Back
Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VIII
361 - Racial and ethnic differences in low-value pediatric emergency care
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 361
Joyce Li, Boston Children's Hospital, Boston, MA, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Jennifer Marin, UPMC Childrens Hospital of Pittsburgh, PIttsburgh, PA, United States
- JL
Joyce Li, MD MPH (she/her/hers)
Assistant Professor in Pediatrics and Emergency Medicine
Boston Children's Hospital
Medford, Massachusetts, United States
Presenting Author(s)
Background: Disparities in health care quality are well described but historically focused on underuse. Over-testing and treatment can result in patient harm.
Objective: We sought to evaluate racial and ethnic differences in low-value services delivered in the pediatric emergency department (ED).
Design/Methods: We performed a retrospective cross-sectional study of low-value services in children discharged from 39 pediatric EDs from January 2018 - December 2019 using the Pediatric Health Information System. Our primary outcome was receipt of one of 12 low-value services across 9 conditions, including: chest radiography in asthma and bronchiolitis, beta agonist and corticosteroids in bronchiolitis, laboratory testing and neuroimaging in febrile seizure, neuroimaging in afebrile seizure, head injury and headache, and any imaging in sinusitis, constipation and facial trauma. We analyzed the association of race and ethnicity on receipt of low-value services using generalized linear mixed models.
Results: There were 4,676,802 patients in the final study cohort. For each condition, most patients were non-Hispanic White, with the exception of asthma (Table 1). Chest radiography for asthma and bronchiolitis, neuroimaging for head injury and headache, and imaging for constipation were more prevalent among non-Hispanic White patients (Table 2). Compared with non-Hispanic White (NHW) patients, non-Hispanic Black (NHB) and Hispanic patients had lower adjusted odds (aOR, 95% confidence interval) of receiving imaging for asthma (0.60, 0.56-0.63 NHB; 0.84, 0.79-0.89 Hispanic); bronchiolitis (0.84, 0.79-0.89 NHB; 0.93, 0.88-0.99 Hispanic); head injury (0.84, 0.80-0.88 NHB; 0.80, 0.76-0.84 Hispanic); headache (0.67, 0.63-0.72 NHB; 0.83, 0.78-0.88 Hispanic); and constipation (0.71, 0.67-0.74 NHB; 0.76, 0.72-0.80 Hispanic). NHB patients had lower odds of receiving imaging for afebrile seizures (0.89, 0.8-1.0) and facial trauma (0.69, 0.60-0.80); and Hispanic patients had lower odds of imaging (0.57, 0.36-0.90) and blood testing (0.82, 0.69-0.98) for febrile seizures. NHB patients had higher odds of receiving steroids (1.11, 1.00-1.21) and beta-agonists (1.38, 1.24-1.54) for bronchiolitis compared with NHW patients (Figure 2).Conclusion(s): NHW patients are more likely to receive low-value imaging while NHB patients are more likely to receive low-value medications for bronchiolitis. Our study demonstrates that racial and ethnic differences care extend to many services including those of low-value, highlighting the importance of greater understanding on the complexities of race and ethnicity on clinical practice.
Table 1. Patient Characteristics, by Condition.jpg) a American Indian, Asian, Native Hawaiian, multiracial, other race/ethnicity
a American Indian, Asian, Native Hawaiian, multiracial, other race/ethnicity
b Includes self-pay, charity, hospital did not bill, and other
Table 2. Prevalence of Low-Value Services, by Race/Ethnicity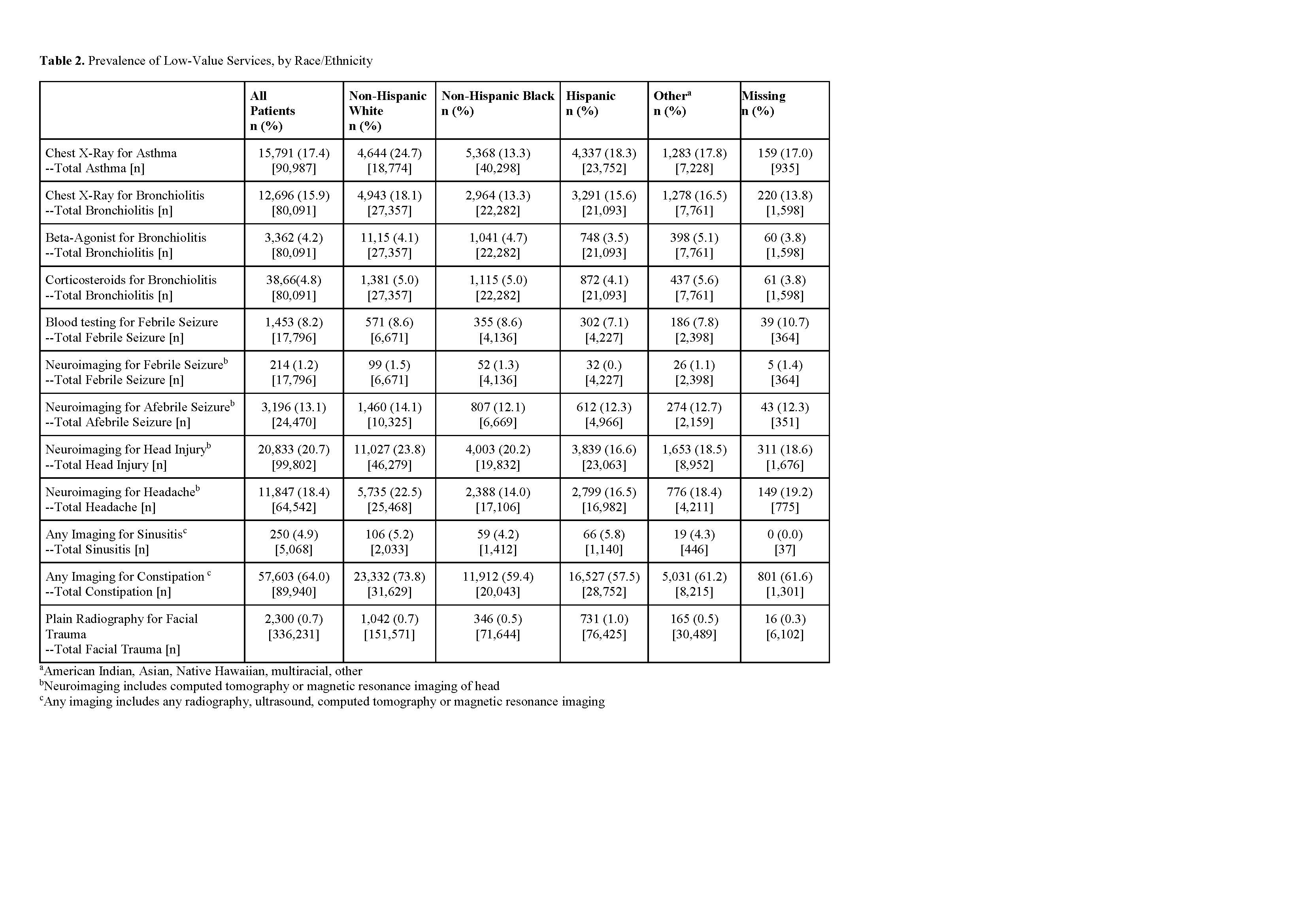 a American Indian, Asian, Native Hawaiian, multiracial, other
a American Indian, Asian, Native Hawaiian, multiracial, other
b Neuroimaging includes computed tomography or magnetic resonance imaging of head
c Any imaging includes any radiography, ultrasound, computed tomography or magnetic resonance imaging
Objective: We sought to evaluate racial and ethnic differences in low-value services delivered in the pediatric emergency department (ED).
Design/Methods: We performed a retrospective cross-sectional study of low-value services in children discharged from 39 pediatric EDs from January 2018 - December 2019 using the Pediatric Health Information System. Our primary outcome was receipt of one of 12 low-value services across 9 conditions, including: chest radiography in asthma and bronchiolitis, beta agonist and corticosteroids in bronchiolitis, laboratory testing and neuroimaging in febrile seizure, neuroimaging in afebrile seizure, head injury and headache, and any imaging in sinusitis, constipation and facial trauma. We analyzed the association of race and ethnicity on receipt of low-value services using generalized linear mixed models.
Results: There were 4,676,802 patients in the final study cohort. For each condition, most patients were non-Hispanic White, with the exception of asthma (Table 1). Chest radiography for asthma and bronchiolitis, neuroimaging for head injury and headache, and imaging for constipation were more prevalent among non-Hispanic White patients (Table 2). Compared with non-Hispanic White (NHW) patients, non-Hispanic Black (NHB) and Hispanic patients had lower adjusted odds (aOR, 95% confidence interval) of receiving imaging for asthma (0.60, 0.56-0.63 NHB; 0.84, 0.79-0.89 Hispanic); bronchiolitis (0.84, 0.79-0.89 NHB; 0.93, 0.88-0.99 Hispanic); head injury (0.84, 0.80-0.88 NHB; 0.80, 0.76-0.84 Hispanic); headache (0.67, 0.63-0.72 NHB; 0.83, 0.78-0.88 Hispanic); and constipation (0.71, 0.67-0.74 NHB; 0.76, 0.72-0.80 Hispanic). NHB patients had lower odds of receiving imaging for afebrile seizures (0.89, 0.8-1.0) and facial trauma (0.69, 0.60-0.80); and Hispanic patients had lower odds of imaging (0.57, 0.36-0.90) and blood testing (0.82, 0.69-0.98) for febrile seizures. NHB patients had higher odds of receiving steroids (1.11, 1.00-1.21) and beta-agonists (1.38, 1.24-1.54) for bronchiolitis compared with NHW patients (Figure 2).Conclusion(s): NHW patients are more likely to receive low-value imaging while NHB patients are more likely to receive low-value medications for bronchiolitis. Our study demonstrates that racial and ethnic differences care extend to many services including those of low-value, highlighting the importance of greater understanding on the complexities of race and ethnicity on clinical practice.
Table 1. Patient Characteristics, by Condition
.jpg) a American Indian, Asian, Native Hawaiian, multiracial, other race/ethnicity
a American Indian, Asian, Native Hawaiian, multiracial, other race/ethnicity b Includes self-pay, charity, hospital did not bill, and other
Table 2. Prevalence of Low-Value Services, by Race/Ethnicity
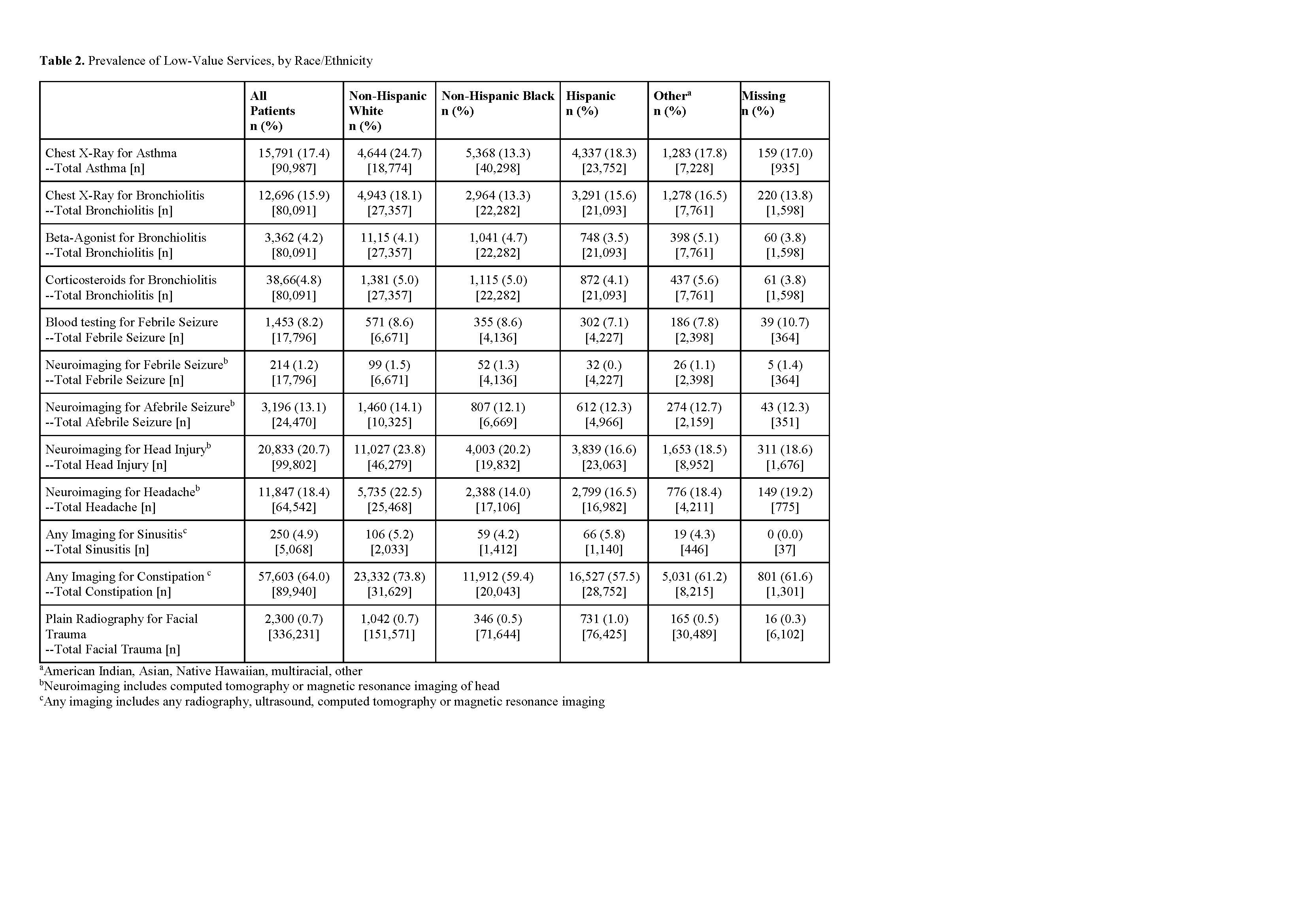 a American Indian, Asian, Native Hawaiian, multiracial, other
a American Indian, Asian, Native Hawaiian, multiracial, otherb Neuroimaging includes computed tomography or magnetic resonance imaging of head
c Any imaging includes any radiography, ultrasound, computed tomography or magnetic resonance imaging
