Back
Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 5: Neonatal Neurology Term Clinical
482 - Predictive value of serially obtained aEEG from neonates with HIE who were treated with therapeutic hypothermia: A report from the Baby Cooling Registry of Japan during the period of 2014-2017
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 482
Yuichiro Sugiyama, Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital, Nagoya, Aichi, Japan; Kennosuke tsuda, Nagoya City University, Nagoya, Aichi, Japan; Jun Shibasaki, Kanagawa Childrens' Medical Center, Yokohama, Kanagawa, Japan; Akihito Takeuchi, National Hospital Organization Okayama Medical Center, Okayama, Okayama, Japan; Osuke Iwata, Nagoya City University, Nagoya, Aichi, Japan
.jpg)
Yuichiro Sugiyama, MD, PhD
Chief Doctor
Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital
Nagoya, Aichi, Japan
Presenting Author(s)
Background: Amplitude-integrated electroencephalography (aEEG) is an established prognostic biomarker of neonates with hypoxic-ischemic encephalopathy (HIE), however, the optimal timing of aEEG recording needs to be elucidated in a large-scale cohort.
Objective: To elucidate the temporal change of predictive values of aEEG for the outcome of neonates who were treated with therapeutic hypothermia in a large cohort of HIE neonates.
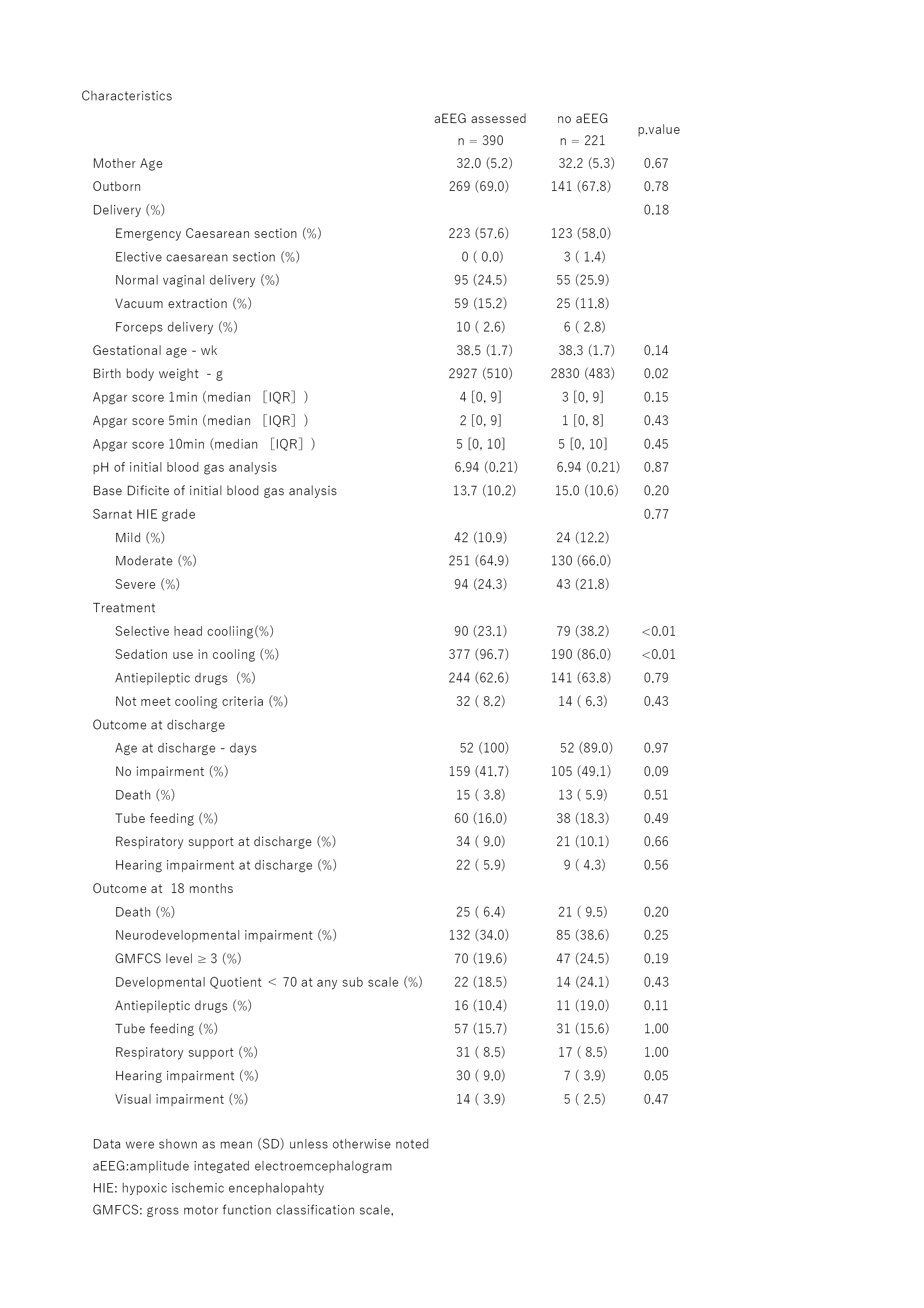
Design/Methods: Using data from 611 neonates born between 2014 and 2017 who were registered to the Baby Cooling Registry of Japan, we examined aEEG findings, that were recorded every 24 hours during 72-hour-cooling; predictive values of aEEG at 0, 24, 48 and 72 hours of cooling with the outcome of the neonates at 18 months of age were assessed. The aEEG findings were classified as normal, mild to moderate depression, severe depression (upper margin < 10 μV and lower margin < 5 μV), or convulsive by clinicians at each facility following a brief tuition. Severely depressed and convulsive aEEG findings were binned as severe aEEG abnormalities.
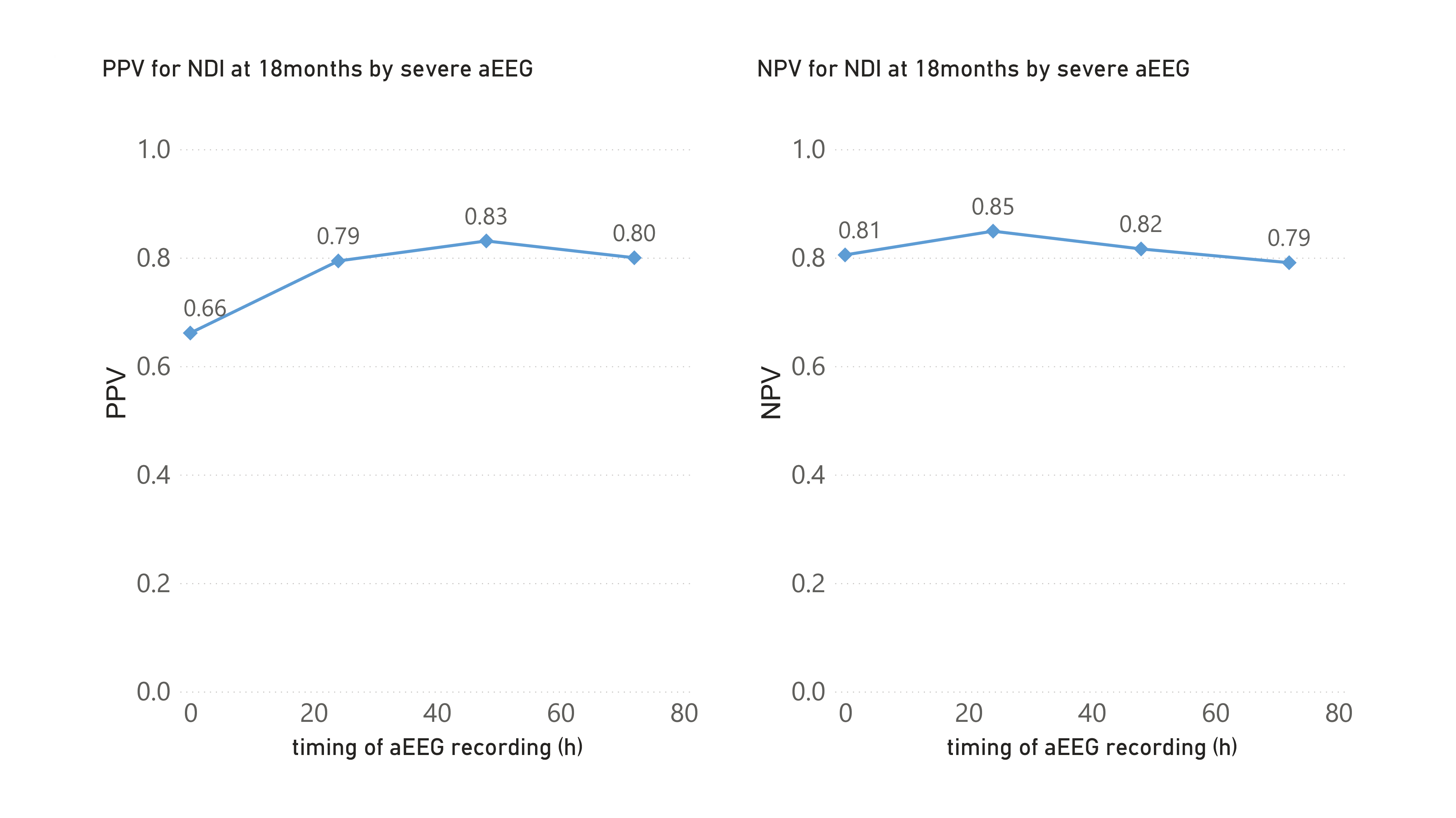
The neurodevelopmental impairment (NDI) at 18 months of age was the presence of at least one of followings; death, gross motor function classification system level ≥ 3, manual ability classification system level ≥ 3, Kyoto Scale of Psychological Developmental Quotient score of < 70 at any sub scale, deafness, visual impairment, tube feeding and respiratory support. Positive (PPV) and negative predictive value (NPV) for NDI at 18 months of age were calculated based on the presence of severe aEEG abnormality at each recording time.
Results: Of the 611 cases, serial aEEG records and outcome data at 18 months of age were available in 390 neonates. Of these, 132 (34%) had NDI at 18 months of age. Neonates within the final study cohort had significantly higher birth weights, lower sedation rates, and were treated less with selective head cooling than those excluded; however, there was no difference in the Sarnat encephalopathy grade and outcomes except that hearing impairment was more frequently observed in neonates within the study cohort. Severe aEEG abnormality predicted NDI at 18 months of age at 0, 24, 48, and 72 hours of cooling with PPVs of 0.66, 0.79, 0.83, and 0.80 and NPVs of 0.81, 0.85, 0.82, and 0.79, respectively.Conclusion(s): In a large cohort of neonates with HIE who were treated with therapeutic hypothermia, severe aEEG abnormality predicted NDI at 18 months of age with convincingly high positive and negative predictive values. There was a trend that the PPV increased from 0 to 24 hours of treatment and remained unchanged thereafter.
Characteristics of the patient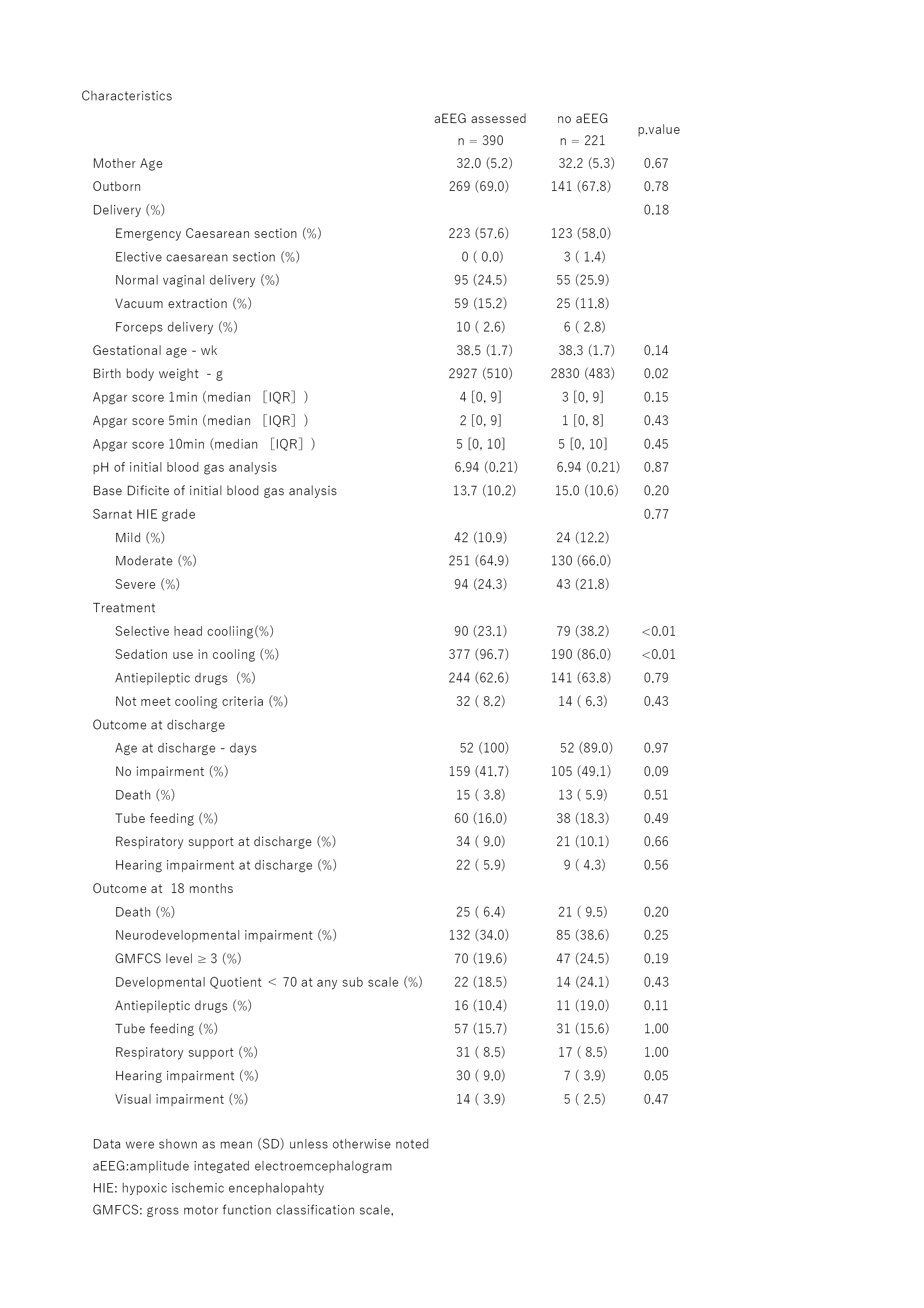
PPV and NPV for NDI at 18 months of age by severe aEEG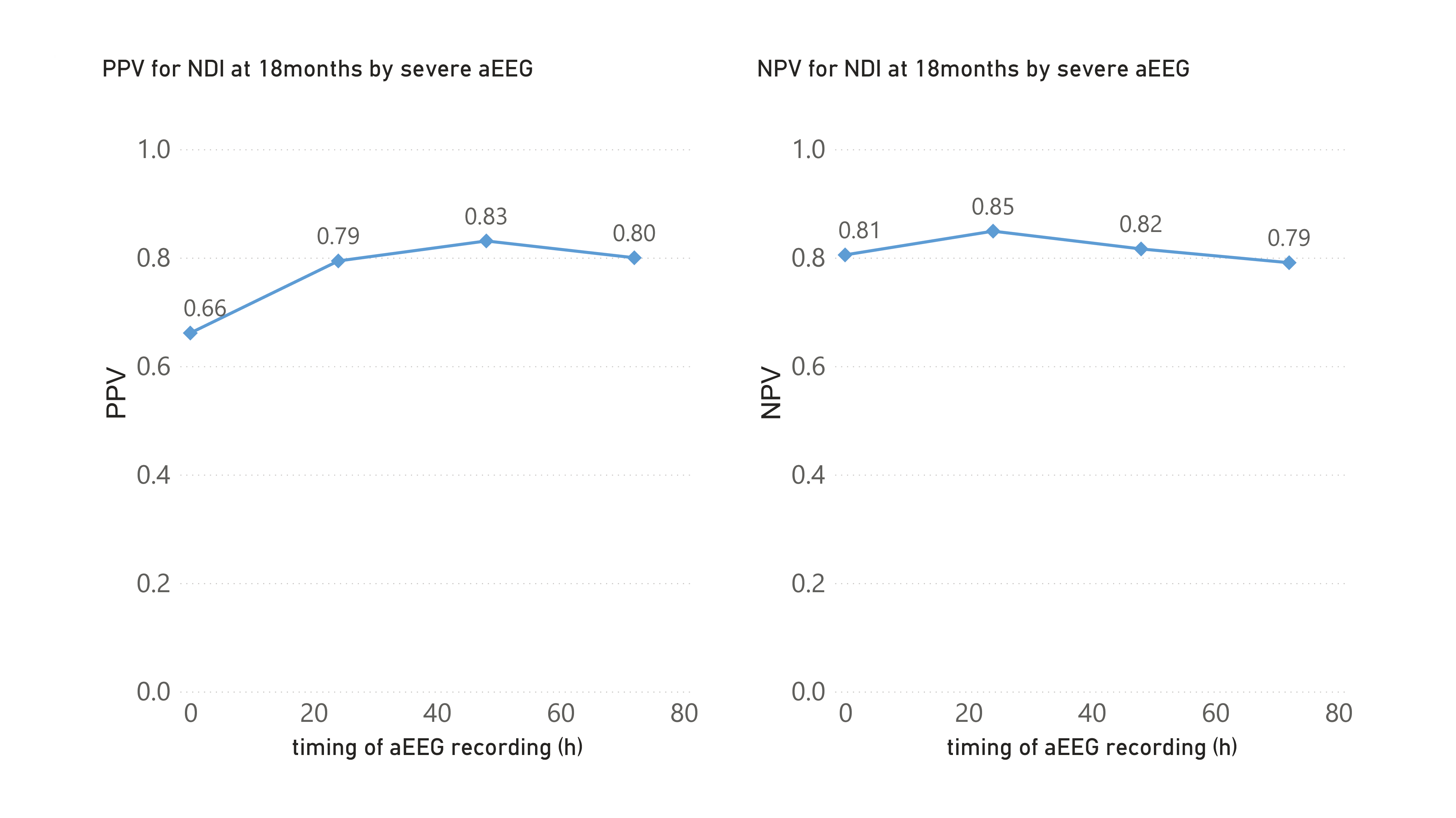
Objective: To elucidate the temporal change of predictive values of aEEG for the outcome of neonates who were treated with therapeutic hypothermia in a large cohort of HIE neonates.
Design/Methods: Using data from 611 neonates born between 2014 and 2017 who were registered to the Baby Cooling Registry of Japan, we examined aEEG findings, that were recorded every 24 hours during 72-hour-cooling; predictive values of aEEG at 0, 24, 48 and 72 hours of cooling with the outcome of the neonates at 18 months of age were assessed. The aEEG findings were classified as normal, mild to moderate depression, severe depression (upper margin < 10 μV and lower margin < 5 μV), or convulsive by clinicians at each facility following a brief tuition. Severely depressed and convulsive aEEG findings were binned as severe aEEG abnormalities.
The neurodevelopmental impairment (NDI) at 18 months of age was the presence of at least one of followings; death, gross motor function classification system level ≥ 3, manual ability classification system level ≥ 3, Kyoto Scale of Psychological Developmental Quotient score of < 70 at any sub scale, deafness, visual impairment, tube feeding and respiratory support. Positive (PPV) and negative predictive value (NPV) for NDI at 18 months of age were calculated based on the presence of severe aEEG abnormality at each recording time.
Results: Of the 611 cases, serial aEEG records and outcome data at 18 months of age were available in 390 neonates. Of these, 132 (34%) had NDI at 18 months of age. Neonates within the final study cohort had significantly higher birth weights, lower sedation rates, and were treated less with selective head cooling than those excluded; however, there was no difference in the Sarnat encephalopathy grade and outcomes except that hearing impairment was more frequently observed in neonates within the study cohort. Severe aEEG abnormality predicted NDI at 18 months of age at 0, 24, 48, and 72 hours of cooling with PPVs of 0.66, 0.79, 0.83, and 0.80 and NPVs of 0.81, 0.85, 0.82, and 0.79, respectively.Conclusion(s): In a large cohort of neonates with HIE who were treated with therapeutic hypothermia, severe aEEG abnormality predicted NDI at 18 months of age with convincingly high positive and negative predictive values. There was a trend that the PPV increased from 0 to 24 hours of treatment and remained unchanged thereafter.
Characteristics of the patient
PPV and NPV for NDI at 18 months of age by severe aEEG