Neonatal Respiratory Assessment/Support/Ventilation
Category: Abstract Submission
Neonatal Respiratory III: BPD
460 - Do Extremely Low Birth Weight (ELBW) Infants Tolerate Extubation to Neurally Adjusted Ventilatory Assist (NAVA) Better Than Conventional Non-Invasive Positive Pressure Ventilation (NIPPV)?
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 460
Publication Number: 460.229
Publication Number: 460.229
Kevin Louie, Westchester Medical Center, Tarrytown, NY, United States; Shaili Amatya, Penn State College of Medicine, Hershey, PA, United States; Lance Parton, MFCH at WMC, NYMC, BCHP, Valhalla, NY, United States
- KL
Kevin Louie, DO
Fellow
Westchester Medical Center
Westchester Medical Center
Tarrytown, New York, United States
Presenting Author(s)
Background: Infants weighing less than 1 kg at birth (ELBW) are at high risk for the development of bronchopulmonary dysplasia (BPD) and ventilator-induced lung injury (VILI), in part because of the need for mechanical ventilation utilizing an endotracheal tube (MVET). Various noninvasive (NIV) strategies have been utilized following elective extubation to prevent the need for reintubation. Continuous positive airway pressure (CPAP) and NIPPV are modalities frequently used. Studies have shown decreased elective extubation failure when placed on NIPPV compared to CPAP. Furthermore, synchronized noninvasive positive pressure ventilation (sNIPPV) utilizing NAVA compared to NIPPV has demonstrated improvements in pulmonary mechanics, work of breathing, and extubation success in preterm infants. To our knowledge, there are no randomized controlled trials comparing sNIPPV using NAVA with NIPPV in ELBW infants during elective extubation.
Objective: This study investigates the effectiveness of extubation from conventional mechanical ventilation (MVET) to sNIPPV using NAVA or NIPPV in ELBW infants.
Design/Methods: Consented ELBW infants are randomized to sNIPPV using NAVA or NIPPV in a one to one computer-generated scheme. Patient demographics are collected and infants are assessed for duration infant remain extubated. The Institutional Review Board (IRB) of New York Medical College approved this study.
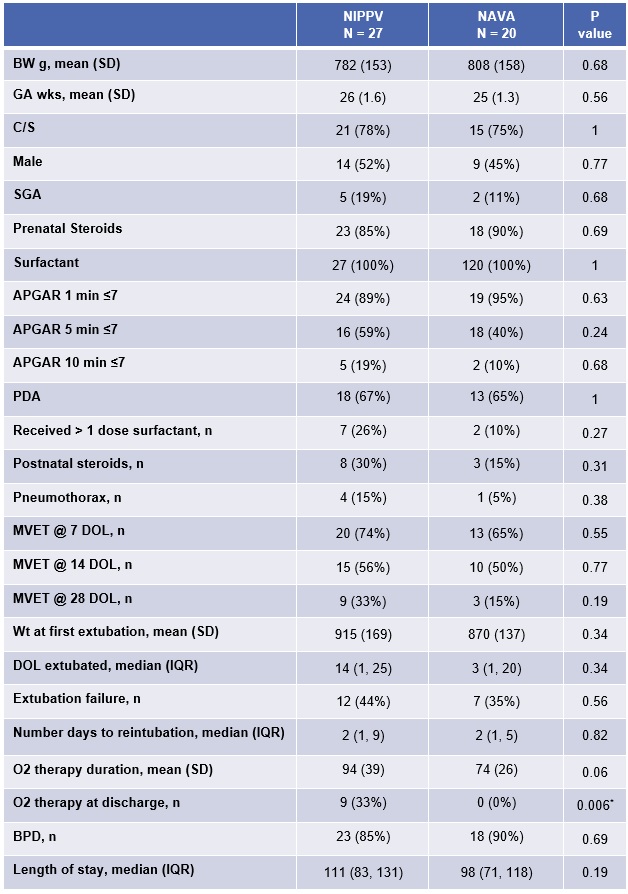
Results: At the time of analysis our data included 47 ELBW infants of which 27 were randomized to NIPPV and 20 to NAVA. The average birth weight was 782 (153) grams [mean (SD)] and 808 (158) grams in the NIPPV and sNIPPV groups, respectively. There were no statistically significant differences between the two group demographics. Median time to reintubation was 2 (1, 9) [median (IQR)] days in the NIPPV group and 2 (1, 5) days in the NAVA group, which was not statistically significant. Overall there was a 40% extubation failure across the groups. There were no infants in the sNIPPV group requiring oxygen at time of discharge compared to 9 in the NIPPV group (p = 0.006).Conclusion(s): This interim analysis has shown similar extubation failure among ELBW infants in comparison to prior studies. While there were no statistically significant differences in extubation success, time to reintubation, BPD, or length of stay there were no infants in the NAVA group discharged home on oxygen, which may improve outcome variables not measured in this study. The use of NAVA may be a possible alternative mode of NIV in the ELBW population.
Infant Characteristics and Results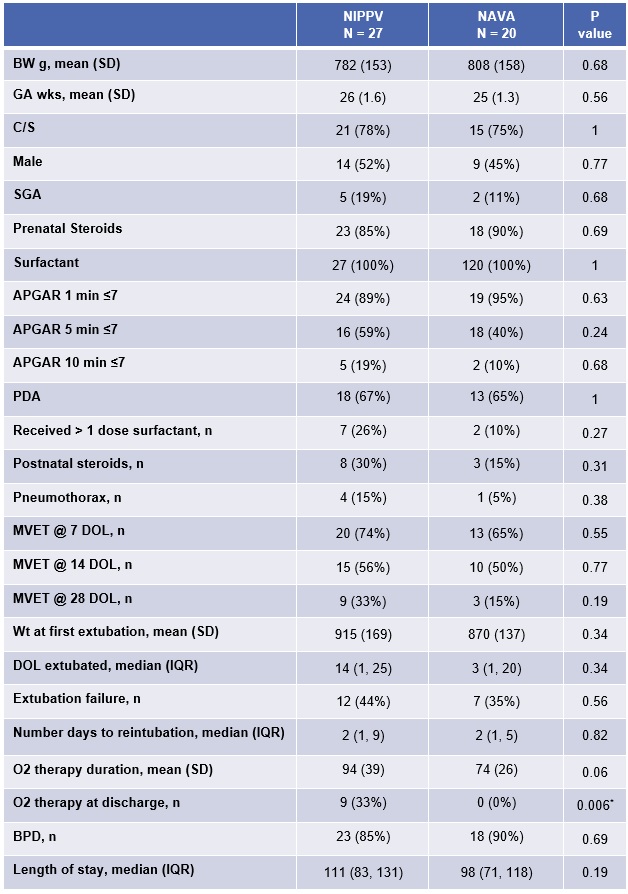
Objective: This study investigates the effectiveness of extubation from conventional mechanical ventilation (MVET) to sNIPPV using NAVA or NIPPV in ELBW infants.
Design/Methods: Consented ELBW infants are randomized to sNIPPV using NAVA or NIPPV in a one to one computer-generated scheme. Patient demographics are collected and infants are assessed for duration infant remain extubated. The Institutional Review Board (IRB) of New York Medical College approved this study.
Results: At the time of analysis our data included 47 ELBW infants of which 27 were randomized to NIPPV and 20 to NAVA. The average birth weight was 782 (153) grams [mean (SD)] and 808 (158) grams in the NIPPV and sNIPPV groups, respectively. There were no statistically significant differences between the two group demographics. Median time to reintubation was 2 (1, 9) [median (IQR)] days in the NIPPV group and 2 (1, 5) days in the NAVA group, which was not statistically significant. Overall there was a 40% extubation failure across the groups. There were no infants in the sNIPPV group requiring oxygen at time of discharge compared to 9 in the NIPPV group (p = 0.006).Conclusion(s): This interim analysis has shown similar extubation failure among ELBW infants in comparison to prior studies. While there were no statistically significant differences in extubation success, time to reintubation, BPD, or length of stay there were no infants in the NAVA group discharged home on oxygen, which may improve outcome variables not measured in this study. The use of NAVA may be a possible alternative mode of NIV in the ELBW population.
Infant Characteristics and Results