Health Equity/Social Determinants of Health
Category: Abstract Submission
Health Equity/Social Determinants of Health IV
152 - Are there healthcare disparities in critically ill children admitted with severe traumatic brain injury (TBI): A Database Study
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 152
Publication Number: 152.411
Publication Number: 152.411
Jennifer R. Schwam, Weill Cornell Medicine, New York, NY, United States; Charlene Thomas, Weill Cornell Medicine, New York, NY, United States; Joy Howell, Weill Cornell Medicine, New York, NY, United States; Christine joyce, NewYork-Presbyterian Komansky Children’s Hospital, Brooklyn, NY, United States; Marianne E. Nellis, Weill Cornell Medicine, New York, NY, United States

Jennifer R. Schwam, MD
Resident
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Healthcare disparities have been observed in several sub-populations of critically ill children including those with critical bronchiolitis and oncologic diagnoses. Whereas outcomes of different medical and surgical management have been described, little work has been done to explore any healthcare disparities in children who suffer from severe traumatic brain injury (TBI).
Objective: We sought to determine any differences in mortality for children with severe TBI patients based on race and/or socioeconomic status.
Design/Methods: We performed a retrospective cohort study using the Pediatric Health Information System (PHIS) database, which includes 51 children’s hospitals affiliated with the Children’s Hospital Association. Pediatric encounters (0 to 18 years old) requiring PICU admission and invasive mechanical ventilation for TBI from 2008-2020 were included. Race and socioeconomic status (defined by type of insurance and median household income) were predictor variables. We performed a multivariate regression to account for confounders (including age, region, year, severity level, risk of mortality, presence of chronic conditions, discharge status, and cardiac arrest). Ethnicity was not accurate in our validation cohort and not included.
Results: 30,027 children were identified. Fifty-nine percent were male with a median (IQR) age of 3 (0-11). Fifty-four percent of children were White, 23% Black, 12% other, 7% 2 or more races, 2% Asian, 1% American Indian, and < 1% Pacific Islander. Sixty-one percent of children had governmental insurance and 31% commercial insurance. The median (IQR) household income was $47,815 (35,992-63,746). The overall mortality rate was 31% (9,414/30,027). As compared to white children, Asian race and 2 or more races were independently associated with increased mortality (Odds ratio – OR – 1.24, 95% CI 1.04-1.48, p=0.016 and OR 1.82, 95% CI 1.64-2.01, p < 0.001, respectively). No significant differences were seen with other races. As compared to commercial insurance, there was no significant difference in mortality in children with governmental insurance (OR 0.99, 95% CI 0.93-1.06, p=0.900). As compared to children in the lowest income bracket, children in each higher income bracket had significantly lower mortality rates (see Table below).Conclusion(s): In a large cohort of children with severe TBI, differences in mortality were observed based on both race and socioeconomic status. Further studies are needed to explore causality and if established, address reasons for disparities.
Table 1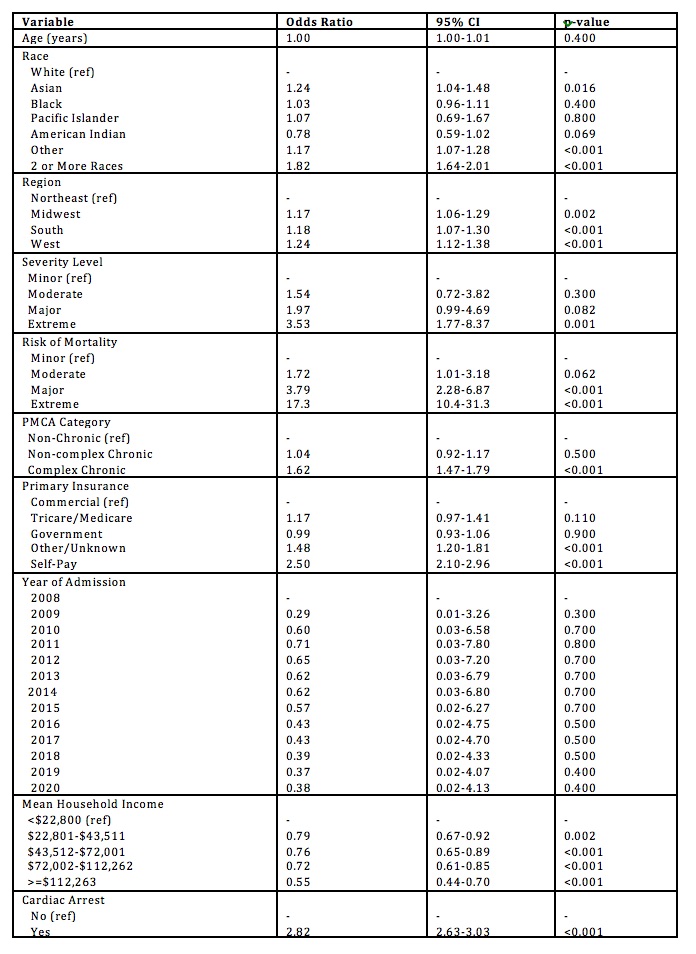 Multivariate Regression Examining Independent Associations with Mortality in Children with Severe TBI
Multivariate Regression Examining Independent Associations with Mortality in Children with Severe TBI
Objective: We sought to determine any differences in mortality for children with severe TBI patients based on race and/or socioeconomic status.
Design/Methods: We performed a retrospective cohort study using the Pediatric Health Information System (PHIS) database, which includes 51 children’s hospitals affiliated with the Children’s Hospital Association. Pediatric encounters (0 to 18 years old) requiring PICU admission and invasive mechanical ventilation for TBI from 2008-2020 were included. Race and socioeconomic status (defined by type of insurance and median household income) were predictor variables. We performed a multivariate regression to account for confounders (including age, region, year, severity level, risk of mortality, presence of chronic conditions, discharge status, and cardiac arrest). Ethnicity was not accurate in our validation cohort and not included.
Results: 30,027 children were identified. Fifty-nine percent were male with a median (IQR) age of 3 (0-11). Fifty-four percent of children were White, 23% Black, 12% other, 7% 2 or more races, 2% Asian, 1% American Indian, and < 1% Pacific Islander. Sixty-one percent of children had governmental insurance and 31% commercial insurance. The median (IQR) household income was $47,815 (35,992-63,746). The overall mortality rate was 31% (9,414/30,027). As compared to white children, Asian race and 2 or more races were independently associated with increased mortality (Odds ratio – OR – 1.24, 95% CI 1.04-1.48, p=0.016 and OR 1.82, 95% CI 1.64-2.01, p < 0.001, respectively). No significant differences were seen with other races. As compared to commercial insurance, there was no significant difference in mortality in children with governmental insurance (OR 0.99, 95% CI 0.93-1.06, p=0.900). As compared to children in the lowest income bracket, children in each higher income bracket had significantly lower mortality rates (see Table below).Conclusion(s): In a large cohort of children with severe TBI, differences in mortality were observed based on both race and socioeconomic status. Further studies are needed to explore causality and if established, address reasons for disparities.
Table 1
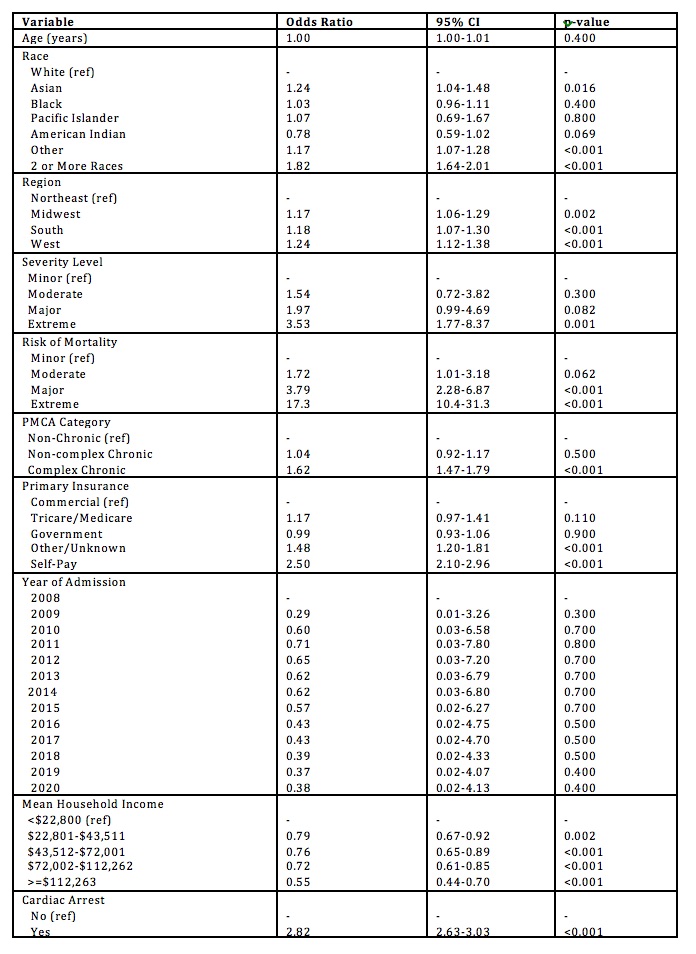 Multivariate Regression Examining Independent Associations with Mortality in Children with Severe TBI
Multivariate Regression Examining Independent Associations with Mortality in Children with Severe TBI