Neonatal Respiratory Assessment/Support/Ventilation
Category: Abstract Submission
Neonatal Respiratory III: BPD
469 - Use of inhaled nitric oxide in extremely preterm infants with hypoxemic respiratory failure: factors affecting the therapeutic response
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 469
Publication Number: 469.229
Publication Number: 469.229
Shuntaro Oka, Saitama Medical Center, Kawagoe, Saitama, Japan; Kazuhiko Kabe, Saitama Medical Univ. Saitama Medical Center, Kawagoe City, Saitama, Japan; Fumihiko Namba, Saitama Medical Center, Saitama Medical University, Kawagoe, Saitama, Japan
- SO
Shuntaro Oka, n/a
assistant professor
Saitama Medical Center
Kawagoe, Saitama, Japan
Presenting Author(s)
Background: Inhaled nitric oxide (iNO) improves oxygenation through enhanced ventilation–perfusion matching. Although iNO therapy has often been used as a rescue treatment for hypoxemic respiratory failure in preterm infants with bronchopulmonary dysplasia (BPD), its efficacy remains controversial.
Objective: We aimed to investigate the effect of iNO therapy on hypoxemic respiratory failure in extremely preterm infants.
Design/Methods: Neonatal intensive care unit charts were reviewed retrospectively. Extremely preterm infants ( < 28 weeks) who had received iNO therapy between 2013 and 2020 were included. Infants treated with iNO only for persistent pulmonary hypertension of the newborn (PPHN) were excluded. The oxygen saturation index (OSI) was used as a non-invasive diagnostic parameter of oxygenation.
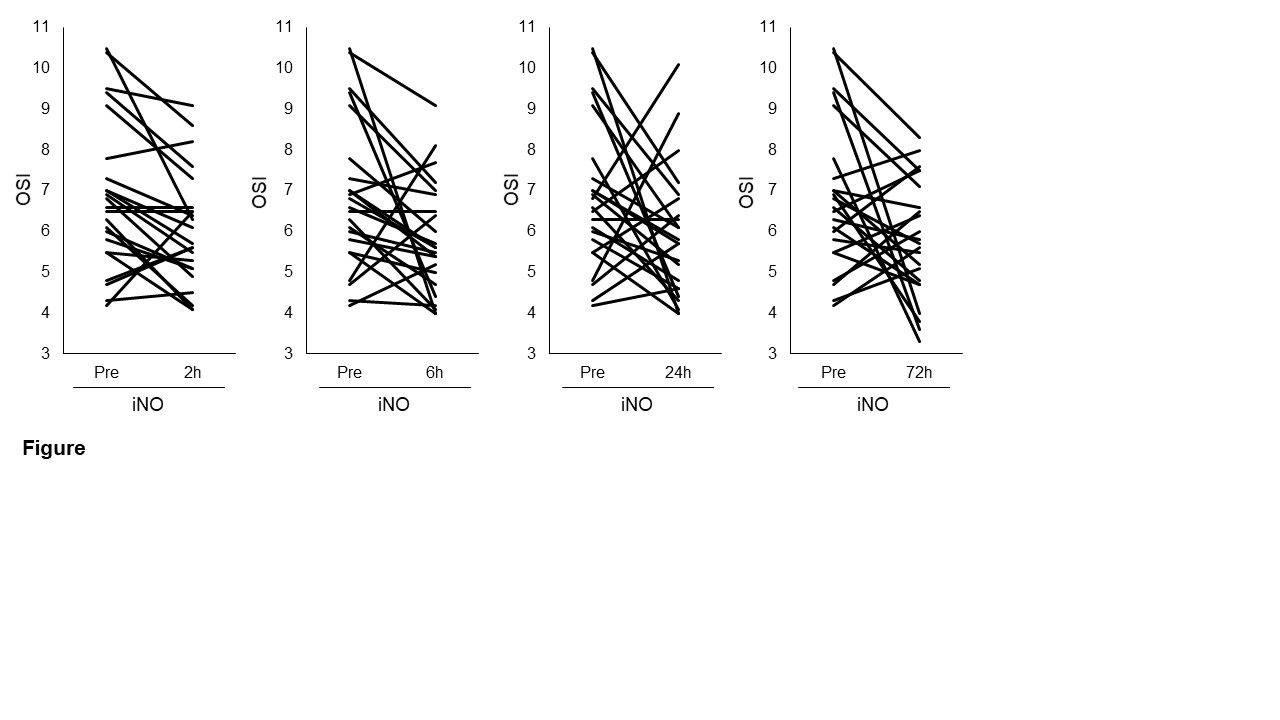
Results: Of the 354 extremely preterm infants, 58 were treated with iNO. After excluding 28 infants treated with iNO only for PPHN, the remaining 30 were included in this study. The median gestational age was 24.6 (interquartile range, 23.1–25.7) weeks, and the median birth weight was 620 (482–814) grams. Twenty-five infants (83%) had BPD, and 24 (80%) had bubbly/cystic appearance on the chest X-ray. Oxygenation improved within 6 hours in extremely preterm infants who received iNO therapy for hypoxemic respiratory failure (figure) . Within the first 6 hours of iNO therapy, OSI decreased by more than 20% in 12 infants (40%, positive response group) but did not decrease in 17 infants (57%, negative response group). One infant died 4 hours after birth, and was not included in either group. There were no significant differences in gestational age, birth weight, sex, frequency of chorioamnionitis, or prematurity-related complications, including BPD, necrotizing enterocolitis, retinopathy of prematurity, and intraventricular hemorrhage, between the positive and negative response groups. The rate of oligohydramnios was higher in the positive response group when compared with the negative response group (4 (33%) vs. 0 (0%), p = 0.02). In addition, when compared with the negative response group, the positive response group had received iNO therapy earlier after birth (day 12 (10–19) vs. 26 (14–28), p = 0.03).Conclusion(s): There was a higher rate of oligohydramnios in the positive response group, which suggests that iNO therapy may be effective in infants with arrested or delayed lung development due to oligohydramnios. The long-term efficacy of iNO therapy needs to be investigated by conducting further studies.
figure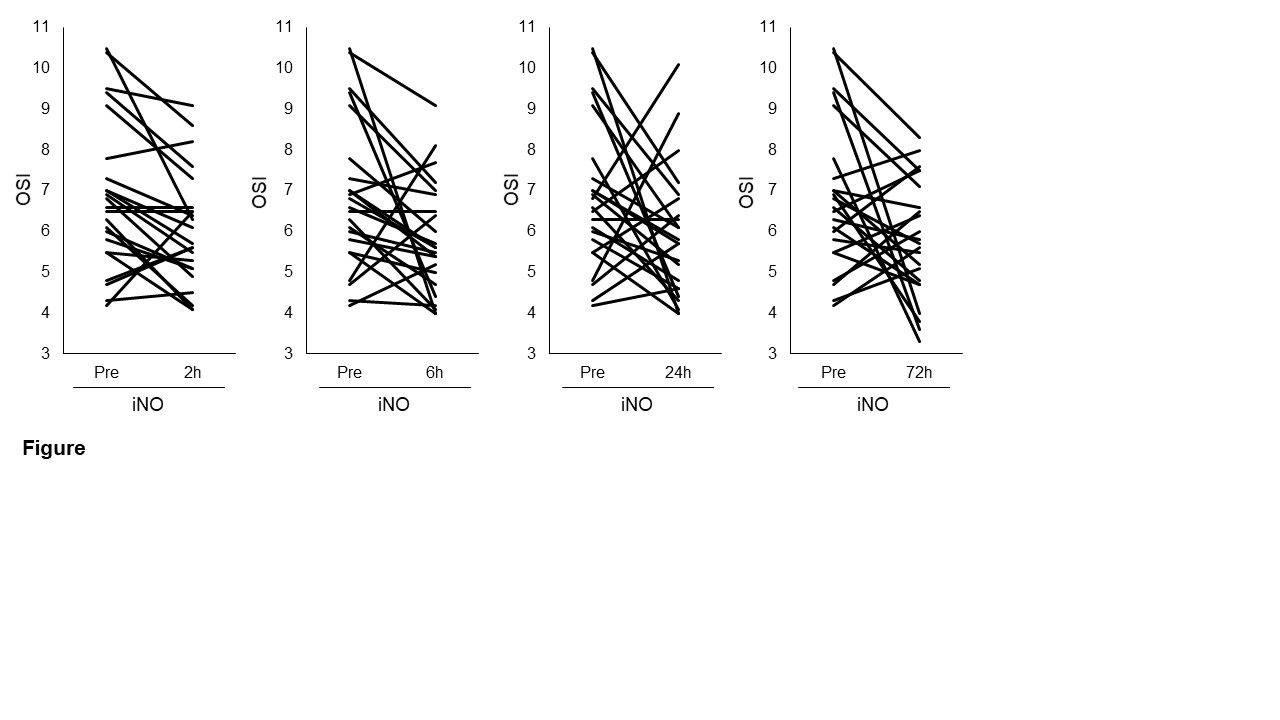
Objective: We aimed to investigate the effect of iNO therapy on hypoxemic respiratory failure in extremely preterm infants.
Design/Methods: Neonatal intensive care unit charts were reviewed retrospectively. Extremely preterm infants ( < 28 weeks) who had received iNO therapy between 2013 and 2020 were included. Infants treated with iNO only for persistent pulmonary hypertension of the newborn (PPHN) were excluded. The oxygen saturation index (OSI) was used as a non-invasive diagnostic parameter of oxygenation.
Results: Of the 354 extremely preterm infants, 58 were treated with iNO. After excluding 28 infants treated with iNO only for PPHN, the remaining 30 were included in this study. The median gestational age was 24.6 (interquartile range, 23.1–25.7) weeks, and the median birth weight was 620 (482–814) grams. Twenty-five infants (83%) had BPD, and 24 (80%) had bubbly/cystic appearance on the chest X-ray. Oxygenation improved within 6 hours in extremely preterm infants who received iNO therapy for hypoxemic respiratory failure (figure) . Within the first 6 hours of iNO therapy, OSI decreased by more than 20% in 12 infants (40%, positive response group) but did not decrease in 17 infants (57%, negative response group). One infant died 4 hours after birth, and was not included in either group. There were no significant differences in gestational age, birth weight, sex, frequency of chorioamnionitis, or prematurity-related complications, including BPD, necrotizing enterocolitis, retinopathy of prematurity, and intraventricular hemorrhage, between the positive and negative response groups. The rate of oligohydramnios was higher in the positive response group when compared with the negative response group (4 (33%) vs. 0 (0%), p = 0.02). In addition, when compared with the negative response group, the positive response group had received iNO therapy earlier after birth (day 12 (10–19) vs. 26 (14–28), p = 0.03).Conclusion(s): There was a higher rate of oligohydramnios in the positive response group, which suggests that iNO therapy may be effective in infants with arrested or delayed lung development due to oligohydramnios. The long-term efficacy of iNO therapy needs to be investigated by conducting further studies.
figure