Back
Infectious Diseases
Category: Abstract Submission
Infectious Diseases: Potpourri
550 - Low diagnostic utility of serial tracheal aspirate cultures in the PICU
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 550
Publication Number: 550.328
Publication Number: 550.328
Evin S. Feldman, NewYork-Presbyterian Morgan Stanley Children's Hospital, Long Island City, NY, United States; Shivang Shah, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Danielle Ahn, Columbia University Medical Ce, New York, NY, United States

Evin S. Feldman, MD
Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
Long Island City, New York, United States
Presenting Author(s)
Background: Tracheal aspirate cultures (TACs) are used to aid in the diagnosis and management of Ventilator Associated Infections (VAIs) such as tracheitis and pneumonia. There is evidence that establishing a 72-hour interval between two consecutive TACs safely allows for reassessment of patient clinical status and confirmation of suspected VAI. Despite this, serial TAC sampling is frequently performed in critically ill patients, and is associated with excess antibiotic exposure and the development of resistance. It is not currently evident what new diagnostic information is available to the clinician from TACs repeated within 72 hours of another TAC.
Objective: To determine the diagnostic outcomes of serial TACs repeated within 72 hours in the Pediatric Intensive Care Unit (PICU).
Design/Methods: A retrospective chart review of TAC utilization in the PICU was performed at a single tertiary-care hospital from January 1st to October 31st, 2021. Subjects included were all patients admitted to the PICU for whom a TAC was performed. Items recorded for each TAC included the time and date of culture acquisition, and the result. Additional data, including changes in resistance patterns and/or antibiotic therapy, was also collected.
Results: One-hundred and fifty-five unique subjects had 597 TACs performed during the study time period (Figure 1). One-hundred and fifty-one TACs (25.3%) were repeated within 72-hours of another TAC sent for the same individual subject. Of these cultures, 82 (54.3%) had no growth, 45 (29.8%) grew the same organism as the prior culture, 13 (8.6%) grew a new organism that was previously grown during the admission, and 11 (7.3%) grew a new organism not previously grown during the admission. Six (4.0%) of these TACs repeated within 72-hours displayed significant change in resistance pattern when the same organism was grown, which lead to a change in therapy in 1 (0.7%) instance. A change in therapy when a new organism was grown occurred in 8 (5.3%) instances.Conclusion(s): Serial TAC sampling within 72-hours in the PICU is commonplace and only infrequently yields new data that impacts clinical decision-making. In light of growing antimicrobial resistance and the role that diagnostic stewardship can have to mitigate it, these findings further support a 72-hour reassessment period prior to performing a repeat TAC in critically-ill children.
Figure 1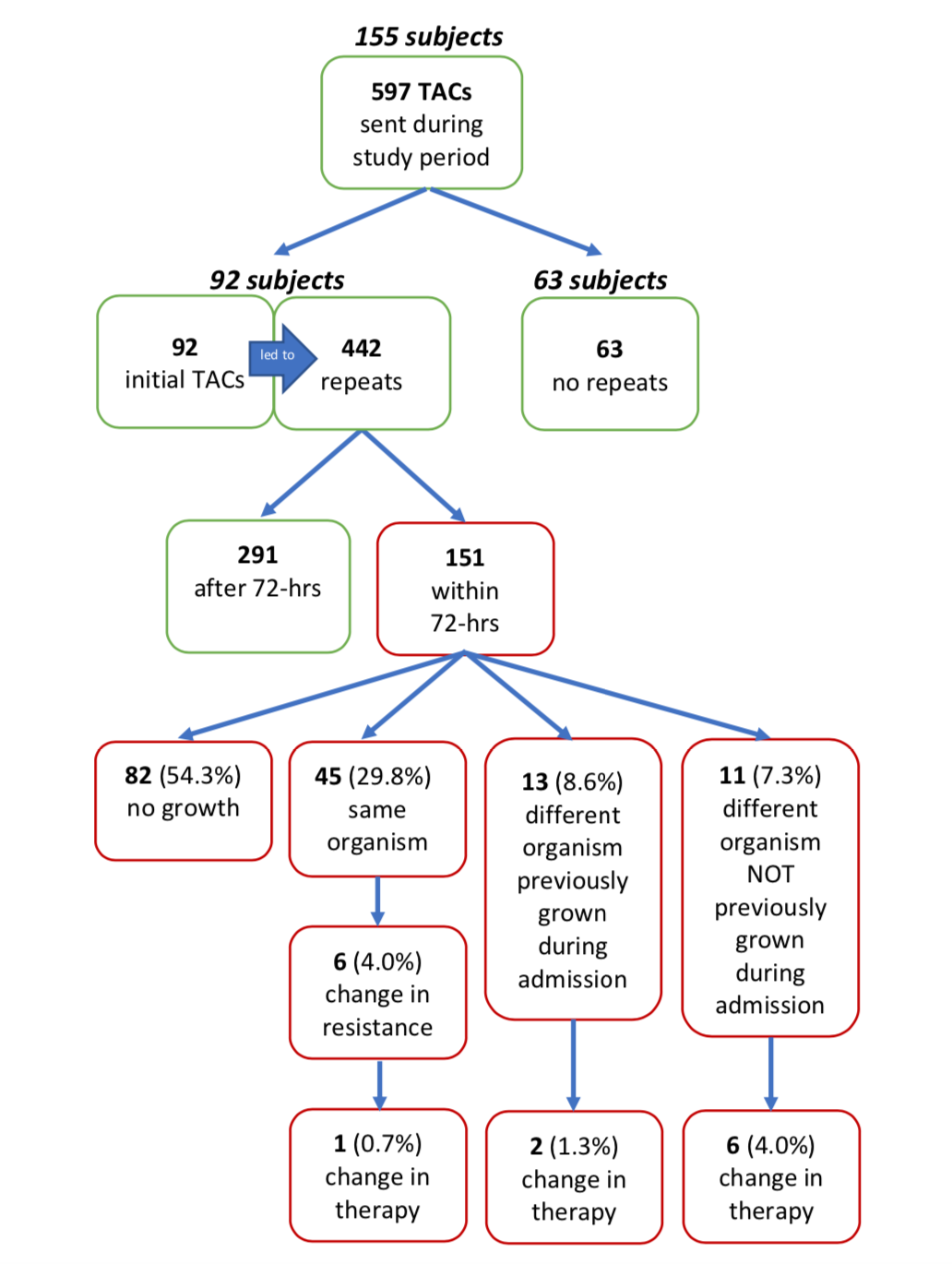 Diagnostic outcomes of tracheal aspirate cultures (TACs). Percentages based off 151 TACs repeated within 72-hours.
Diagnostic outcomes of tracheal aspirate cultures (TACs). Percentages based off 151 TACs repeated within 72-hours.
Objective: To determine the diagnostic outcomes of serial TACs repeated within 72 hours in the Pediatric Intensive Care Unit (PICU).
Design/Methods: A retrospective chart review of TAC utilization in the PICU was performed at a single tertiary-care hospital from January 1st to October 31st, 2021. Subjects included were all patients admitted to the PICU for whom a TAC was performed. Items recorded for each TAC included the time and date of culture acquisition, and the result. Additional data, including changes in resistance patterns and/or antibiotic therapy, was also collected.
Results: One-hundred and fifty-five unique subjects had 597 TACs performed during the study time period (Figure 1). One-hundred and fifty-one TACs (25.3%) were repeated within 72-hours of another TAC sent for the same individual subject. Of these cultures, 82 (54.3%) had no growth, 45 (29.8%) grew the same organism as the prior culture, 13 (8.6%) grew a new organism that was previously grown during the admission, and 11 (7.3%) grew a new organism not previously grown during the admission. Six (4.0%) of these TACs repeated within 72-hours displayed significant change in resistance pattern when the same organism was grown, which lead to a change in therapy in 1 (0.7%) instance. A change in therapy when a new organism was grown occurred in 8 (5.3%) instances.Conclusion(s): Serial TAC sampling within 72-hours in the PICU is commonplace and only infrequently yields new data that impacts clinical decision-making. In light of growing antimicrobial resistance and the role that diagnostic stewardship can have to mitigate it, these findings further support a 72-hour reassessment period prior to performing a repeat TAC in critically-ill children.
Figure 1
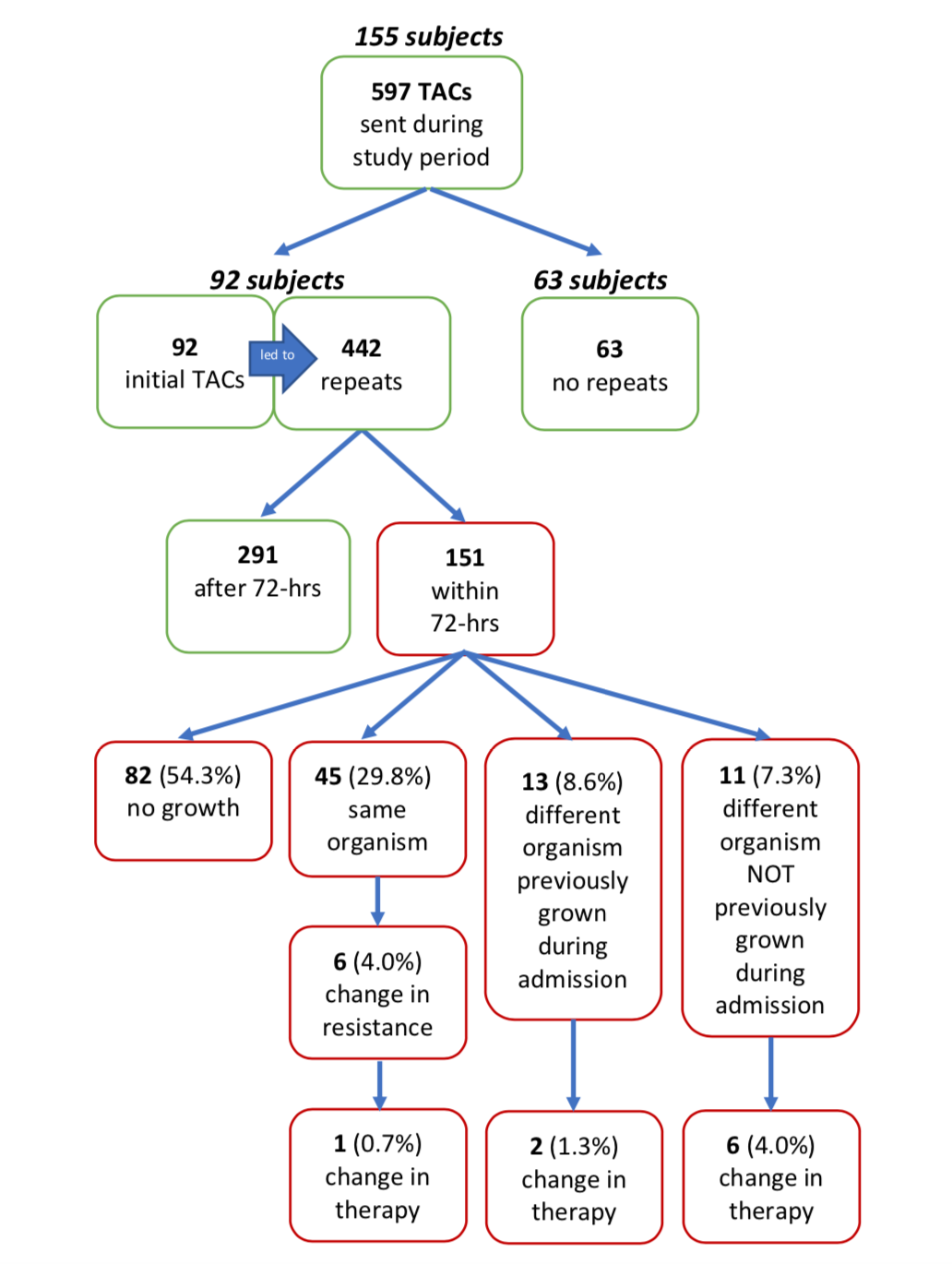 Diagnostic outcomes of tracheal aspirate cultures (TACs). Percentages based off 151 TACs repeated within 72-hours.
Diagnostic outcomes of tracheal aspirate cultures (TACs). Percentages based off 151 TACs repeated within 72-hours.