Child Abuse & Neglect
Category: Abstract Submission
Child Abuse & Neglect I
215 - Child Protective Services for Preterm Infants in the NICU: Rates and Risk Factors
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 215
Publication Number: 215.401
Publication Number: 215.401
Alison Little, Brown University/Women & Infants Hospital, Providence, RI, United States; Betty R. Vohr, Women & Infants Hospital of Rhode Island; Alpert Medical School of Brown University, Providence, SD, United States; Richard Tucker, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Elisabeth McGowan, Women & Infants Hospital of Rhode Island, Providence, RI, United States

Alison Little, MD, MPH
Fellow in Neonatal-Perinatal Medicine
Brown University/Women & Infants Hospital
Providence, Rhode Island, United States
Presenting Author(s)
Background: Preterm (PT) infants are at increased risk for maltreatment and child protective services involvement (CPSI) compared to term infants. However, little is known about their CPSI while in the neonatal intensive care unit (NICU).
Objective: (1) To describe the incidence of CPSI among PT infants in the NICU and (2) to identify infant medical characteristics and maternal psychosocial characteristics associated with CPSI in the NICU and/or at discharge.
Design/Methods: The cohort includes infants < 30 weeks gestation born at Women & Infants Hospital from 2012 to 2018. Maternal socioeconomic and psychosocial data (e.g., mental health history, substance abuse, domestic abuse) and infant medical data were analyzed. Infants were categorized as No CPSI, prior CPSI only (i.e., family history of CPSI) or NICU CPSI. NICU CPSI was further subcategorized as CPSI NICU only or ongoing CPSI at NICU discharge. The primary outcome was NICU CPSI. Descriptive statistics were performed to characterize CPSI subcategories. Bivariate analyses and multivariate logistic regression were used to identify factors independently associated with NICU CPSI.
Results: Of 741 infants, 124 (17%) had NICU CPSI: 35 (28%) had CPSI NICU only, and 89 (72%) had CPSI at discharge (Table 1). Of those with CPSI at discharge, 40 (45%) were discharged to CPS custody. 65% of NICU CPSI cases involved maternal substance abuse; of these, 73% involved cannabis and 36% involved opiates. Bivariate analyses showed no major differences in infant medical characteristics between groups, though infants with NICU CPSI were less likely to receive breast milk at discharge compared to the No CPSI group (8% vs. 51%, p< 0.0001). Mothers of infants with NICU CPSI were significantly younger, less educated and more likely to be single. Rates of maternal mental health disorders (77% vs 45%), substance abuse (76% vs 8%) and domestic abuse (45% vs 7%) were significantly higher in infants with NICU CPSI (p < 0.0001; Table 2). In the multivariate analyses, mothers with substance abuse had 25 times the odds of CPSI (OR 25.3; 11.9-53.6, Table 3). Other predictors of NICU CPSI were public insurance (OR 13.0; 2.4-69.7), domestic abuse (OR 4.11; 1.9-9.1) and maternal education less than high school (OR 2.19; 1.0-4.8).Conclusion(s): One in 6 PT infants had NICU CPSI; of these, 3 in 4 had ongoing CPSI at discharge. PT infants with NICU CPSI have significantly higher rates of co-existing socioeconomic and psychosocial factors, indicating a need for proactive intervention and support in the NICU.
Table 1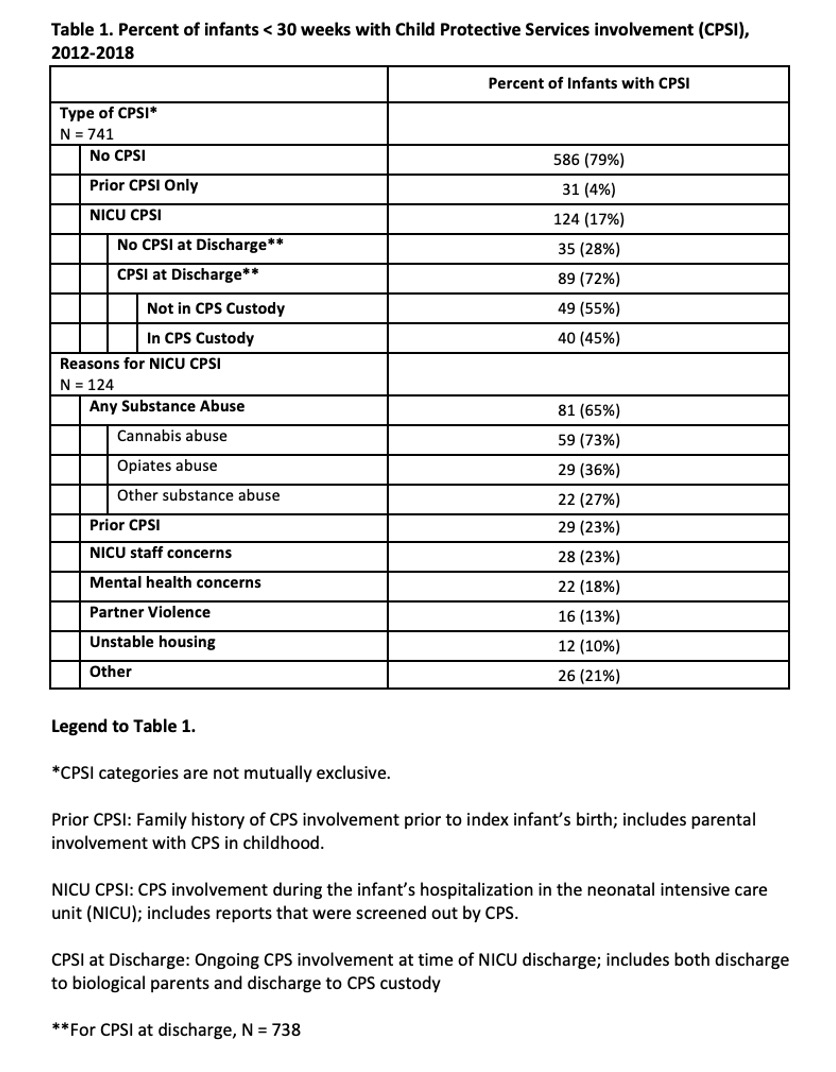 Percent of infants < 30 weeks with Child Protective Services involvement (CPSI), 2012-2018
Percent of infants < 30 weeks with Child Protective Services involvement (CPSI), 2012-2018
Table 2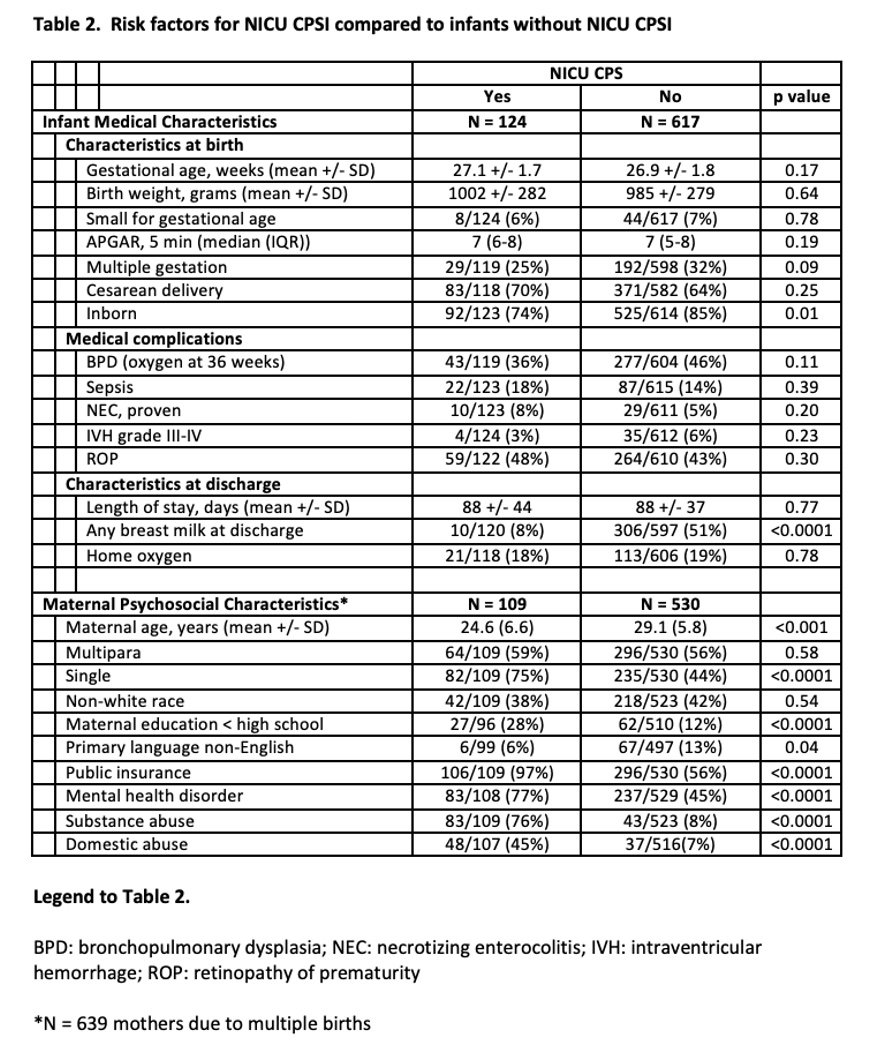 Risk factors for NICU CPSI compared to infants without NICU CPSI
Risk factors for NICU CPSI compared to infants without NICU CPSI
Objective: (1) To describe the incidence of CPSI among PT infants in the NICU and (2) to identify infant medical characteristics and maternal psychosocial characteristics associated with CPSI in the NICU and/or at discharge.
Design/Methods: The cohort includes infants < 30 weeks gestation born at Women & Infants Hospital from 2012 to 2018. Maternal socioeconomic and psychosocial data (e.g., mental health history, substance abuse, domestic abuse) and infant medical data were analyzed. Infants were categorized as No CPSI, prior CPSI only (i.e., family history of CPSI) or NICU CPSI. NICU CPSI was further subcategorized as CPSI NICU only or ongoing CPSI at NICU discharge. The primary outcome was NICU CPSI. Descriptive statistics were performed to characterize CPSI subcategories. Bivariate analyses and multivariate logistic regression were used to identify factors independently associated with NICU CPSI.
Results: Of 741 infants, 124 (17%) had NICU CPSI: 35 (28%) had CPSI NICU only, and 89 (72%) had CPSI at discharge (Table 1). Of those with CPSI at discharge, 40 (45%) were discharged to CPS custody. 65% of NICU CPSI cases involved maternal substance abuse; of these, 73% involved cannabis and 36% involved opiates. Bivariate analyses showed no major differences in infant medical characteristics between groups, though infants with NICU CPSI were less likely to receive breast milk at discharge compared to the No CPSI group (8% vs. 51%, p< 0.0001). Mothers of infants with NICU CPSI were significantly younger, less educated and more likely to be single. Rates of maternal mental health disorders (77% vs 45%), substance abuse (76% vs 8%) and domestic abuse (45% vs 7%) were significantly higher in infants with NICU CPSI (p < 0.0001; Table 2). In the multivariate analyses, mothers with substance abuse had 25 times the odds of CPSI (OR 25.3; 11.9-53.6, Table 3). Other predictors of NICU CPSI were public insurance (OR 13.0; 2.4-69.7), domestic abuse (OR 4.11; 1.9-9.1) and maternal education less than high school (OR 2.19; 1.0-4.8).Conclusion(s): One in 6 PT infants had NICU CPSI; of these, 3 in 4 had ongoing CPSI at discharge. PT infants with NICU CPSI have significantly higher rates of co-existing socioeconomic and psychosocial factors, indicating a need for proactive intervention and support in the NICU.
Table 1
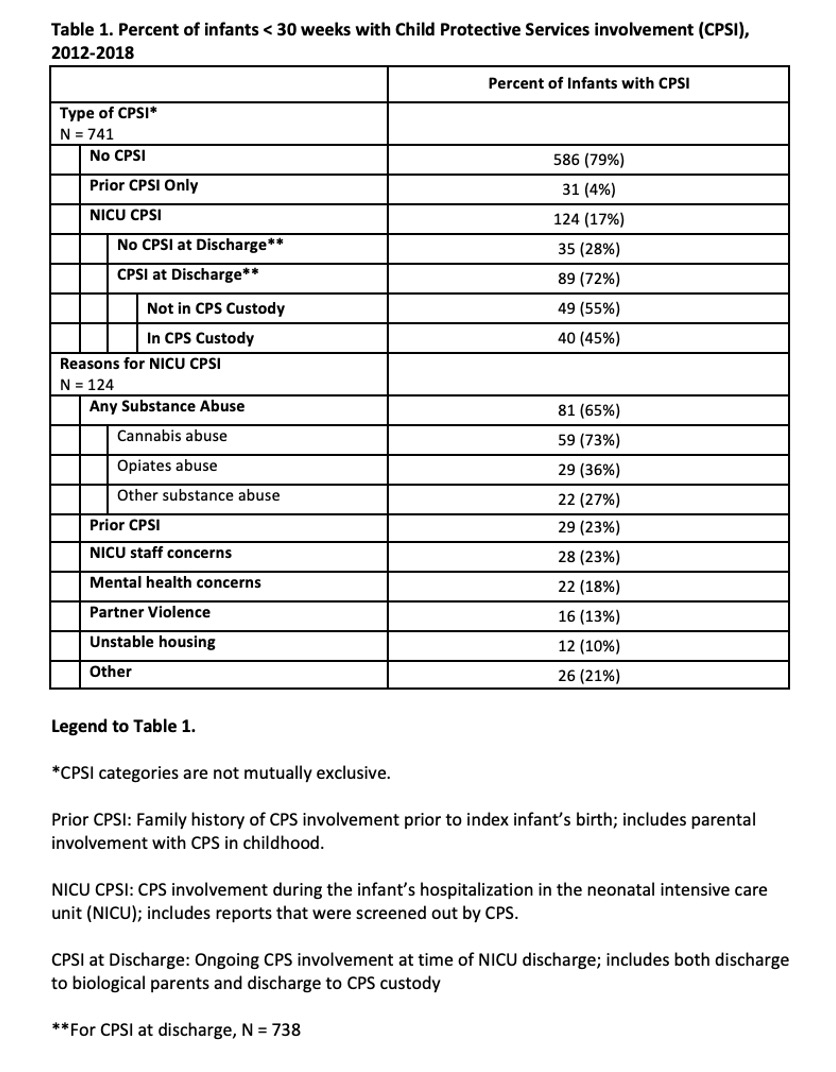 Percent of infants < 30 weeks with Child Protective Services involvement (CPSI), 2012-2018
Percent of infants < 30 weeks with Child Protective Services involvement (CPSI), 2012-2018Table 2
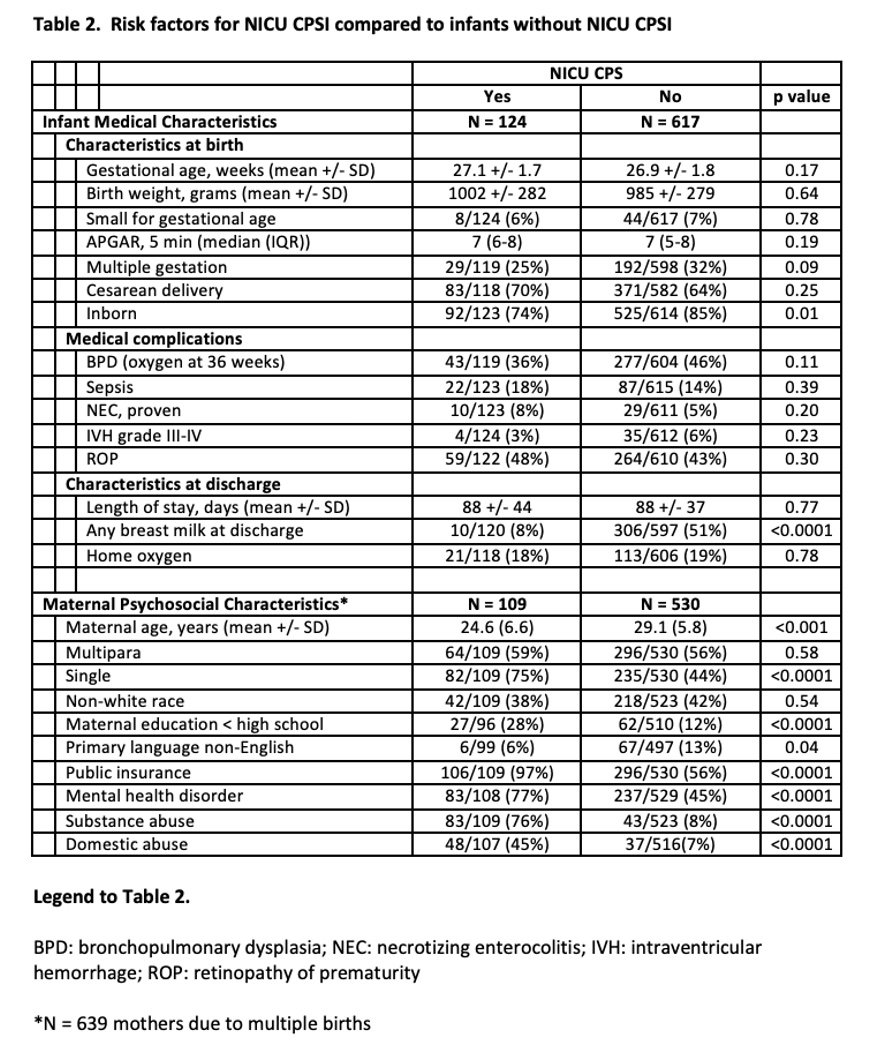 Risk factors for NICU CPSI compared to infants without NICU CPSI
Risk factors for NICU CPSI compared to infants without NICU CPSI