Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health III
531 - Neonatal respiratory distress and respiratory support utilization at an urban referral hospital in Kenya
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 531
Nora Switchenko, University of Alabama at Birmingham, Homewood, AL, United States; Elizabeth G. Kibaru, Egerton university, Nakuru, Rift Valley, Kenya

Nora Switchenko, MD
Assistant Professor
University of Alabama at Birmingham
Homewood, Alabama, United States
Presenting Author(s)
Background: Respiratory distress (RD) is a common presentation of illness in neonates. Sick newborns with hypoxemia require oxygen supplementation, but many develop respiratory failure that necessitates life-saving respiratory support, including CPAP and/or mechanical ventilation (MV). Knowledge of the epidemiology of newborns with RD in low-resource settings will help stakeholders to adapt clinical practice guidelines and implement programs geared towards delivering high quality, effective respiratory support to sick newborns worldwide.
Objective: Describe the rates of respiratory distress and the rate of utilization of respiratory support resources by term and preterm infants at the Nakuru Country and Referral Hospital in Nakuru, Kenya.
Design/Methods: Medical records of neonates treated at the Nakuru Country and Referral Hospital between 2018 and 2019 were reviewed. The frequency at which term and preterm neonates presented after birth with RD and the numbers treated with oxygen via cannula, CPAP, and MV were obtained. The study center has equipment for all levels of respiratory support, however lacks personnel trained to provide MV to newborns. Preterm was defined by documentation of estimated gestational age (EGA) at < 37 weeks. If EGA was not documented, preterm was defined by birthweight < 2.5 kg. Respiratory distress was defined by documentation of increased work of breathing (chest wall indrawing, retractions, or grunting) or hypoxemia (oxygen saturation under 90 percent). Proportions were compared by chi square.
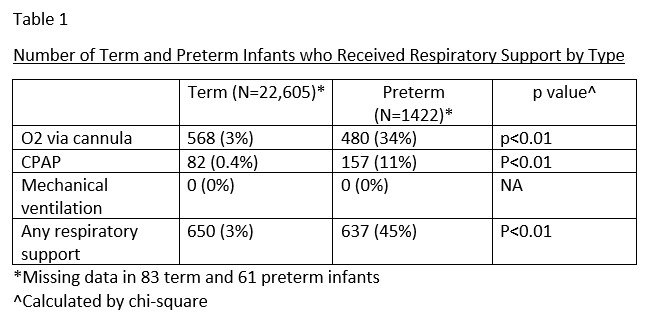
Results: There were 24,171 deliveries during the study period (22,688 term, 1483 preterm). 515 term (2%) and 490 preterm (33%) had RD. A greater number of term infants received oxygen via nasal cannula and a greater number preterm infants received CPAP (Table 1). No infants were treated with MV. 2701 sick infants were admitted to the hospital’s newborn unit (NBU). The pre-discharge mortality of infants admitted to the NBU was 14% (375/2693) overall, and 27% (268/1004) in the group with RD. Of the infants admitted to NBU, RD was associated with mortality in both term (p < 0.01) and preterm (p < 0.01) infants.Conclusion(s): Respiratory distress is common in both term and preterm neonates. Use of advanced respiratory support was low. Variable access to and low utilization of respiratory support therapies in resource-limited settings may contribute to preventable neonatal deaths.
Table 1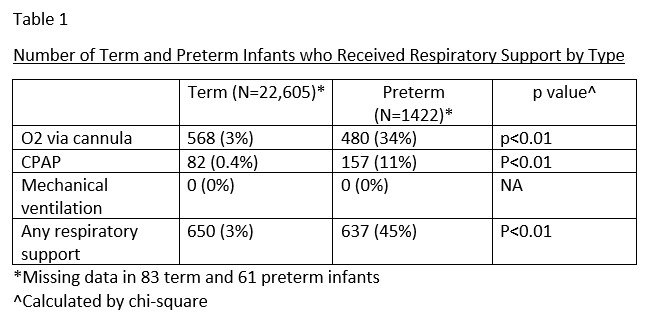
Objective: Describe the rates of respiratory distress and the rate of utilization of respiratory support resources by term and preterm infants at the Nakuru Country and Referral Hospital in Nakuru, Kenya.
Design/Methods: Medical records of neonates treated at the Nakuru Country and Referral Hospital between 2018 and 2019 were reviewed. The frequency at which term and preterm neonates presented after birth with RD and the numbers treated with oxygen via cannula, CPAP, and MV were obtained. The study center has equipment for all levels of respiratory support, however lacks personnel trained to provide MV to newborns. Preterm was defined by documentation of estimated gestational age (EGA) at < 37 weeks. If EGA was not documented, preterm was defined by birthweight < 2.5 kg. Respiratory distress was defined by documentation of increased work of breathing (chest wall indrawing, retractions, or grunting) or hypoxemia (oxygen saturation under 90 percent). Proportions were compared by chi square.
Results: There were 24,171 deliveries during the study period (22,688 term, 1483 preterm). 515 term (2%) and 490 preterm (33%) had RD. A greater number of term infants received oxygen via nasal cannula and a greater number preterm infants received CPAP (Table 1). No infants were treated with MV. 2701 sick infants were admitted to the hospital’s newborn unit (NBU). The pre-discharge mortality of infants admitted to the NBU was 14% (375/2693) overall, and 27% (268/1004) in the group with RD. Of the infants admitted to NBU, RD was associated with mortality in both term (p < 0.01) and preterm (p < 0.01) infants.Conclusion(s): Respiratory distress is common in both term and preterm neonates. Use of advanced respiratory support was low. Variable access to and low utilization of respiratory support therapies in resource-limited settings may contribute to preventable neonatal deaths.
Table 1