcare costs.
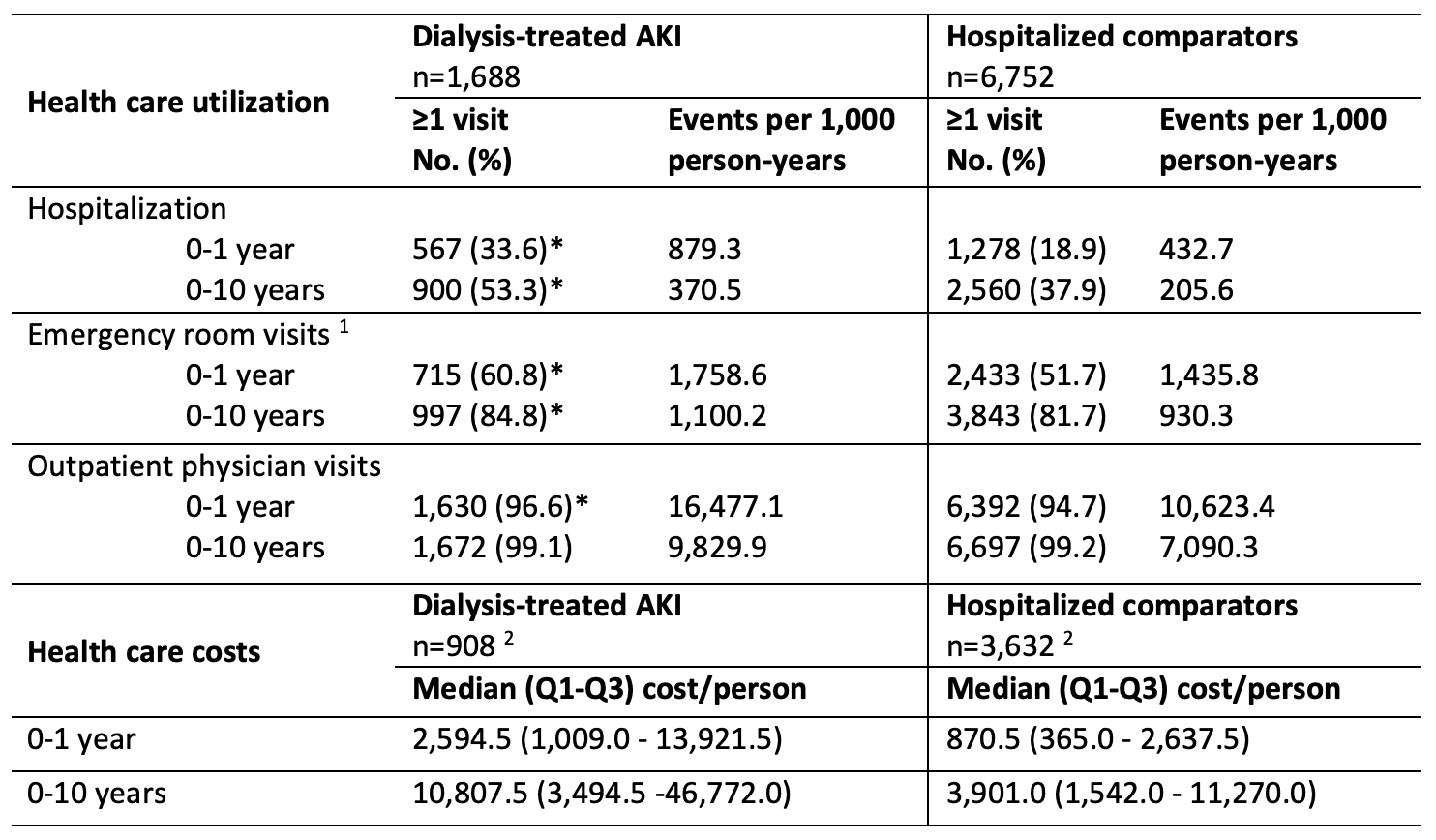
Results: We included 1688 pediatric dialysis-treated AKI survivors and 6752 matched comparators. Dialysis-treated AKI survivors had higher rates of re-hospitalization, emergency department visits, and outpatient physician visits (at 0-1yr, 0-5yr, and 0-10yr; Table). Following adjustment, dialysis-treated AKI survivors had significantly higher rates of re-hospitalization (aRR 1.46 (95% confidence interval (CI) 1.25-1.69, p < 0.0001) and outpatient visits (aRR 1.16 (95%CI 1.09-1.23, p=0.01), but not emergency department visits (aRR 1.10 (95%CI 0.99-1.22, p=0.09). Dialysis-treated AKI survivors also had higher healthcare costs vs. hospitalized comparators throughout follow-up (median $2549 vs. $888 CAD per person-year). Only 18.8% of dialysis-treated AKI survivors had nephrologist follow-up within 1yr post-discharge (Figure), while 92.2% were seen by a family physician or pediatrician in this timeframe. There were no significant differences in post-discharge healthcare utilization or costs between cardiac surgery patients with vs. without dialysis-treated AKI.Conclusion(s): Dialysis-treated AKI survivors had greater post-discharge healthcare utilization and costs vs. hospitalized comparators. Strategies are needed to improve follow-up care for children after dialysis-treated AKI to prevent long-term complications.
Figure. Cumulative incidence of nephrologist visits, among dialysis-treated AKI survivors versus hospitalized comparators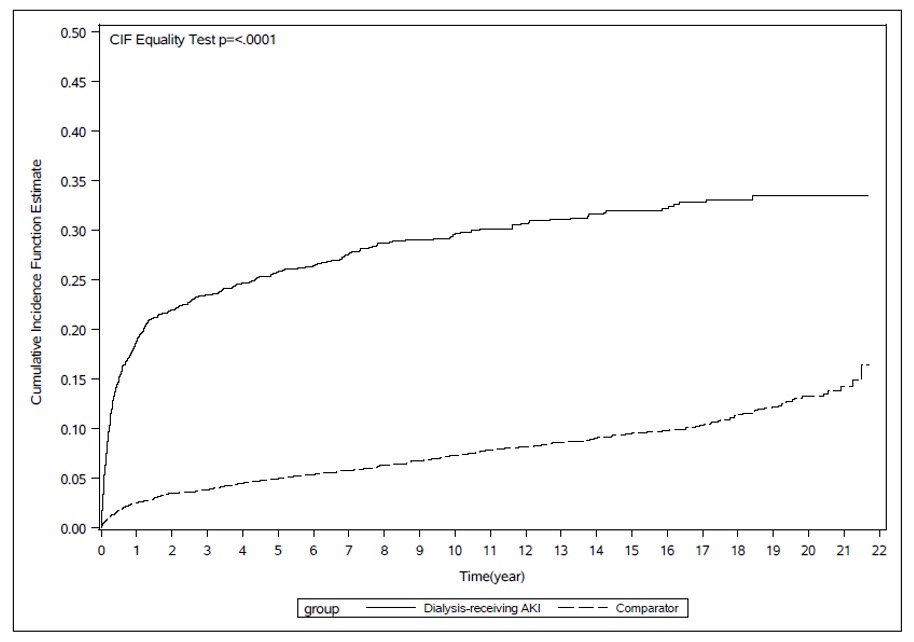 The index date was defined as 104 days post-index hospitalization discharge date. Dialysis-treated AKI survivors experienced nephrologist visits significantly sooner than hospitalized comparators. The greatest difference was observed within the first year after the index date. By 20 years post-hospitalization, only one-third of dialysis-treated AKI survivors had seen a nephrologist.
The index date was defined as 104 days post-index hospitalization discharge date. Dialysis-treated AKI survivors experienced nephrologist visits significantly sooner than hospitalized comparators. The greatest difference was observed within the first year after the index date. By 20 years post-hospitalization, only one-third of dialysis-treated AKI survivors had seen a nephrologist.
Table. Long-term health care utilization and costs among children with dialysis-treated AKI and comparator cohort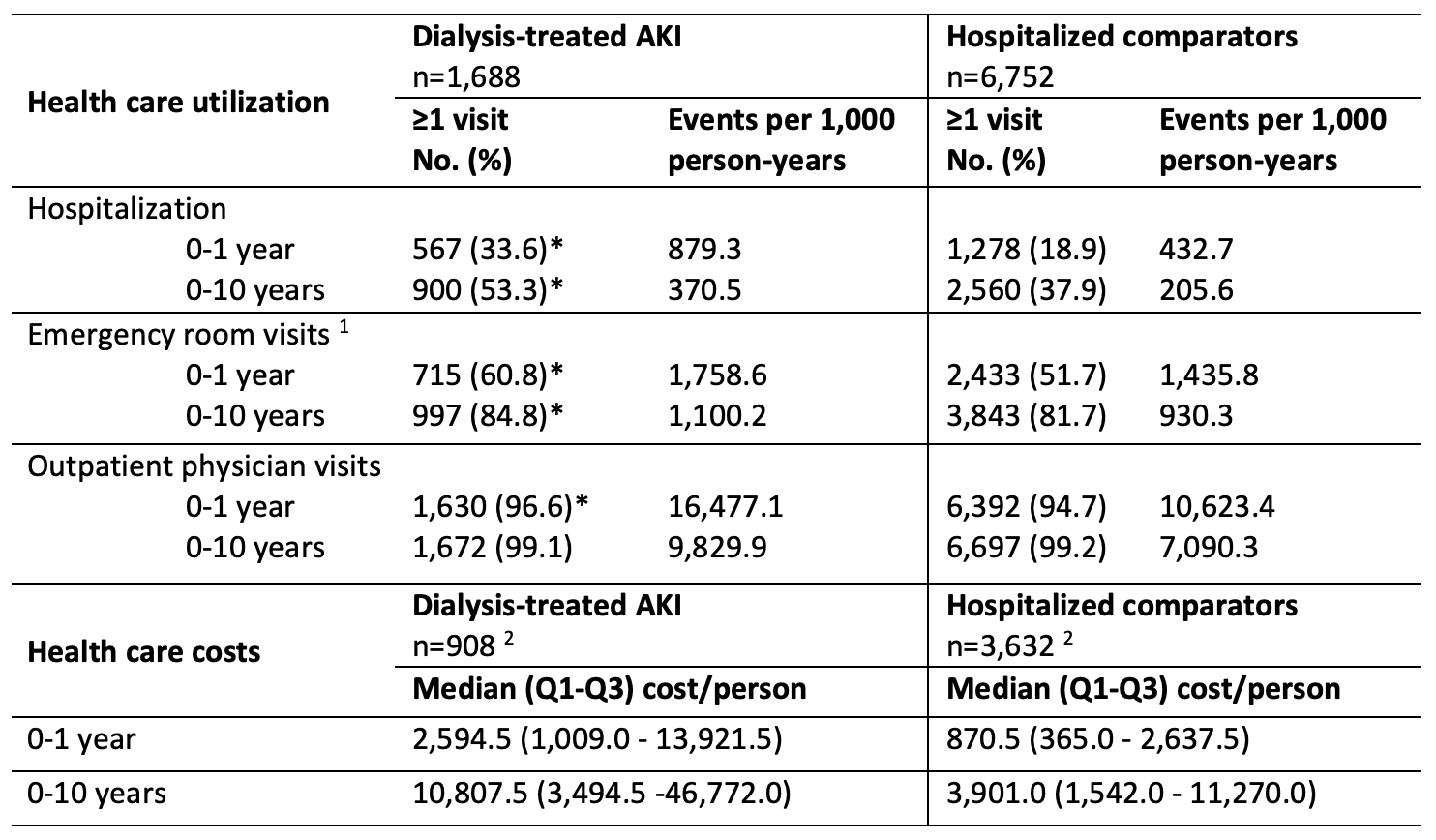 *p-value < 0.05
*p-value < 0.05
CAD: Canadian Dollars
1 Emergency department visit data was available from July 1, 2000 onwards. We therefore restricted analysis of baseline emergency department utilization to those with an index date on or after July 1, 2001 (i.e., one year of baseline utilization data available). This included n = 1,176 and 4,704 for dialysis-recipients and controls, respectively.
2 Cost analysis was restricted to study participants with an index date on or after April 1, 2006, due to incomplete prior costing data.
Objective: To determine long-term healthcare utilization, costs, and physician follow-up patterns after pediatric dialysis-treated AKI hospitalization.
Design/Methods: Using provincial health administrative databases, we performed a retrospective cohort study of all hospitalized pediatric patients (0-18yr) surviving a dialysis-treated AKI episode between 1996-2017 in Ontario, Canada. AKI survivors were matched to four hospitalized comparators without dialysis-treated AKI by age, sex, and admission year. Our primary outcome was post-discharge hospitalizations, emergency department, and outpatient physician visits. We calculated adjusted rate ratios (aRR) using negative binomial regression models. We also evaluated physician follow-up (by specialty) and healthcare costs.
Results: We included 1688 pediatric dialysis-treated AKI survivors and 6752 matched comparators. Dialysis-treated AKI survivors had higher rates of re-hospitalization, emergency department visits, and outpatient physician visits (at 0-1yr, 0-5yr, and 0-10yr; Table). Following adjustment, dialysis-treated AKI survivors had significantly higher rates of re-hospitalization (aRR 1.46 (95% confidence interval (CI) 1.25-1.69, p < 0.0001) and outpatient visits (aRR 1.16 (95%CI 1.09-1.23, p=0.01), but not emergency department visits (aRR 1.10 (95%CI 0.99-1.22, p=0.09). Dialysis-treated AKI survivors also had higher healthcare costs vs. hospitalized comparators throughout follow-up (median $2549 vs. $888 CAD per person-year). Only 18.8% of dialysis-treated AKI survivors had nephrologist follow-up within 1yr post-discharge (Figure), while 92.2% were seen by a family physician or pediatrician in this timeframe. There were no significant differences in post-discharge healthcare utilization or costs between cardiac surgery patients with vs. without dialysis-treated AKI.Conclusion(s): Dialysis-treated AKI survivors had greater post-discharge healthcare utilization and costs vs. hospitalized comparators. Strategies are needed to improve follow-up care for children after dialysis-treated AKI to prevent long-term complications.
Figure. Cumulative incidence of nephrologist visits, among dialysis-treated AKI survivors versus hospitalized comparators
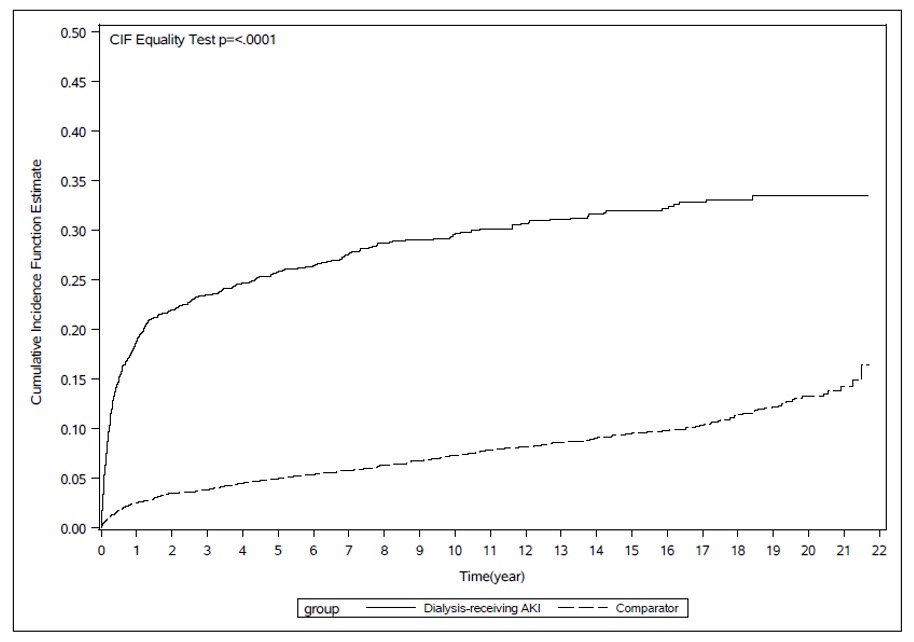 The index date was defined as 104 days post-index hospitalization discharge date. Dialysis-treated AKI survivors experienced nephrologist visits significantly sooner than hospitalized comparators. The greatest difference was observed within the first year after the index date. By 20 years post-hospitalization, only one-third of dialysis-treated AKI survivors had seen a nephrologist.
The index date was defined as 104 days post-index hospitalization discharge date. Dialysis-treated AKI survivors experienced nephrologist visits significantly sooner than hospitalized comparators. The greatest difference was observed within the first year after the index date. By 20 years post-hospitalization, only one-third of dialysis-treated AKI survivors had seen a nephrologist.Table. Long-term health care utilization and costs among children with dialysis-treated AKI and comparator cohort
 *p-value < 0.05
*p-value < 0.05CAD: Canadian Dollars
1 Emergency department visit data was available from July 1, 2000 onwards. We therefore restricted analysis of baseline emergency department utilization to those with an index date on or after July 1, 2001 (i.e., one year of baseline utilization data available). This included n = 1,176 and 4,704 for dialysis-recipients and controls, respectively.
2 Cost analysis was restricted to study participants with an index date on or after April 1, 2006, due to incomplete prior costing data.
