Telemedicine/EHR/Medical Informatics
Category: Abstract Submission
Telemedicine/EHR/Medical Informatics II
301 - Premedication for Neonatal Endotracheal Intubation: Barriers to Provider Driven Reporting with the Electronic Medical Record
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 301
Publication Number: 301.347
Publication Number: 301.347
Ameena N. Husain, Washington University in St. Louis School of Medicine, St Louis, MO, United States; Zachary A. Vesoulis, Washington University School of Medicine, St. Louis, MO, United States; Christopher McPherson, St. Louis Children's Hospital, St. Louis, MO, United States

Ameena N. Husain, DO
Clinical Fellow
Washington University in St. Louis School of Medicine
St Louis, Missouri, United States
Presenting Author(s)
Background: Neonatal endotracheal intubation is a common, high-risk procedure with possible adverse effects such as pain, bradycardia, oxygen desaturation, and airway injury. Cardiorespiratory compromise during intubation increases the risk of preterm brain injury. As a result, analgesia premedication with or without paralytic agents is indicated prior to non-emergent intubation. However, premedication usage rates vary widely, and the impact on outcomes remains unclear. Inaccessibility of data and lack of reporting standards in the electronic medical record (EMR) are a significant barrier to widespread, data-driven premedication practices.
Objective: To develop a report using the EMR to accurately capture premedication usage rates for all non-emergent intubations and evaluate the impact on number of attempts and adverse events.
Design/Methods: All term and preterm infants admitted to the NICU at Saint Louis Children’s Hospital who underwent intubation between January 2021 and December 2021 were identified. Intubations were classified as emergent (excluded) or non-emergent (included). The EMR tool SlicerDicer was used to generate a customized data report which extracted standard clinical characteristics, medication exposure, and procedure details (number of intubation attempts and complications).
Results: A total of 237 non-emergent intubations were included. Procedures were divided into groups based on type of premedication, and results are summarized in Table 1. 88% of infants were provided analgesia, and 40% were given a paralytic. Use of paralytics was associated with a reduction in number of attempts from 1.8 to 1.6 (p < 0.01).
Several EMR barriers were identified during data collection. The default reporting tool lacked neonatal specific columns (e.g., gestational age, birth weight). Additionally, inconsistencies were identified in provider documentation including time of procedure, encounter information, intubation indication, and presence/absence of vital sign changes. Other event and nursing documentation was manually reviewed to ensure accurate data collection.Conclusion(s): Premedication for neonatal intubations may decrease risk of adverse effects in neonates. However, barriers within EMR documentation limit local and national efforts for quality improvement in this area. Standardization of documentation and reporting tools within the EMR will greatly improve the ability for providers to perform meaningful quality improvement work in this area and others.
Non-Emergent Intubation Procedures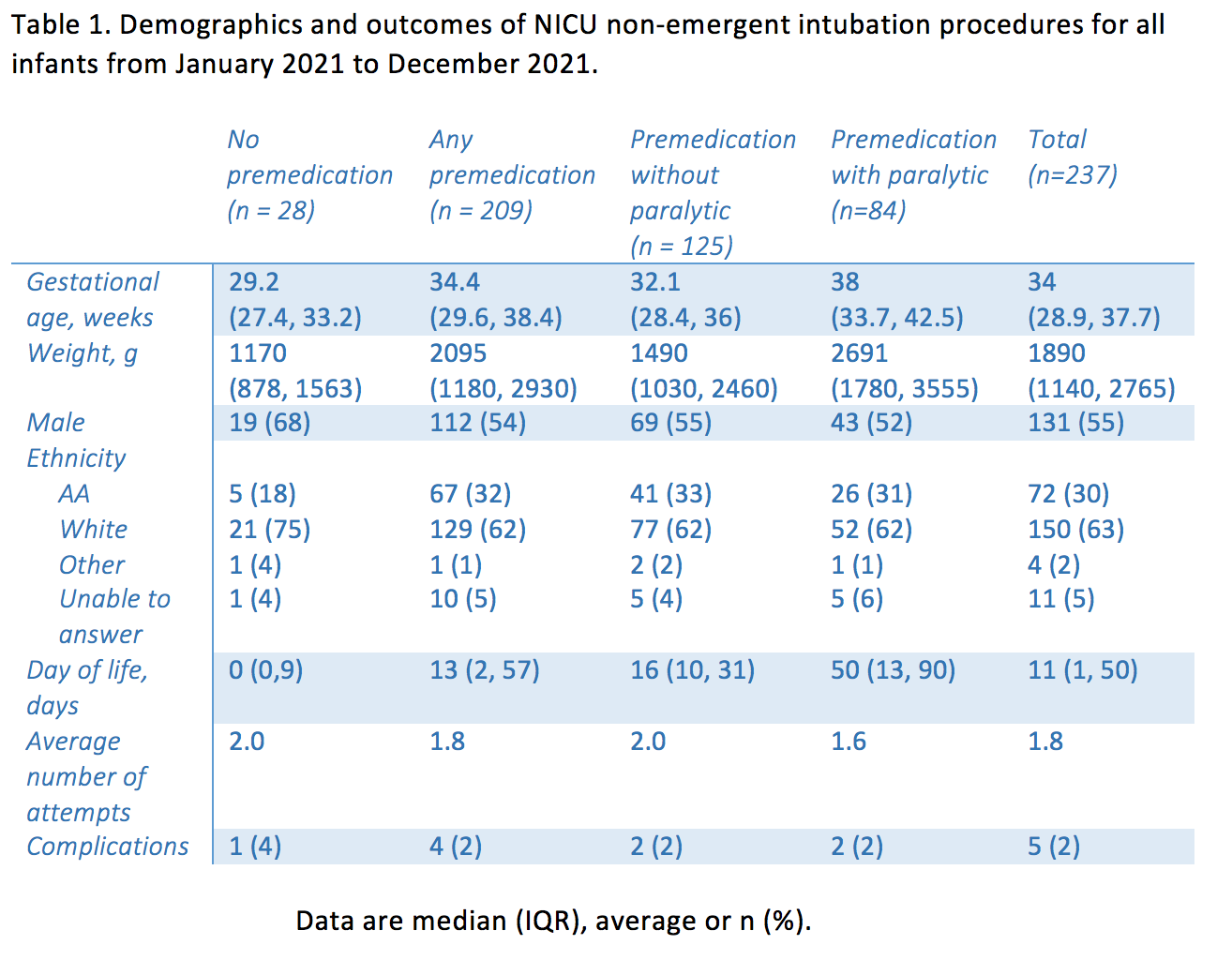 Table 1. Demographics and outcomes of NICU non-emergent intubation procedures for all infants from January 2021 to December 2021.
Table 1. Demographics and outcomes of NICU non-emergent intubation procedures for all infants from January 2021 to December 2021.
Objective: To develop a report using the EMR to accurately capture premedication usage rates for all non-emergent intubations and evaluate the impact on number of attempts and adverse events.
Design/Methods: All term and preterm infants admitted to the NICU at Saint Louis Children’s Hospital who underwent intubation between January 2021 and December 2021 were identified. Intubations were classified as emergent (excluded) or non-emergent (included). The EMR tool SlicerDicer was used to generate a customized data report which extracted standard clinical characteristics, medication exposure, and procedure details (number of intubation attempts and complications).
Results: A total of 237 non-emergent intubations were included. Procedures were divided into groups based on type of premedication, and results are summarized in Table 1. 88% of infants were provided analgesia, and 40% were given a paralytic. Use of paralytics was associated with a reduction in number of attempts from 1.8 to 1.6 (p < 0.01).
Several EMR barriers were identified during data collection. The default reporting tool lacked neonatal specific columns (e.g., gestational age, birth weight). Additionally, inconsistencies were identified in provider documentation including time of procedure, encounter information, intubation indication, and presence/absence of vital sign changes. Other event and nursing documentation was manually reviewed to ensure accurate data collection.Conclusion(s): Premedication for neonatal intubations may decrease risk of adverse effects in neonates. However, barriers within EMR documentation limit local and national efforts for quality improvement in this area. Standardization of documentation and reporting tools within the EMR will greatly improve the ability for providers to perform meaningful quality improvement work in this area and others.
Non-Emergent Intubation Procedures
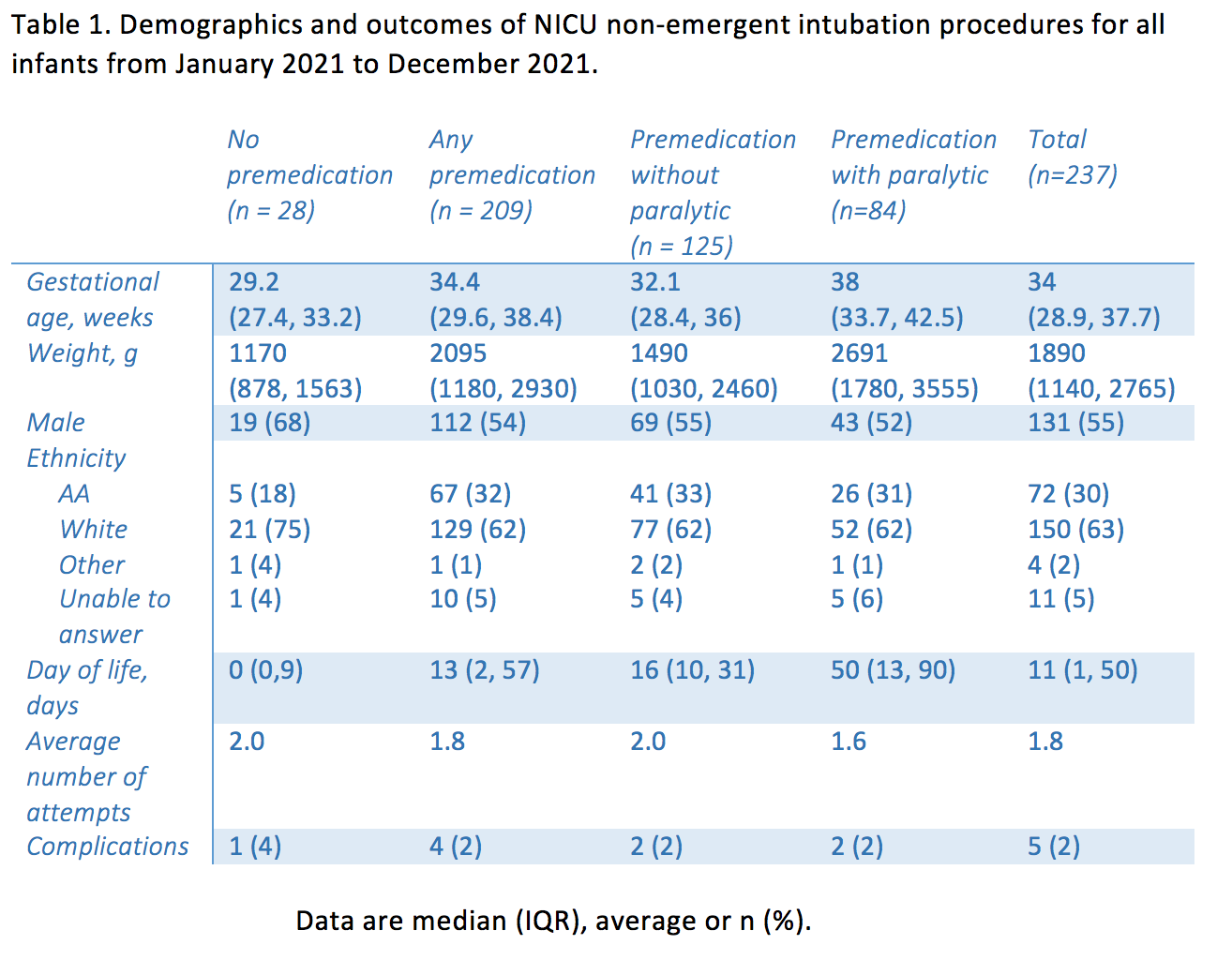 Table 1. Demographics and outcomes of NICU non-emergent intubation procedures for all infants from January 2021 to December 2021.
Table 1. Demographics and outcomes of NICU non-emergent intubation procedures for all infants from January 2021 to December 2021.