Back
Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement V
391 - Improving Postpartum Depression Screening in a Level IV NICU: Utilizing Health Professional Students to Improve Outreach
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 391
Publication Number: 391.435
Publication Number: 391.435
Sinead Brady, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Sandhya S. Brachio, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Rachel S. Kim, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Rochelle Steinwurtzel, Columbia University Vagelos College of Physicians and Surgeons, Hastings On Hudson, NY, United States; Elena Abascal, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States
.jpg)
Sinead Brady, MD (she/her/hers)
Fellow
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Infants born to mothers struggling with postpartum depression (PPD) are at risk for adverse developmental outcomes. Mothers of premature infants are 40% more likely to develop PPD when compared to the general population. Our NICU utilized the IHI Model for Improvement to institute a PPD screening program that centered around bedside screening. With the COVID-19 pandemic, hospital policy shifted to only allow one parent at the bedside at any time. During this time, medicine and public health students formed the COVID-19 Student Service Corps to help improve outreach. This provided an opportunity to adjust our screening program to meet the parents' needs during this difficult time. Adjusting to the current environment was vital to ensure that the NICU continues to identify and refer parents to appropriate mental health resources.
Objective: We utilized a multidisciplinary team approach to develop strategies to screen for PPD in parents whose infant was admitted to our NICU beyond 2 weeks of age. Our initial screening process increased our screening rates from 0% to a baseline of 27%; with the incorporation of health professional students, we have established a new baseline of 55% over the past 6 months, and aim to improve this rate to 100% by June 2022.
Design/Methods: The IHI Model for Improvement was used as a framework for this project. Participants included NICU physicians, physician extenders, registered nurses, health professional students and caregivers of patients admitted to the NICU. Major interventions included provider education, identification of parents to be screened, weekly telephone screening of parents by health professional students, and utilization of the electronic medical record for notification of providers and social workers of screening results.
Results: The run chart(Figure 1) displays the rates of parents appropriately screened with the PHQ-2. Currently, 55% of qualifying families are screened appropriately with the PHQ-2. Of the parents screened, 25% of parents had a positive PHQ-9 requiring referral to higher level services.Conclusion(s): Implementation of a postpartum depression screening program that complies with the AAP standard is feasible within a level 4 NICU, even under extreme circumstances secondary to the COVID-19 pandemic. This type of program has a clear need within the NICU given the high percentage of parents with postpartum depression who were identified with appropriate screening. Utilizing health professional students greatly improved our ability to screen parents. This underutilized resource may help expand parent outreach efforts with other projects.
Percentage of Qualifying Parents Reached for Postpartum Depression Screening By Week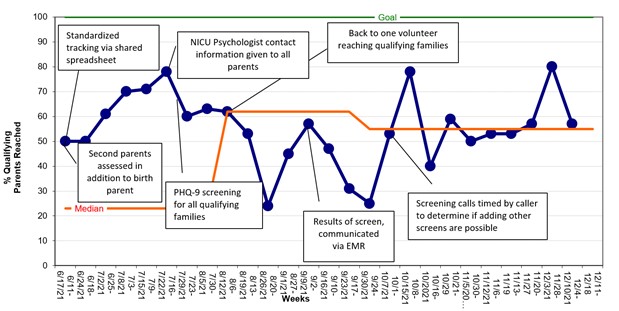 Figure 1: Run chart of weekly screening of qualifying families with PHQ-2; x-axis - week, y-axis – weekly screening rate (%)
Figure 1: Run chart of weekly screening of qualifying families with PHQ-2; x-axis - week, y-axis – weekly screening rate (%)
Objective: We utilized a multidisciplinary team approach to develop strategies to screen for PPD in parents whose infant was admitted to our NICU beyond 2 weeks of age. Our initial screening process increased our screening rates from 0% to a baseline of 27%; with the incorporation of health professional students, we have established a new baseline of 55% over the past 6 months, and aim to improve this rate to 100% by June 2022.
Design/Methods: The IHI Model for Improvement was used as a framework for this project. Participants included NICU physicians, physician extenders, registered nurses, health professional students and caregivers of patients admitted to the NICU. Major interventions included provider education, identification of parents to be screened, weekly telephone screening of parents by health professional students, and utilization of the electronic medical record for notification of providers and social workers of screening results.
Results: The run chart(Figure 1) displays the rates of parents appropriately screened with the PHQ-2. Currently, 55% of qualifying families are screened appropriately with the PHQ-2. Of the parents screened, 25% of parents had a positive PHQ-9 requiring referral to higher level services.Conclusion(s): Implementation of a postpartum depression screening program that complies with the AAP standard is feasible within a level 4 NICU, even under extreme circumstances secondary to the COVID-19 pandemic. This type of program has a clear need within the NICU given the high percentage of parents with postpartum depression who were identified with appropriate screening. Utilizing health professional students greatly improved our ability to screen parents. This underutilized resource may help expand parent outreach efforts with other projects.
Percentage of Qualifying Parents Reached for Postpartum Depression Screening By Week
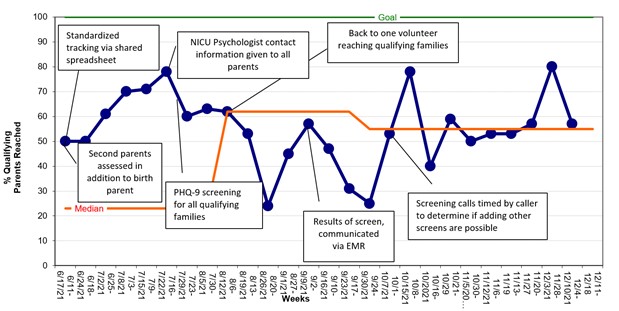 Figure 1: Run chart of weekly screening of qualifying families with PHQ-2; x-axis - week, y-axis – weekly screening rate (%)
Figure 1: Run chart of weekly screening of qualifying families with PHQ-2; x-axis - week, y-axis – weekly screening rate (%)