Back
Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement IV: Respiratory and Temperature Regulation
374 - Continuous positive airway pressure weaning guidelines in preterm infants: a quality improvement project
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 374
Publication Number: 374.434
Publication Number: 374.434
Shivani Mattikalli, Pennsylvania State University College of Medicine, Potomac, MD, United States; Shaili Amatya, Penn State College of Medicine, Hershey, PA, United States; Kelly Weller, Penn State Children's Hospital, Millerstown, PA, United States; Heather Stephens, Penn State Health Children's Hospital, Hershey, PA, United States; Jennifer L. Erkinger, Penn State Children's Hospital, Denver, PA, United States; Kimberly Wisecup, Penn State Children's Hospital, Hershey, PA, United States

Shivani Mattikalli, BS
MS1
Pennsylvania State University College of Medicine
Potomac, Maryland, United States
Presenting Author(s)
Background:
Continuous positive airway pressure (CPAP) has many benefits in managing preterm infants with respiratory distress. It is associated with less surfactant use, decreased extubation failure, and increased alveolar recruitment. Introduction of CPAP bundles has been shown to decrease bronchopulmonary dysplasia (BPD). Successful weaning from CPAP facilitates oral feeding and developmentally appropriate activities. There have been two randomized controlled trials and one systemic review investigating weaning methods; however, no consensus has been reached about the optimal timing.
Objective: This study aims to increase compliance to new weaning guidelines to 100% and increase successful weaning to room air to 95% in a level-IV neonatal intensive care unit (NICU) over a 2 years.
Design/Methods:
Bubble CPAP was initiated in our NICU in 2020. Guidelines were created, including weaning criteria, and education was provided. This ongoing quality improvement (QI) has included 3 plan-do-study-act cycles to date. Primary outcomes include compliance with guidelines and successful transition to room air on the first attempt. Secondary outcomes include BPD. Process measures included the creation of bedside cards, the introduction of multidisciplinary rounds, and use of reminders. Balancing measures included total days on respiratory support and length of hospital stay. Trends were observed using a run chart, and process changes were studied using control p charts. This project was reviewed by the institutional review board and deemed exempt.
Results:
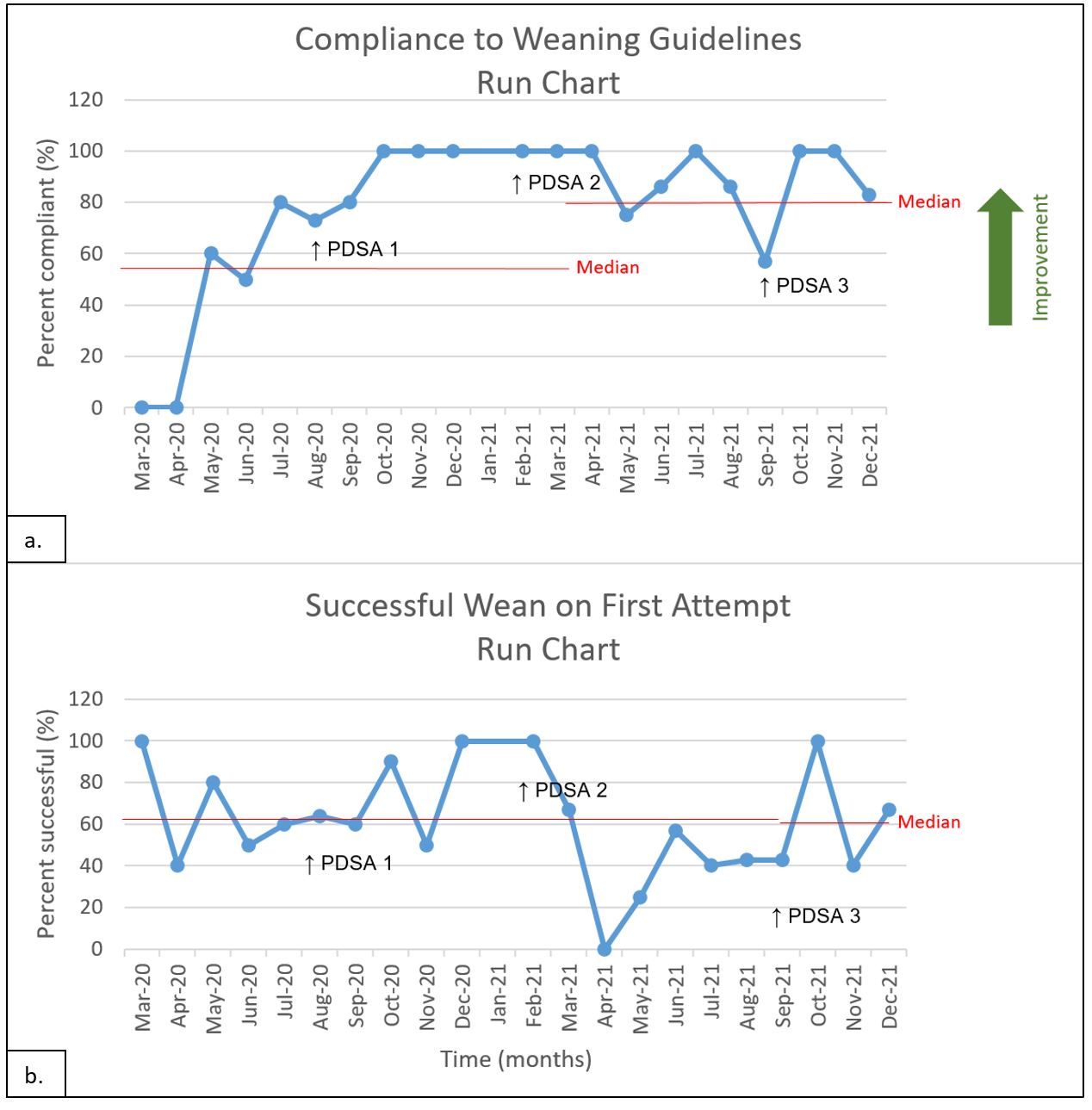
Between March 2020 and December 2021, 109 neonates with an average gestational age of 29 3/7 weeks’ and birth weight of 1.22 kilograms were studied (Table 1.). Concept changes included managing variation (standardization), changing the work environment (developing alliances and providing access to information), and designing a system to avoid mistakes (use of reminders). Practice changes resulted in an increase in compliance (Figure 1a.) and overall improvement. In addition, there were no noted special-cause variations (Figure 2.).
Conclusion(s):
Implementation of process measures led to greater compliance to weaning guidelines. Trends showed that as compliance improved, so did successful weaning to room air. Areas where this did not track occurred in the extremely low gestational age and birth weight infants. It is important to determine which weaning criteria lead to success, as well as increasing the compliance to criteria as opposed to an ad hoc method of weaning.
Table 1. Patient Demographics.jpg) Mean (SD) unless stated otherwise, *n(%). Abbreviations: INSURE- intubation, surfactant, rapid extubation.
Mean (SD) unless stated otherwise, *n(%). Abbreviations: INSURE- intubation, surfactant, rapid extubation.
Figure 1. Run Chart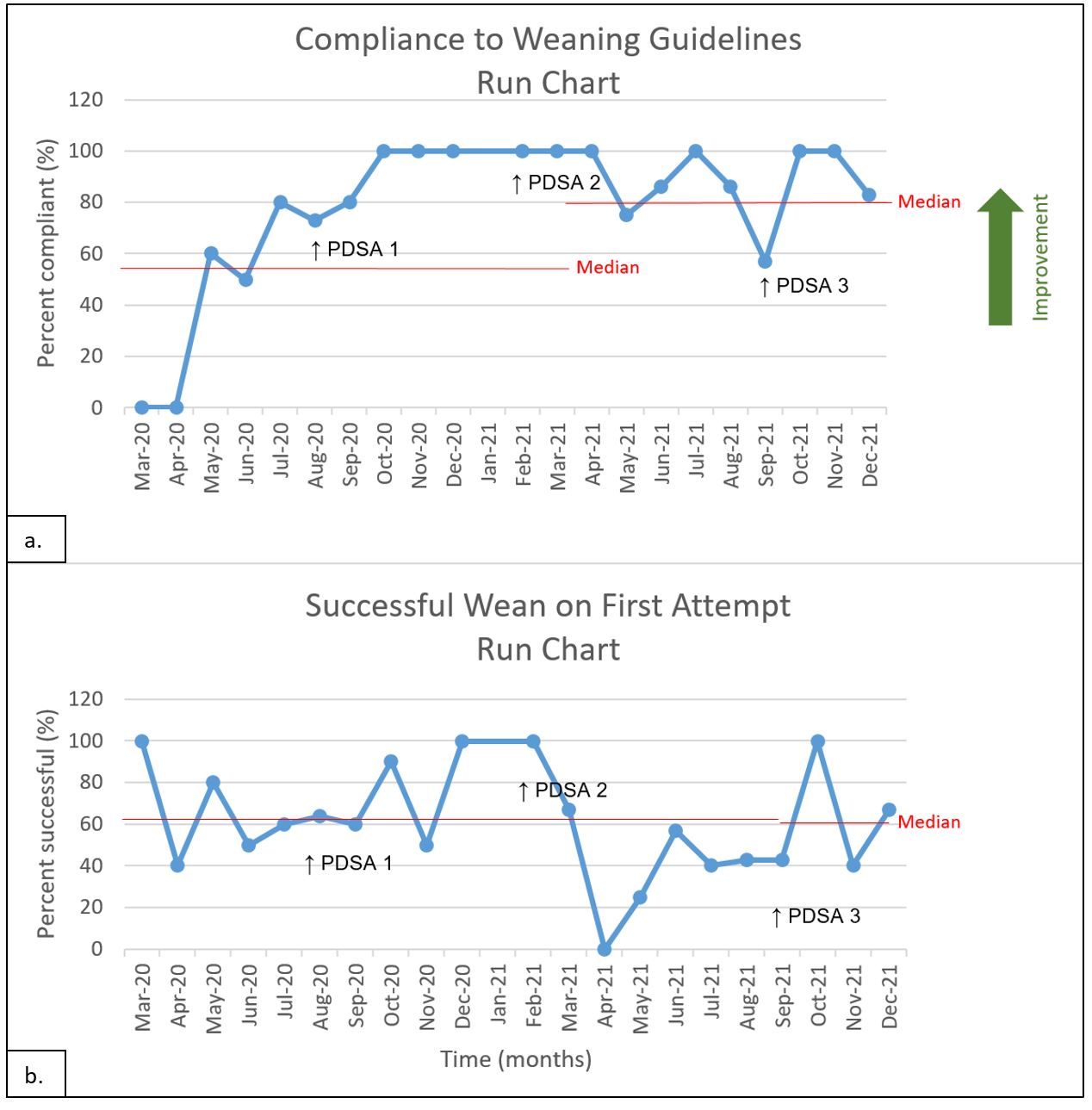
Continuous positive airway pressure (CPAP) has many benefits in managing preterm infants with respiratory distress. It is associated with less surfactant use, decreased extubation failure, and increased alveolar recruitment. Introduction of CPAP bundles has been shown to decrease bronchopulmonary dysplasia (BPD). Successful weaning from CPAP facilitates oral feeding and developmentally appropriate activities. There have been two randomized controlled trials and one systemic review investigating weaning methods; however, no consensus has been reached about the optimal timing.
Objective: This study aims to increase compliance to new weaning guidelines to 100% and increase successful weaning to room air to 95% in a level-IV neonatal intensive care unit (NICU) over a 2 years.
Design/Methods:
Bubble CPAP was initiated in our NICU in 2020. Guidelines were created, including weaning criteria, and education was provided. This ongoing quality improvement (QI) has included 3 plan-do-study-act cycles to date. Primary outcomes include compliance with guidelines and successful transition to room air on the first attempt. Secondary outcomes include BPD. Process measures included the creation of bedside cards, the introduction of multidisciplinary rounds, and use of reminders. Balancing measures included total days on respiratory support and length of hospital stay. Trends were observed using a run chart, and process changes were studied using control p charts. This project was reviewed by the institutional review board and deemed exempt.
Results:
Between March 2020 and December 2021, 109 neonates with an average gestational age of 29 3/7 weeks’ and birth weight of 1.22 kilograms were studied (Table 1.). Concept changes included managing variation (standardization), changing the work environment (developing alliances and providing access to information), and designing a system to avoid mistakes (use of reminders). Practice changes resulted in an increase in compliance (Figure 1a.) and overall improvement. In addition, there were no noted special-cause variations (Figure 2.).
Conclusion(s):
Implementation of process measures led to greater compliance to weaning guidelines. Trends showed that as compliance improved, so did successful weaning to room air. Areas where this did not track occurred in the extremely low gestational age and birth weight infants. It is important to determine which weaning criteria lead to success, as well as increasing the compliance to criteria as opposed to an ad hoc method of weaning.
Table 1. Patient Demographics
.jpg) Mean (SD) unless stated otherwise, *n(%). Abbreviations: INSURE- intubation, surfactant, rapid extubation.
Mean (SD) unless stated otherwise, *n(%). Abbreviations: INSURE- intubation, surfactant, rapid extubation.Figure 1. Run Chart