Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology V: Preclinical studies and Clinical Care Issues
475 - Changes in lung volume in a Crossover Trial of High-Flow Nasal Cannula compared to Nasal CPAP in Extremely Low Birth Weight Infants
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 475
Publication Number: 475.433
Publication Number: 475.433
Anup Katheria, Sharp Mary Birch Hospital for Women & Newborns, SAN DIEGO, CA, United States; Felix Ines, Sharp HealthCare, San Diego, CA, United States; Judith Hough, Australian Catholic University, Brisbane, Queensland, Australia; Shashank Sanjay, Sharp Healthcare, San Diego, CA, United States; Wade D. Rich, Sharp Mary Birch Hospital for Women and Newborns, San Diego, CA, United States; Ana L. Morales, Sharp Healthcare Neonatal Research Institute, San Diego, CA, United States; paul R. wozniak, Sharp Mary Birch Hospital, san diego, CA, United States; Neil N. Finer, University of California, San Diego School of Medicine, La Jolla, CA, United States

Anup Katheria, MD
Physician
Sharp Mary Birch Hospital for Women & Newborns
San Diego, California, United States
Presenting Author(s)
Background: There are inadequate data on the effects of high flow nasal cannula (HFNC) in infants < 29 weeks gestational age.
Objective: To measure changes in pulmonary parameters in preterm infants on HFNC compared to nasal continuous positive airway pressure (nCPAP) using electrical impedance tomography (EIT).
Design/Methods: A crossover study in preterm infants < 29 weeks gestation at birth requiring CPAP therapy was conducted. Once stable on CPAP (at least 72 hours post extubation or >72 hours of life) infants had serial measurements using the EIT belt while being transitioned from CPAP to HFNC and back to CPAP. The EIT belt was placed around the chest while infants were in the supine position. The primary endpoint to be used for efficacy evaluation was the percentage of atelectasis (measured as unventilated lung) as measured by EIT. Subjects had a baseline read while on CPAP (5-7 cm of H2O) then transitioned to HFNC (8 LPM) and a reading at 30 minutes, another reading at 6 hours, and a reading once transitioned back on CPAP for 1 hour. Normally distributed continuous outcome variables were analyzed within dependent samples T-Test and non-normal continuous outcome variables were analyzed with the Mann–Whitney U test. A one way repeated measured analysis of variance (ANOVA) was conducted to evaluate the null hypothesis that there was no change in each measure from baseline. Significance was set at a p value less than 0.05. Demographic data are presented as numbers and proportions.
Results: 80 newborns were enrolled (Table 1, demographics). 78 infants had data for interpretation (2 infants had missing data). There was no difference in the percentage of unventilated lung (as measured by dependent silent spaces (DSS) using electrical impedance tomography (Figure 1, ANOVA, p=0.64). In addition, secondary outcomes of geometric center of ventilation (CoV), end-expiratory lung volumes, and stretch (percentage of maximal impedance change) were not different between groups (ANOVA, p= 0.366, 0.221, 0.752 respectively). 20 infants could not tolerate 6 hours of HFNC due to increasing oxygen requirement but had measurements at 30 minutes of HFNC and back on CPAP. Failed HFNC infants were smaller and required higher CPAP and FiO2 (Table 2).Conclusion(s): Infants transitioned from CPAP to HFNC for a period of 6 hours did not demonstrate any differences in lung aeration using EIT, despite one-fourth of infants requiring rescue CPAP due to increased oxygen requirements. Providing eight liters per minute of flow via a nasal cannula appears to be effective/comparable to nasal CPAP in the majority of very preterm infants.
Table 1 Baseline Characteristics.jpg)
Figure 1 Box and Whisker plot over each period.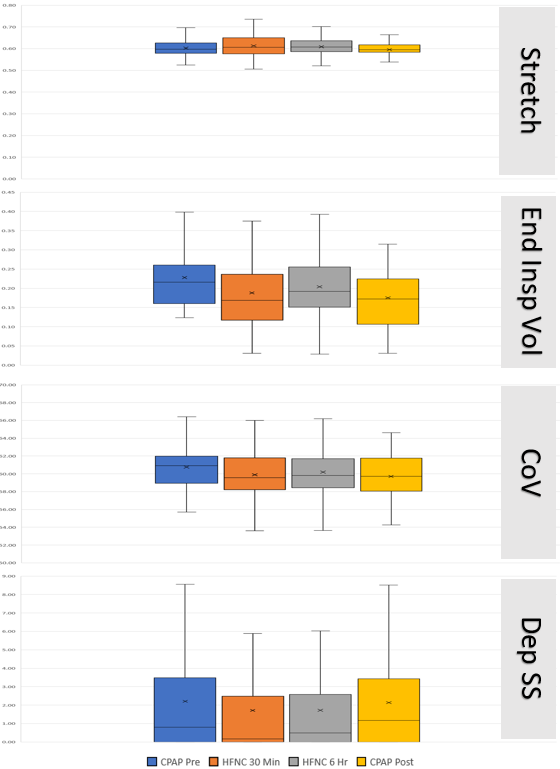 Figure 1 Box and Whisker plot over each period (Stretch, CoV, Center of Ventilation; Dep SS, dependent silent spaces as a percentage of lung;, Volume, end insp vol, end-inspiratory lung volume). CPAP Pre- CPAP at the start of the study, HFNC 30min- 30 minutes of High-flow Cannula, HFNC 6hrs- 6 hours of High-flow cannula, CPAP post- 1 hour after return to CPAP. X denotes mean value otherwise median and 25th and 75th percentiles are shown.
Figure 1 Box and Whisker plot over each period (Stretch, CoV, Center of Ventilation; Dep SS, dependent silent spaces as a percentage of lung;, Volume, end insp vol, end-inspiratory lung volume). CPAP Pre- CPAP at the start of the study, HFNC 30min- 30 minutes of High-flow Cannula, HFNC 6hrs- 6 hours of High-flow cannula, CPAP post- 1 hour after return to CPAP. X denotes mean value otherwise median and 25th and 75th percentiles are shown.
Objective: To measure changes in pulmonary parameters in preterm infants on HFNC compared to nasal continuous positive airway pressure (nCPAP) using electrical impedance tomography (EIT).
Design/Methods: A crossover study in preterm infants < 29 weeks gestation at birth requiring CPAP therapy was conducted. Once stable on CPAP (at least 72 hours post extubation or >72 hours of life) infants had serial measurements using the EIT belt while being transitioned from CPAP to HFNC and back to CPAP. The EIT belt was placed around the chest while infants were in the supine position. The primary endpoint to be used for efficacy evaluation was the percentage of atelectasis (measured as unventilated lung) as measured by EIT. Subjects had a baseline read while on CPAP (5-7 cm of H2O) then transitioned to HFNC (8 LPM) and a reading at 30 minutes, another reading at 6 hours, and a reading once transitioned back on CPAP for 1 hour. Normally distributed continuous outcome variables were analyzed within dependent samples T-Test and non-normal continuous outcome variables were analyzed with the Mann–Whitney U test. A one way repeated measured analysis of variance (ANOVA) was conducted to evaluate the null hypothesis that there was no change in each measure from baseline. Significance was set at a p value less than 0.05. Demographic data are presented as numbers and proportions.
Results: 80 newborns were enrolled (Table 1, demographics). 78 infants had data for interpretation (2 infants had missing data). There was no difference in the percentage of unventilated lung (as measured by dependent silent spaces (DSS) using electrical impedance tomography (Figure 1, ANOVA, p=0.64). In addition, secondary outcomes of geometric center of ventilation (CoV), end-expiratory lung volumes, and stretch (percentage of maximal impedance change) were not different between groups (ANOVA, p= 0.366, 0.221, 0.752 respectively). 20 infants could not tolerate 6 hours of HFNC due to increasing oxygen requirement but had measurements at 30 minutes of HFNC and back on CPAP. Failed HFNC infants were smaller and required higher CPAP and FiO2 (Table 2).Conclusion(s): Infants transitioned from CPAP to HFNC for a period of 6 hours did not demonstrate any differences in lung aeration using EIT, despite one-fourth of infants requiring rescue CPAP due to increased oxygen requirements. Providing eight liters per minute of flow via a nasal cannula appears to be effective/comparable to nasal CPAP in the majority of very preterm infants.
Table 1 Baseline Characteristics
.jpg)
Figure 1 Box and Whisker plot over each period.
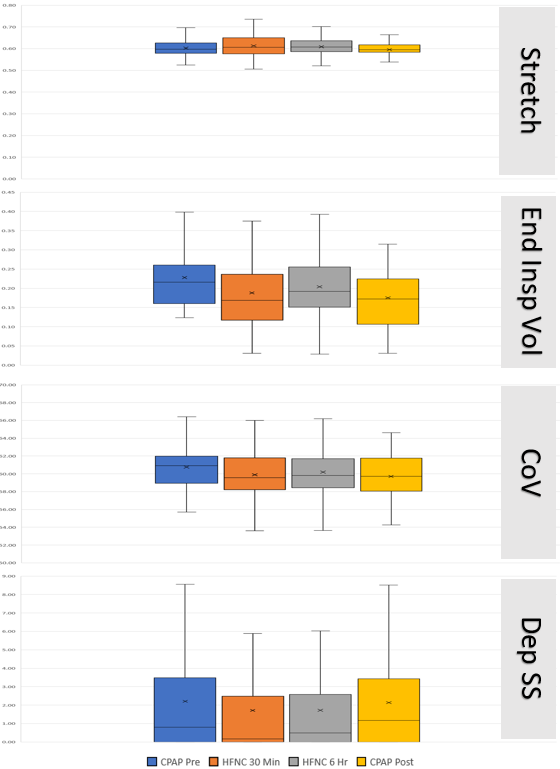 Figure 1 Box and Whisker plot over each period (Stretch, CoV, Center of Ventilation; Dep SS, dependent silent spaces as a percentage of lung;, Volume, end insp vol, end-inspiratory lung volume). CPAP Pre- CPAP at the start of the study, HFNC 30min- 30 minutes of High-flow Cannula, HFNC 6hrs- 6 hours of High-flow cannula, CPAP post- 1 hour after return to CPAP. X denotes mean value otherwise median and 25th and 75th percentiles are shown.
Figure 1 Box and Whisker plot over each period (Stretch, CoV, Center of Ventilation; Dep SS, dependent silent spaces as a percentage of lung;, Volume, end insp vol, end-inspiratory lung volume). CPAP Pre- CPAP at the start of the study, HFNC 30min- 30 minutes of High-flow Cannula, HFNC 6hrs- 6 hours of High-flow cannula, CPAP post- 1 hour after return to CPAP. X denotes mean value otherwise median and 25th and 75th percentiles are shown.