Medical Education: Resident
Category: Abstract Submission
Medical Education 9 - Medical Education: Resident II
251 - Resident education on food insecurity: partnering with the community to improve resident comfort, screening, and referrals
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 251
Publication Number: 251.333
Publication Number: 251.333
Samantha Williams Al-Kharusy, University of Wisconsin, Madison, WI, United States; Kelsi Rogers, University of Wisconsin, Madison, WI, United States; Laura Houser, UW Health, Madison, WI, United States; Mala Mathur, University of Wisconsin School of Medicine and Public Health, Verona, WI, United States
- SW
Samantha Williams Al-Kharusy, MD
Resident
University of Wisconsin
Madison, Wisconsin, United States
Presenting Author(s)
Background: As a result of the COVID-19 pandemic, Feeding America estimates that as many as 1 in 4 US children lives in a household with insufficient food to sustain an active, healthy life. Despite this significant need, few pediatricians receive training to reduce the burden of Food Insecurity (FI).
Objective: In this quality improvement initiative, we attempt to increase pediatric resident comfort addressing FI by developing a FI curriculum.
Design/Methods: We created an educational curriculum using evidence-based national and local resources in partnership with local community organizations. This curriculum consisted of one-hour educational sessions over a consecutive three-day period. Sessions focused on the burden of FI in our local community and how to address FI with patients and families, including how to place a referral for social work support within the electronic medical record. Instructional materials included a “FI Resident Quick-Guide” tri-fold pocket brochure that we developed alongside the FI curriculum. Additionally, residents had the opportunity to participate in the Supplemental Nutrition Assistance Program (SNAP) Challenge followed by a group reflection session. We measured outcomes by comparing pre-curriculum surveys to those completed 3 and 8 months’ post-curriculum.
Results: Pediatric residents completed surveys prior to the FI curriculum and again at 3 and 8 months’ post-curriculum (n=55). At 3 months’ post-curriculum, an increased proportion of residents reported they asked about FI in a majority of clinic visits (increase from 48% to 75% of residents, p = 0.026), were comfortable placing referrals (increase from 24% to 65% of residents, p = 0.037), and placed referrals in a majority of visits after identifying a FI need (increase from 36% to 65% of residents, p = 0.049). At 8 months’ post-curriculum, residents sustained increased comfort placing referrals (from 24% to 78% of residents, p = 0.013).Conclusion(s): Partnering with community organizations to provide a FI curriculum resulted in increased reported screening rates, comfort placing referrals, and referral rates among pediatric residents, with a sustained increase in comfort placing referrals at 8 months’ post-curriculum.
Food Insecurity Resident Quick-Guide, Outer tri-fold.jpg) Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources
Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources
Food Insecurity Resident Quick-Guide, Inner tri-fold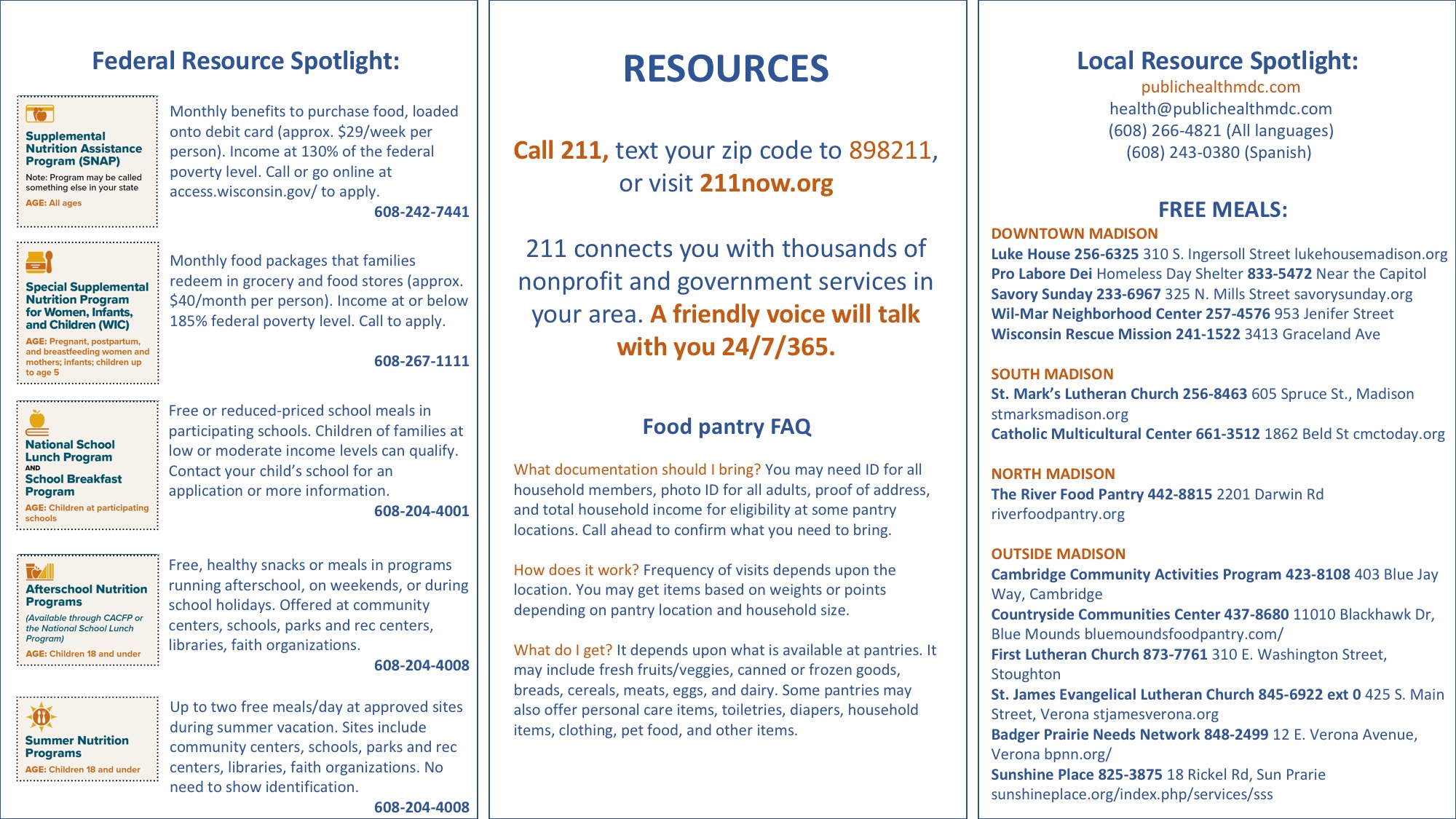 Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources
Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources
Objective: In this quality improvement initiative, we attempt to increase pediatric resident comfort addressing FI by developing a FI curriculum.
Design/Methods: We created an educational curriculum using evidence-based national and local resources in partnership with local community organizations. This curriculum consisted of one-hour educational sessions over a consecutive three-day period. Sessions focused on the burden of FI in our local community and how to address FI with patients and families, including how to place a referral for social work support within the electronic medical record. Instructional materials included a “FI Resident Quick-Guide” tri-fold pocket brochure that we developed alongside the FI curriculum. Additionally, residents had the opportunity to participate in the Supplemental Nutrition Assistance Program (SNAP) Challenge followed by a group reflection session. We measured outcomes by comparing pre-curriculum surveys to those completed 3 and 8 months’ post-curriculum.
Results: Pediatric residents completed surveys prior to the FI curriculum and again at 3 and 8 months’ post-curriculum (n=55). At 3 months’ post-curriculum, an increased proportion of residents reported they asked about FI in a majority of clinic visits (increase from 48% to 75% of residents, p = 0.026), were comfortable placing referrals (increase from 24% to 65% of residents, p = 0.037), and placed referrals in a majority of visits after identifying a FI need (increase from 36% to 65% of residents, p = 0.049). At 8 months’ post-curriculum, residents sustained increased comfort placing referrals (from 24% to 78% of residents, p = 0.013).Conclusion(s): Partnering with community organizations to provide a FI curriculum resulted in increased reported screening rates, comfort placing referrals, and referral rates among pediatric residents, with a sustained increase in comfort placing referrals at 8 months’ post-curriculum.
Food Insecurity Resident Quick-Guide, Outer tri-fold
.jpg) Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources
Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resourcesFood Insecurity Resident Quick-Guide, Inner tri-fold
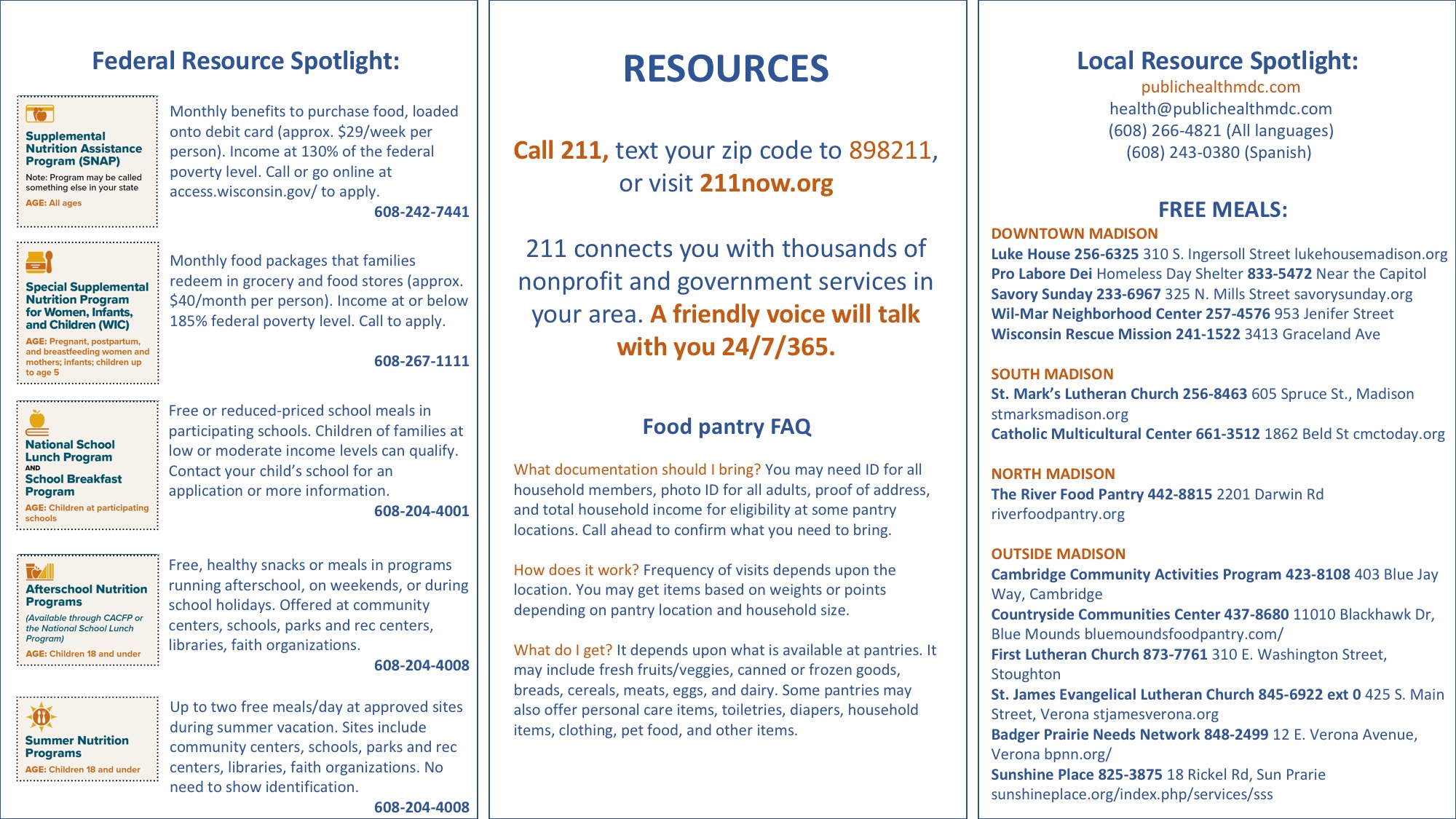 Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources
Tri-fold brochure created for residents outlining how to ask families about food insecurity, document this need in the medical record, and connect families with appropriate resources