Back
Emergency Medicine: Quality Improvement
Category: Abstract Submission
Emergency Medicine XIII
36 - Improving Communication with Limited English Proficiency Families in a Pediatric Emergency Department
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 36
Publication Number: 36.406
Publication Number: 36.406
Gauthami Soma, Yale School of Medicine, West Hartford, CT, United States; Emily Powers, Yale School of Medicine, Hamden, CT, United States; Melissa L. Langhan, Yale University School of Medicine, New Haven, CT, United States; Ammarah U. Iqbal, Yale-New Haven Children's Hospital, New Haven, CT, United States; Rabia N. Malik, Yale School of Medicine, New Haven, CT, United States; Isabel Gross, Yale School of Medicine, New Haven, CT, United States; Yesenia Reynoso Severino, Yale New Haven Health, New Haven, CT, United States; Crystal Clemons, Yale New Haven Hospital, Wallingford, CT, United States; Sonali Bhalodkar, Yale-New Haven Children's Hospital, New Haven, CT, United States; Taryn Webb, Yale-New Haven Children's Hospital, Westport, CT, United States; Prisca Takundwa, Yale New Haven Hospital, Hamden, CT, United States; Alexandria Georgadarellis, Yale-New Haven Children's Hospital, New Havn, CT, United States; Nicole Irgens-Moller, Yale-New Haven Children's Hospital, New Haven, CT, United States; Gunjan Tiyyagura, yale university school of medicine, New Haven, CT, United States
- GS
Gauthami Soma, MD
Fellow in Pediatric Emergency Medicine
Yale School of Medicine
West Hartford, Connecticut, United States
Presenting Author(s)
Background: Language barriers contribute to poor patient care, medical errors, and patient dissatisfaction. Differential communication also leads to health care disparities.
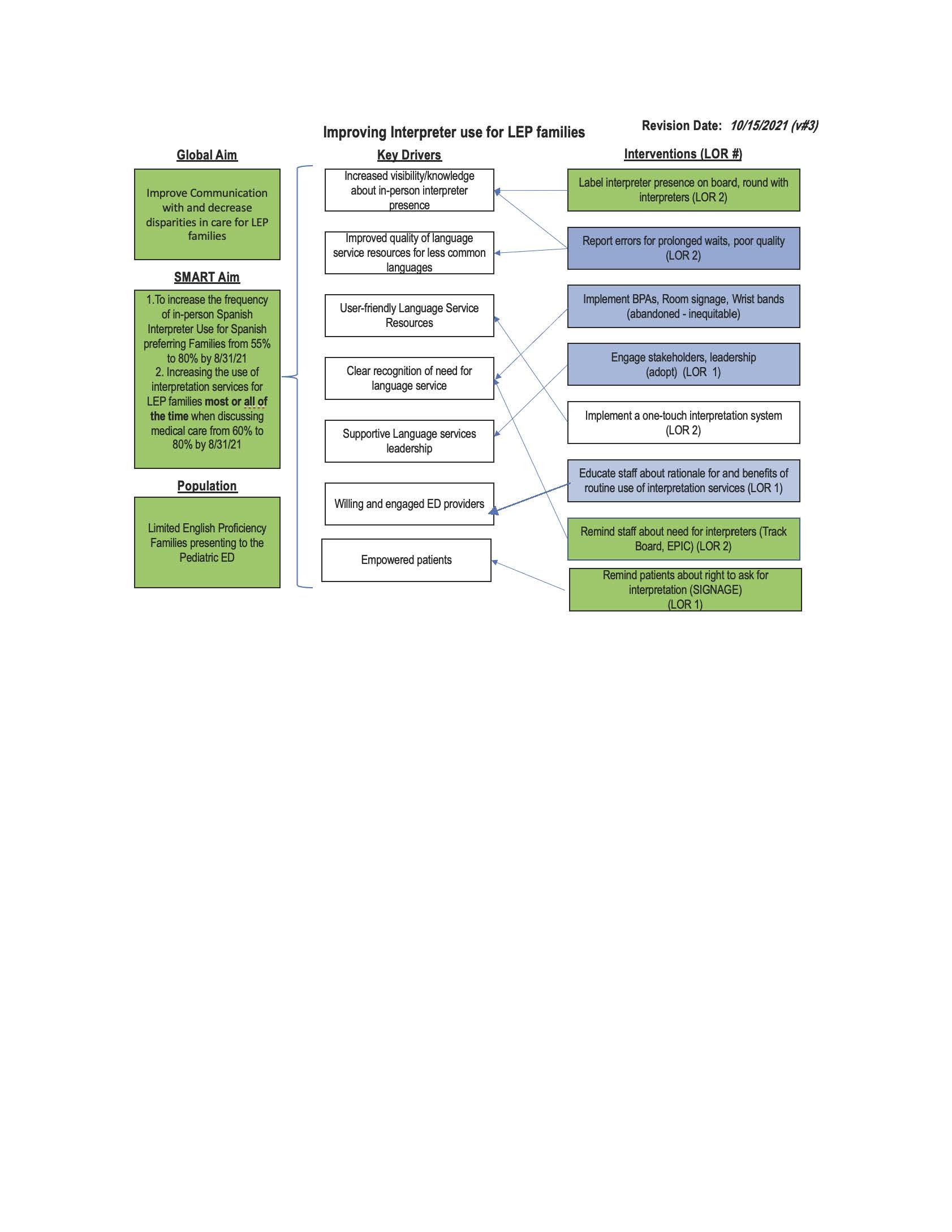
Objective: We aimed to improve communication with and decrease disparities in the care of Limited English Proficiency (LEP) families in our Pediatric Emergency Department (PED). Our objectives were to increase the frequency of 1) in-person Spanish interpreter use from 55 % to 80 % of encounters and 2) any interpreter use (in-person, video, or phone) to “most” or “all of the time” from 60 to 80% within 12 months.
Design/Methods: Using the Model for Improvement approach, we formed a team of PED providers and language service, patient, and informatics representatives to identify barriers to and analyze the process of using interpreters. Baseline data collection included ED staff and family interviews to identify barriers, electronic record data to examine Spanish interpreter use, and surveys of LEP families to assess the frequency of any interpreter use. Using a Plan, Do, Study, Act approach, we tested, refined, and implemented interventions.
Results: Provider barriers (Fig 1) included lack of knowledge of in-person interpreter presence and prolonged waits for less prevalent languages (eg, Pashto). LEP caregivers (n=70) recommended consistent use of interpreters throughout the visit, favored in-person interpretation and advised against using family members for interpretation. Interview data and visual representation of the system helped identify key drivers in the process (Fig 2). Interventions included leadership engagement, provider education, initiation of a process of “rounding” with interpreters, use of the electronic track board to highlight language preference, event reporting for prolonged waits for less prevalent languages and signage reminding patients of their right to interpretive services.
We measured the percent of Spanish families for whom in-person interpretation was used with a statistical control (p) chart, using cohorts of 20 patients. Evidence of special cause variation with 2 shifts in the center line, reflecting 8 data points to one side of the center line, was identified beginning in 10/14/21 with average in-person interpretation use increasing to 68% (Fig 3). Conclusion(s): Using targeted interventions, we increased the use of in-person interpreters. Patient surveys will provide additional data on the use of any interpreters. Ongoing work includes implementing one-step video interpretation and decreasing waits for languages less prevalent in our local community.
GauthamiSomaCV11.30.pdf
Figure 2: Key Driver Diagram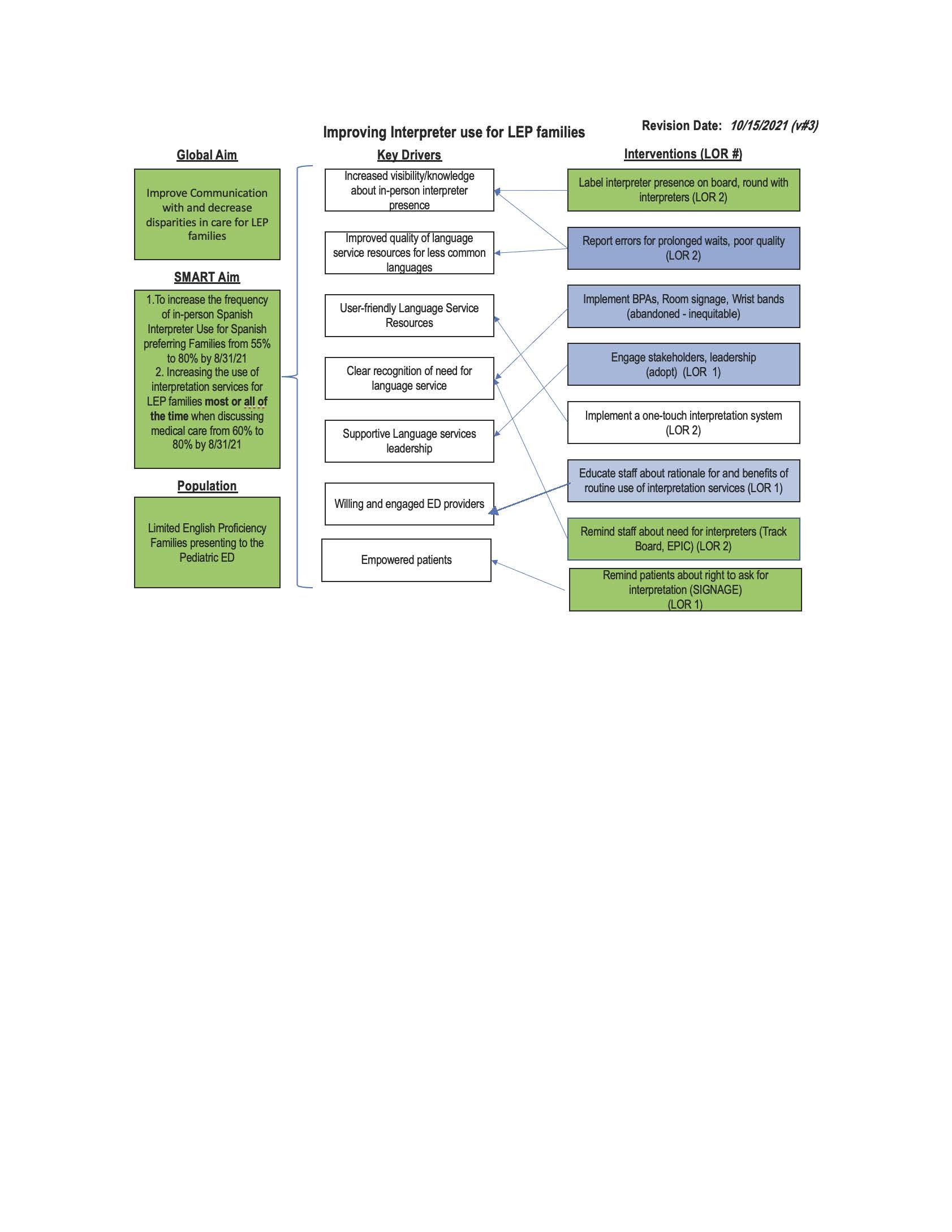
Objective: We aimed to improve communication with and decrease disparities in the care of Limited English Proficiency (LEP) families in our Pediatric Emergency Department (PED). Our objectives were to increase the frequency of 1) in-person Spanish interpreter use from 55 % to 80 % of encounters and 2) any interpreter use (in-person, video, or phone) to “most” or “all of the time” from 60 to 80% within 12 months.
Design/Methods: Using the Model for Improvement approach, we formed a team of PED providers and language service, patient, and informatics representatives to identify barriers to and analyze the process of using interpreters. Baseline data collection included ED staff and family interviews to identify barriers, electronic record data to examine Spanish interpreter use, and surveys of LEP families to assess the frequency of any interpreter use. Using a Plan, Do, Study, Act approach, we tested, refined, and implemented interventions.
Results: Provider barriers (Fig 1) included lack of knowledge of in-person interpreter presence and prolonged waits for less prevalent languages (eg, Pashto). LEP caregivers (n=70) recommended consistent use of interpreters throughout the visit, favored in-person interpretation and advised against using family members for interpretation. Interview data and visual representation of the system helped identify key drivers in the process (Fig 2). Interventions included leadership engagement, provider education, initiation of a process of “rounding” with interpreters, use of the electronic track board to highlight language preference, event reporting for prolonged waits for less prevalent languages and signage reminding patients of their right to interpretive services.
We measured the percent of Spanish families for whom in-person interpretation was used with a statistical control (p) chart, using cohorts of 20 patients. Evidence of special cause variation with 2 shifts in the center line, reflecting 8 data points to one side of the center line, was identified beginning in 10/14/21 with average in-person interpretation use increasing to 68% (Fig 3). Conclusion(s): Using targeted interventions, we increased the use of in-person interpreters. Patient surveys will provide additional data on the use of any interpreters. Ongoing work includes implementing one-step video interpretation and decreasing waits for languages less prevalent in our local community.
GauthamiSomaCV11.30.pdf
Figure 2: Key Driver Diagram