Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement IV: Respiratory and Temperature Regulation
380 - Model for Extubation Readiness in Extremely Preterm Infants in NICU patients at the Children’s Hospital of The King’s Daughters
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 380
Publication Number: 380.434
Publication Number: 380.434
Daley Owens, Eastern Virginia Medical School, Norfolk, VA, United States; Kaila Lessner, EVMS/ CHKD, Norfolk, VA, United States; Turaj Vazifedan, Eastern Virginia Medical School, Norfolk, VA, United States; Haree Pallera, Eastern Virginia Medical School, Virginia Beach, VA, United States; Brett Siegfried, CHKD/EVMS, Norfolk, VA, United States
Daley Owens, MD (she/her/hers)
Resident Physician
Eastern Virginia Medical School
Norfolk, Virginia, United States
Presenting Author(s)
Background: Prolonged mechanical ventilation in premature infants is associated with development of bronchopulmonary dysplasia (BPD), affecting 15,000 US infants annually. Early extubation may reduce this risk. However, there are no standardized guidelines for elective extubation.
Objective: Evaluate the Wayne State Extubation Success Calculator (ESC) validity to predict the success of an elective extubation in a preterm infant. Primary outcome is successful extubation (96 hours without re-intubation). Secondary outcome is the correlation of the calculated ESC probability with successful extubation.
Design/Methods:
Two-year retrospective study of 311 infants at the Children’s Hospital of King’s Daughters NICU. Inclusion criteria: Infants with birth weight ≤ 1250 grams and electively extubated within 60 days of age. ESC used the following variables to calculate a percent value: gestational age (GA), age at extubation, pre-extubation FiO2, peak respiratory severity score (RSS) at 6 hours of life, weight at extubation and pre-extubation pH. Excluded deceased infants prior to extubation and infants missing documented variable information. Acknowledge attrition bias with exclusion of 128 screened infants. Generalized Linear Model (GLM) evaluated the secondary outcome and the association between successful extubation and each variable. Dominance analysis (DA) compared the relative importance of variables in the GLM. Validated results using a bootstrapping technique with 1000 replication. All statistical tests were two-sided using R Studio and SPSS 26 (Chicago, IL).
Results: Of the 183 infants included in the study, 151 were successfully extubated. A higher ESC probability was associated with successful extubation, OR=1.05, 95% CI (1.03, 1.07), p< 0.001. Associations were found between successful extubation and GA (p=0.002), PMA at extubation (p=0.002), pre-extubation FiO2 (p=0.015) and pre-extubation RSS (p=0.021). Demonstrated sensitivity/specificity of 34%/97%, 47%/90%, and 66%/76% for cutoff of 60%, 70%, and 80% probability of extubation success, respectively. DA showed GA to be the most important predictor, followed by age at extubation, pre-extubation FiO2, pre-extubation pH, weight at extubation and peak RSS in first 6 hours.Conclusion(s): The ESC is a valid tool that predicts extubation success for a preterm infant. Higher GA is most influential of ESC results. Implementation of this ESC as an objective clinical decision-making tool to guide early extubation and possibly reduce the incidence of BPD should be considered. Further research is needed to determine how to improve the tool to increase sensitivity.
Primary and Secondary Outcomes.jpg) The corresponding AUC for this model was calculated as 0.772, 95% CI (0.674, 0.871). Moreover, the model had sensitivity/specificity of 34%/97%, 47%/90%, and 66%/76% for cutoff of 60%, 70%, and 80% probability of extubation success, respectively.
The corresponding AUC for this model was calculated as 0.772, 95% CI (0.674, 0.871). Moreover, the model had sensitivity/specificity of 34%/97%, 47%/90%, and 66%/76% for cutoff of 60%, 70%, and 80% probability of extubation success, respectively.
Generalized Linear Model of Extubation Success Calculator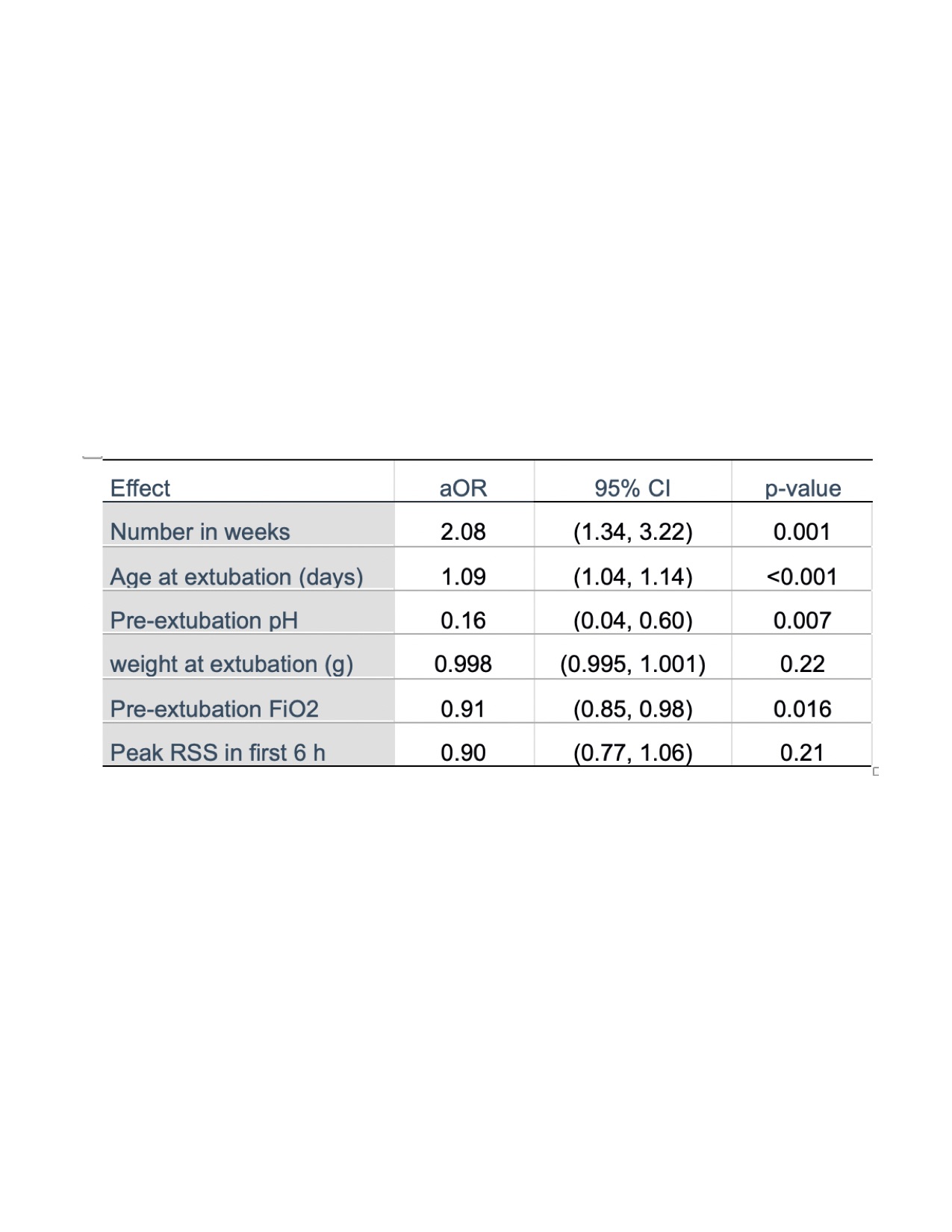 There was a significant association between remaining extubated more than 96 hours and number in weeks (p=0.001), age at extubation (p < 0.001), pre-extubation pH (p=0.007), and pre-extubation FiO2 (p=0.016),
There was a significant association between remaining extubated more than 96 hours and number in weeks (p=0.001), age at extubation (p < 0.001), pre-extubation pH (p=0.007), and pre-extubation FiO2 (p=0.016),
Objective: Evaluate the Wayne State Extubation Success Calculator (ESC) validity to predict the success of an elective extubation in a preterm infant. Primary outcome is successful extubation (96 hours without re-intubation). Secondary outcome is the correlation of the calculated ESC probability with successful extubation.
Design/Methods:
Two-year retrospective study of 311 infants at the Children’s Hospital of King’s Daughters NICU. Inclusion criteria: Infants with birth weight ≤ 1250 grams and electively extubated within 60 days of age. ESC used the following variables to calculate a percent value: gestational age (GA), age at extubation, pre-extubation FiO2, peak respiratory severity score (RSS) at 6 hours of life, weight at extubation and pre-extubation pH. Excluded deceased infants prior to extubation and infants missing documented variable information. Acknowledge attrition bias with exclusion of 128 screened infants. Generalized Linear Model (GLM) evaluated the secondary outcome and the association between successful extubation and each variable. Dominance analysis (DA) compared the relative importance of variables in the GLM. Validated results using a bootstrapping technique with 1000 replication. All statistical tests were two-sided using R Studio and SPSS 26 (Chicago, IL).
Results: Of the 183 infants included in the study, 151 were successfully extubated. A higher ESC probability was associated with successful extubation, OR=1.05, 95% CI (1.03, 1.07), p< 0.001. Associations were found between successful extubation and GA (p=0.002), PMA at extubation (p=0.002), pre-extubation FiO2 (p=0.015) and pre-extubation RSS (p=0.021). Demonstrated sensitivity/specificity of 34%/97%, 47%/90%, and 66%/76% for cutoff of 60%, 70%, and 80% probability of extubation success, respectively. DA showed GA to be the most important predictor, followed by age at extubation, pre-extubation FiO2, pre-extubation pH, weight at extubation and peak RSS in first 6 hours.Conclusion(s): The ESC is a valid tool that predicts extubation success for a preterm infant. Higher GA is most influential of ESC results. Implementation of this ESC as an objective clinical decision-making tool to guide early extubation and possibly reduce the incidence of BPD should be considered. Further research is needed to determine how to improve the tool to increase sensitivity.
Primary and Secondary Outcomes
.jpg) The corresponding AUC for this model was calculated as 0.772, 95% CI (0.674, 0.871). Moreover, the model had sensitivity/specificity of 34%/97%, 47%/90%, and 66%/76% for cutoff of 60%, 70%, and 80% probability of extubation success, respectively.
The corresponding AUC for this model was calculated as 0.772, 95% CI (0.674, 0.871). Moreover, the model had sensitivity/specificity of 34%/97%, 47%/90%, and 66%/76% for cutoff of 60%, 70%, and 80% probability of extubation success, respectively.Generalized Linear Model of Extubation Success Calculator
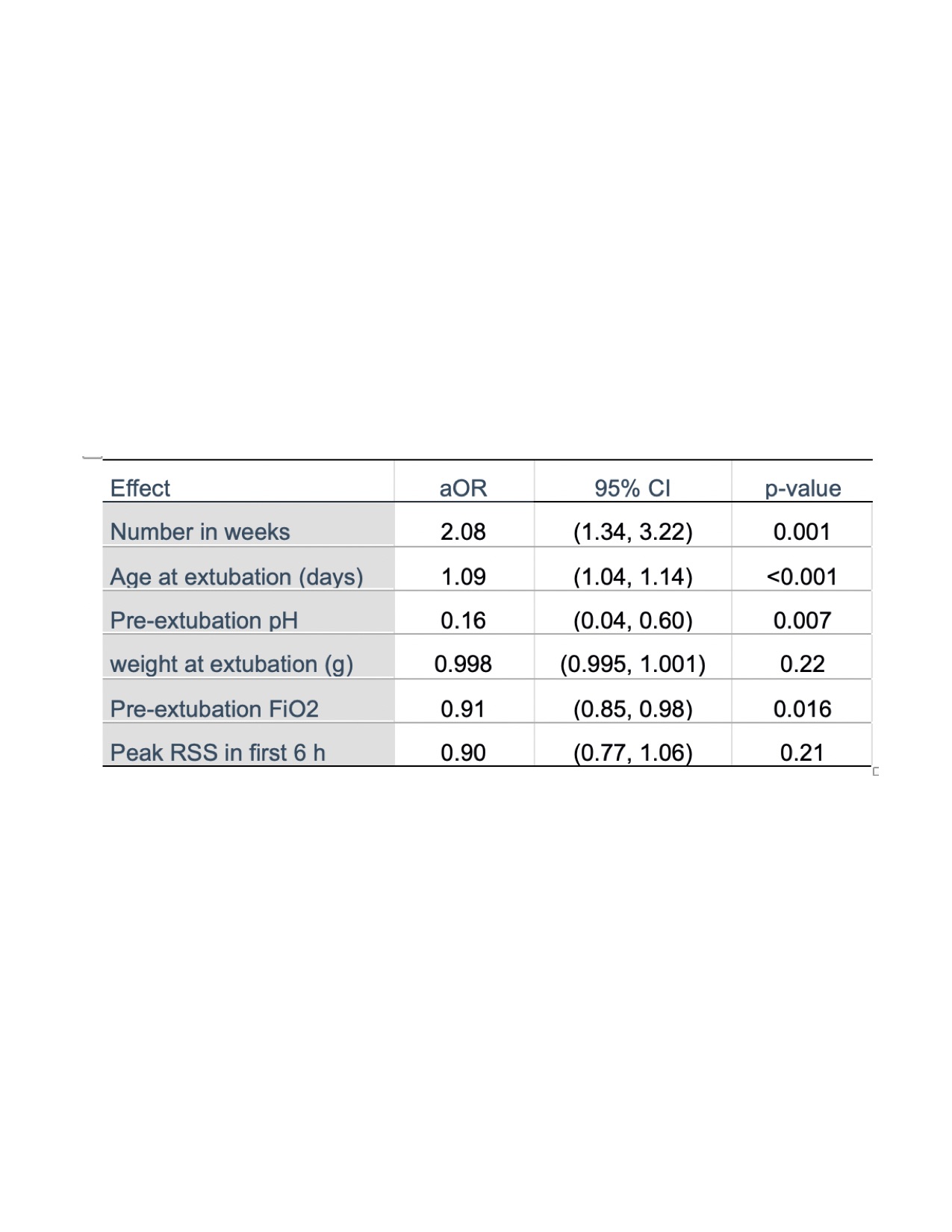 There was a significant association between remaining extubated more than 96 hours and number in weeks (p=0.001), age at extubation (p < 0.001), pre-extubation pH (p=0.007), and pre-extubation FiO2 (p=0.016),
There was a significant association between remaining extubated more than 96 hours and number in weeks (p=0.001), age at extubation (p < 0.001), pre-extubation pH (p=0.007), and pre-extubation FiO2 (p=0.016),