Medical Education: Simulation & Technology
Category: Abstract Submission
Medical Education 11 - Medical Education: Simulation & Technology II
272 - Impact of video laryngoscopy-enhanced advanced airway curriculum for learners in the neonatal intensive care unit.
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 272
Publication Number: 272.331
Publication Number: 272.331
Christine Yankowski, Christiana Care, Newark, DE, United States; Rula Nassar, Christiana Care Health System, Newark, DE, United States; Kelley Z. Kovatis, Christiana Care, Philadelphia, PA, United States
- CY
Christine Yankowski, DO
Attending Physician
Christiana Care
Newark, Delaware, United States
Presenting Author(s)
Background: Neonatal intubation (NI) is an important intervention in the resuscitation of critically ill neonates. Improving competency with NI skills during pediatric training is challenging due to limited teaching opportunities. Video laryngoscopy (VL) may be an effective teaching tool during simulation and improve clinical intubation success but this has not been previously studied.
Objective: The study objective was to determine the impact of a VL intubation and standard direct laryngoscopy (DL) intubation curriculum on 1) time to successful intubation and number of intubation attempts during a simulated intubation, 2) perceived intubation competency, and 3) DL intubation success rates in neonatal patient encounters.
Design/Methods: Neonatal learners with < 1 year NI experience were randomized to either VL/DL or standard DL intubation curriculums during their neonatal rotations. Participants remained in assigned group throughout the study period and completed the curriculum during each rotation. Both groups received a short presentation on NI procedure followed by hands-on procedural simulation training using either VL/DL or DL. Simulated DL intubation attempts were recorded and timed for both groups. Participants completed surveys prior to the initial curriculum and after each subsequent session. Patient intubation attempts in clinical setting were collected.
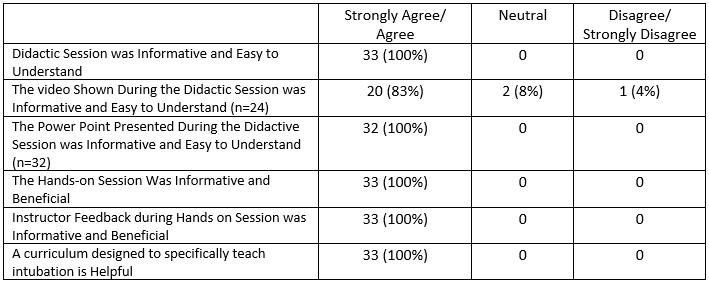
Results: A total of 49 learners were enrolled: 25 in the VL group and 24 in the standard DL group. Response to feedback survey was 67%. Learners had little experience and confidence in their ability to perform NI prior to participation (Table 1). Participants perceived the hands-on and instructor portions of the curriculum as most helpful and informative (Table 2). There were no differences in evaluation of the curriculum (p >.70 for all questions), successful first attempts (p=.31), or time to intubation (p=.33). Compared to the VL/DL curriculum, participants in the standard DL curriculum were more successful in the clinical setting (70% vs 33%, p=.048). When only residents were included this trend remained but was no longer statistically significant (77% vs 33%, p=.164). Curriculum did not predict intubation clinical success in a logistical regression model but this may reflect the small sample size (p=.77).Conclusion(s): A hands-on interactive intubation curriculum is viewed by novice learners as beneficial. This pilot suggests a VL educational curriculum could negatively impact early learners DL intubation skills. Our study highlights the need for further investigation on how VL/DL intubation technique translate from an education to clinical setting.
Table 1: Summary Data at the Time of Enrollment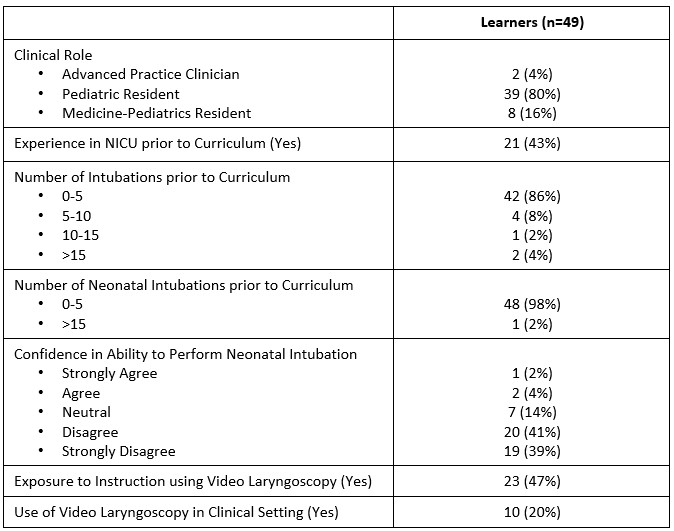
Table 2: Feedback on Intubation Curriculum (n=33)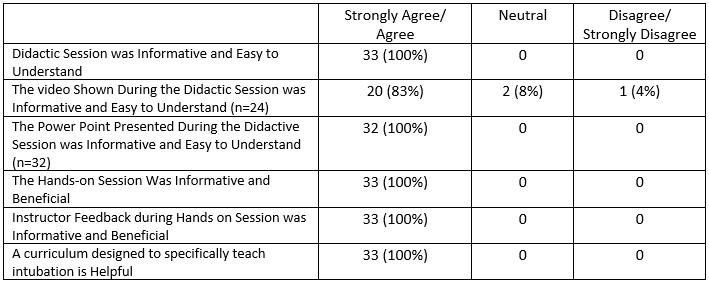
Objective: The study objective was to determine the impact of a VL intubation and standard direct laryngoscopy (DL) intubation curriculum on 1) time to successful intubation and number of intubation attempts during a simulated intubation, 2) perceived intubation competency, and 3) DL intubation success rates in neonatal patient encounters.
Design/Methods: Neonatal learners with < 1 year NI experience were randomized to either VL/DL or standard DL intubation curriculums during their neonatal rotations. Participants remained in assigned group throughout the study period and completed the curriculum during each rotation. Both groups received a short presentation on NI procedure followed by hands-on procedural simulation training using either VL/DL or DL. Simulated DL intubation attempts were recorded and timed for both groups. Participants completed surveys prior to the initial curriculum and after each subsequent session. Patient intubation attempts in clinical setting were collected.
Results: A total of 49 learners were enrolled: 25 in the VL group and 24 in the standard DL group. Response to feedback survey was 67%. Learners had little experience and confidence in their ability to perform NI prior to participation (Table 1). Participants perceived the hands-on and instructor portions of the curriculum as most helpful and informative (Table 2). There were no differences in evaluation of the curriculum (p >.70 for all questions), successful first attempts (p=.31), or time to intubation (p=.33). Compared to the VL/DL curriculum, participants in the standard DL curriculum were more successful in the clinical setting (70% vs 33%, p=.048). When only residents were included this trend remained but was no longer statistically significant (77% vs 33%, p=.164). Curriculum did not predict intubation clinical success in a logistical regression model but this may reflect the small sample size (p=.77).Conclusion(s): A hands-on interactive intubation curriculum is viewed by novice learners as beneficial. This pilot suggests a VL educational curriculum could negatively impact early learners DL intubation skills. Our study highlights the need for further investigation on how VL/DL intubation technique translate from an education to clinical setting.
Table 1: Summary Data at the Time of Enrollment
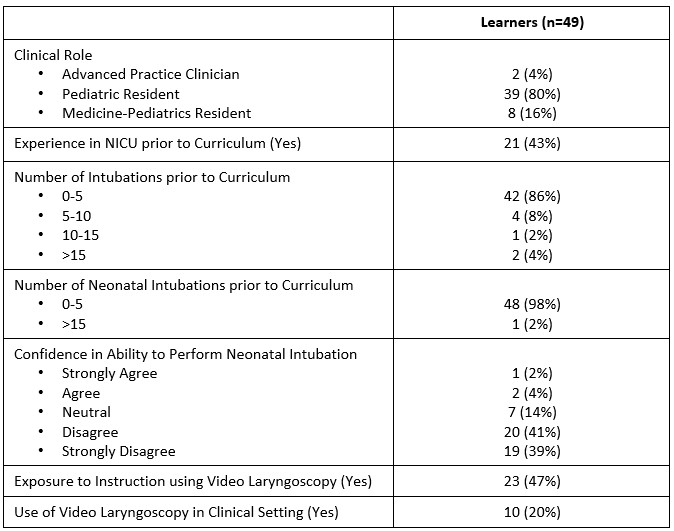
Table 2: Feedback on Intubation Curriculum (n=33)