Neonatal General
Category: Abstract Submission
Neonatology General 8: Health Disparities - Health Services Research
221 - Potential Cost Savings Associated With Bubble Continuous Positive Airway Pressure In Neonates: A Retrospective Study
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 221
Publication Number: 221.339
Publication Number: 221.339
Shelbye Schweinhart, University of Louisville School of Medicine, Louisville, KY, United States; Yana Feygin, University of Louisville School of Medicine, Louisville, KY, United States; Scott C. Duncan, University fo Louisville, Louisville, KY, United States; Hannah Fischer, University of Louisville School of Medicine, Louisville, KY, United States

Hannah Fischer, MD
Associate Professor
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background: Bubble continuous positive airway pressure (bCPAP) is a well-established non-invasive respiratory support mechanism in preterm infants which decreases rates of mechanical ventilation, and bronchopulmonary dysplasia (BPD) and death. Heated high flow nasal cannula (HFNC) is another form of noninvasive respiratory support, lacking evidence for its use as a primary mode of support in neonates.
Objective: We propose that there are cost savings with the implementation of bCPAP as an alternative to HFNC, without a detrimental effect on outcomes.
Design/Methods: Data was collected in the context of a QI project and approved as not human subjects research. Infants admitted to our NICU in 2020 with a birthweight (BW) less than 1500g or gestational age less than 32 weeks were included. Infants were excluded if they expired or required tracheostomy prior to discharge or did not require bCPAP or HFNC support. Days of each method of respiratory support, respiratory charges and clinical outcomes were collected. Patients were divided into groups based upon the percentage of non-invasive ventilation days spent on bCPAP. Group A had the lowest proportion of bCPAP days, while group D had the highest. Charges were converted to cost by utilizing the institution specific 2020 cost to charge ratio from the Kentucky Labor Cabinet. Respiratory costs were calculated and potential cost savings estimated by converting applied costs for HFNC to bCPAP. Descriptive statistics were used to compare groups; p-values for continuous variables calculated based on Kruskal-Wallis rank sum test, and Chi-square test for difference in proportions of BPD.
Results: A total of 110 patients were included in the final analysis and grouped based on the percentage of days with bCPAP as noninvasive respiratory support (Figure 1). Patients in group A with the least amount of bCPAP use had greater ventilator days; conversely, group D with the highest proportion of bCPAP use, had lower number of ventilator days (p < 0.001). Rates of BPD and LOS decreased significantly between groups as the percentage of bCPAP days increased (p=0.001; p < 0.001). There was a trend towards lower respiratory costs as the percentage of bCPAP days increased. There was an average potential cost savings of $1675 per patient if noninvasive ventilation days were converted from HFNC to bCPAP (p < 0.001).Conclusion(s): As NICU respiratory practices evolve to focus on reducing rates of BPD, morbidity, and mortality, costs of common strategies should be considered. Protocols prioritizing the use of bCPAP show potential cost reduction in addition to previously recognized clinical benefit.
Respiratory, Cost and Clinical Outcomes Grouped by Percentage of Days with BCPAP as Noninvasive Respiratory Support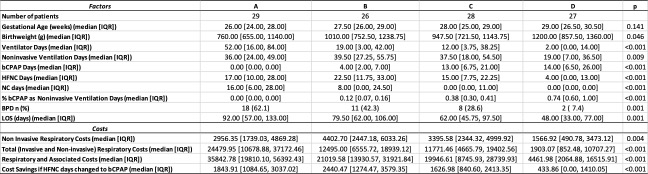
Median and Interquartile Ranges for Length of Stay and Respiratory Costs.jpg)
Objective: We propose that there are cost savings with the implementation of bCPAP as an alternative to HFNC, without a detrimental effect on outcomes.
Design/Methods: Data was collected in the context of a QI project and approved as not human subjects research. Infants admitted to our NICU in 2020 with a birthweight (BW) less than 1500g or gestational age less than 32 weeks were included. Infants were excluded if they expired or required tracheostomy prior to discharge or did not require bCPAP or HFNC support. Days of each method of respiratory support, respiratory charges and clinical outcomes were collected. Patients were divided into groups based upon the percentage of non-invasive ventilation days spent on bCPAP. Group A had the lowest proportion of bCPAP days, while group D had the highest. Charges were converted to cost by utilizing the institution specific 2020 cost to charge ratio from the Kentucky Labor Cabinet. Respiratory costs were calculated and potential cost savings estimated by converting applied costs for HFNC to bCPAP. Descriptive statistics were used to compare groups; p-values for continuous variables calculated based on Kruskal-Wallis rank sum test, and Chi-square test for difference in proportions of BPD.
Results: A total of 110 patients were included in the final analysis and grouped based on the percentage of days with bCPAP as noninvasive respiratory support (Figure 1). Patients in group A with the least amount of bCPAP use had greater ventilator days; conversely, group D with the highest proportion of bCPAP use, had lower number of ventilator days (p < 0.001). Rates of BPD and LOS decreased significantly between groups as the percentage of bCPAP days increased (p=0.001; p < 0.001). There was a trend towards lower respiratory costs as the percentage of bCPAP days increased. There was an average potential cost savings of $1675 per patient if noninvasive ventilation days were converted from HFNC to bCPAP (p < 0.001).Conclusion(s): As NICU respiratory practices evolve to focus on reducing rates of BPD, morbidity, and mortality, costs of common strategies should be considered. Protocols prioritizing the use of bCPAP show potential cost reduction in addition to previously recognized clinical benefit.
Respiratory, Cost and Clinical Outcomes Grouped by Percentage of Days with BCPAP as Noninvasive Respiratory Support
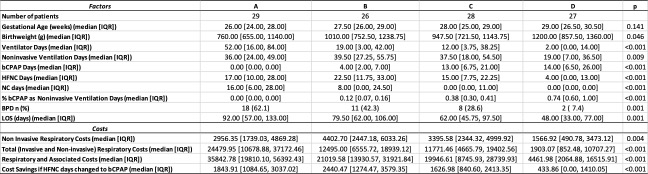
Median and Interquartile Ranges for Length of Stay and Respiratory Costs
.jpg)
