Infectious Diseases
Category: Abstract Submission
Infectious Diseases: COVID-19
291 - A Multicenter study of hospital course, resource utilization, and outcomes of children with COVID-19 infection and pre-existing conditions
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 291
Publication Number: 291.215
Publication Number: 291.215
Prithvi Raj Sendi Keshavamurthy, Nicklaus Children’s Hospital, Miami, FL, United States; Meghana Nadiger, OSF Children’s hospital of Illinois/ University of Illinois College of Medicine at Peoria, Dunlap, IL, United States; Utpal Bhalala, Driscoll Children’s Hospital, Corpus Christi, TX, United States; Paul A. Martinez, Nicklaus Children’s Hospital, Miami, FL, United States; Balagangadhar R. Totapally, Nicklaus Children’s Hospital, Miami, FL, United States

Prithvi Raj Sendi Keshavamurthy, MD
Clinical Assistant Professor of Pediatrics
Nicklaus Children’s Hospital
Miami, Florida, United States
Presenting Author(s)
Background: Children with underlying pre-existing conditions are at a higher risk for respiratory illness and mortality compared to healthy children. Although COVID-19 infection in children is known to cause mild symptoms, some children could develop a severe life-threatening infection. Data on COVID-19 infection in children with a pre-existing condition is sparse.
Objective: The study aimed to compare hospital course, resource utilization, and outcomes in children with and without pre-existing conditions and COVID-19 infection.
Design/Methods: A retrospective analysis using the Viral Infection and Respiratory illness Universal Study (VIRUS) COVID-19 registry from the Society of Critical Care Medicine was performed. Hospitalized children from age 0 to 18 years with COVID-19 infection from 51 centers were included. Categorical variables were analyzed using the chi-square test, continuous variables were compared with the Mann-Whitney U test and binomial data are presented as odds ratios with 95% CI. A P-value less than 0.05 was considered statistically significant. SPSS was used for statistical analysis.
Results: Among 1059 patients included in the analysis, 440 (41.5%) children had an underlying pre-existing condition. The demographic differences between the two groups are presented in Table 1. Children with the pre-existing condition were more likely to present with cough (31.8 Vs.22.0), dyspnea (32.5% Vs. 17.4%), and seizures (6.8% Vs 2.7%, Table 1). Multisystem inflammatory syndrome (MISC) was less commonly observed in children with pre-existing conditions (21.6% Vs 35.0%, OR=0.51, 95% CI: 0.38-0.68). Children with pre-existing conditions were more often admitted to the PICU (52.4% vs 43.1%, OR=1.45, 95% CI: 1.13-1.86), required high flow nasal cannula (20.6% Vs 9.3%), noninvasive mechanical ventilation (12.7% Vs 6.2%), and invasive mechanical ventilation (14.2% Vs 8.8%, Table 2) and had a longer duration of oxygen support (Table 3). The rates of inotrope use, CPR, and mortality were similar in the two groups. The hospital LOS was higher in patients with pre-existing conditions (median = 14.3 Vs 7.5 days, p = 0.004).Conclusion(s): Our multicenter study demonstrates that children with pre-existing conditions and COVID-19 infection are less likely to present with MISC and more often require respiratory support and have a longer length of stay. Our study adds to the knowledge of COVID-19 infection in the vulnerable population of children with pre-existing conditions.
Table 1. Demographic characteristics and presenting signs and symptoms of children with pre-existing condition and children with no pre-existing condition and COVID-19 infection.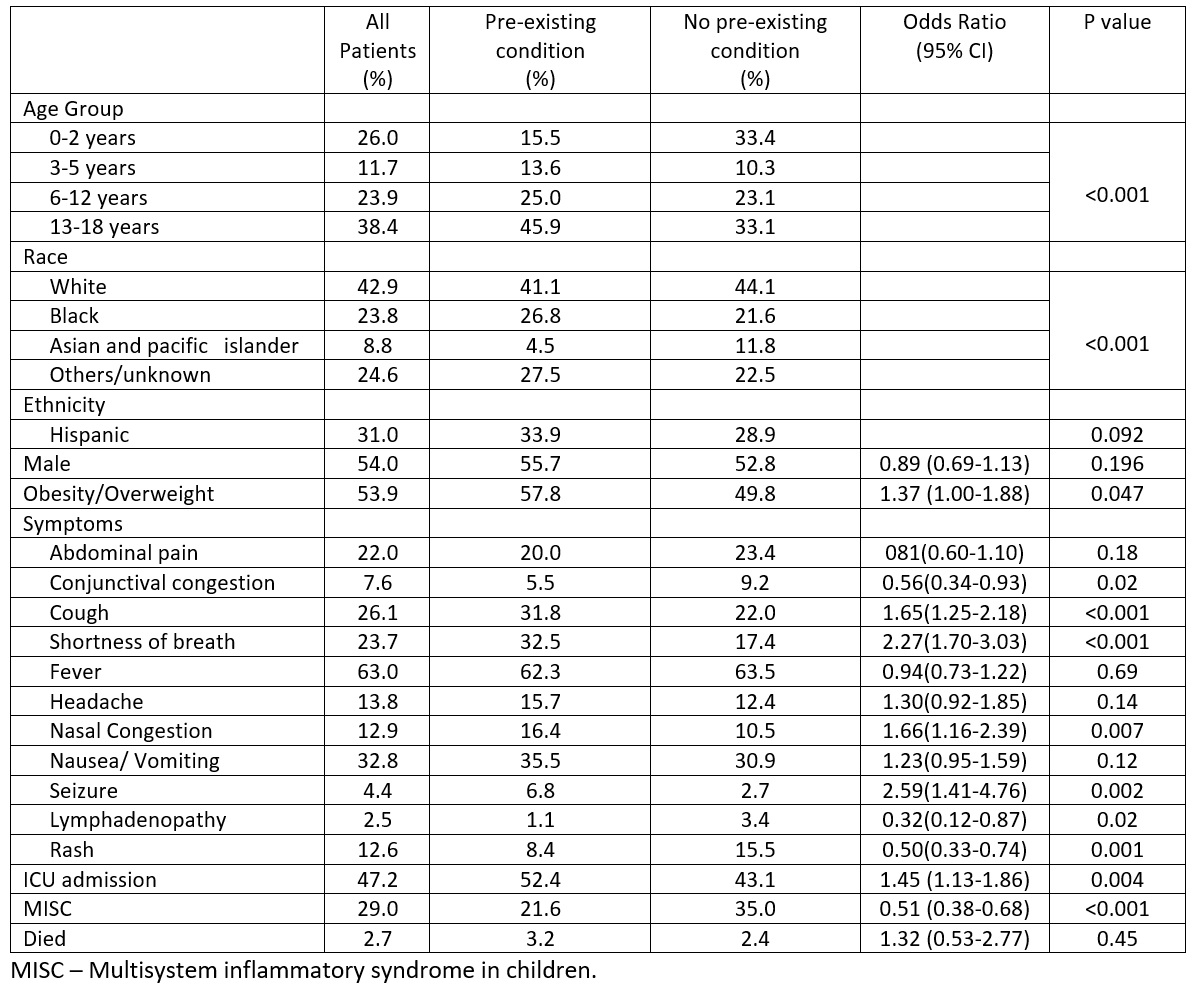
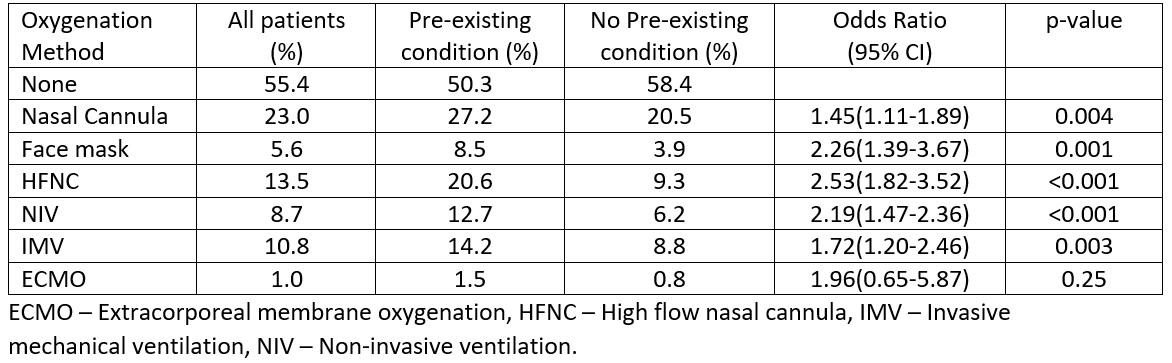
Table 2. Oxygenation methods in children with pre-existing condition and with no pre-existing condition and COVID-19 infection.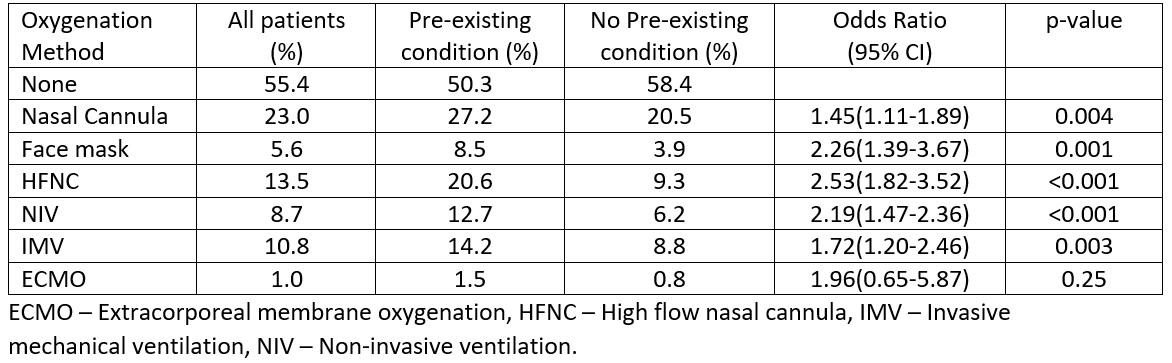
Objective: The study aimed to compare hospital course, resource utilization, and outcomes in children with and without pre-existing conditions and COVID-19 infection.
Design/Methods: A retrospective analysis using the Viral Infection and Respiratory illness Universal Study (VIRUS) COVID-19 registry from the Society of Critical Care Medicine was performed. Hospitalized children from age 0 to 18 years with COVID-19 infection from 51 centers were included. Categorical variables were analyzed using the chi-square test, continuous variables were compared with the Mann-Whitney U test and binomial data are presented as odds ratios with 95% CI. A P-value less than 0.05 was considered statistically significant. SPSS was used for statistical analysis.
Results: Among 1059 patients included in the analysis, 440 (41.5%) children had an underlying pre-existing condition. The demographic differences between the two groups are presented in Table 1. Children with the pre-existing condition were more likely to present with cough (31.8 Vs.22.0), dyspnea (32.5% Vs. 17.4%), and seizures (6.8% Vs 2.7%, Table 1). Multisystem inflammatory syndrome (MISC) was less commonly observed in children with pre-existing conditions (21.6% Vs 35.0%, OR=0.51, 95% CI: 0.38-0.68). Children with pre-existing conditions were more often admitted to the PICU (52.4% vs 43.1%, OR=1.45, 95% CI: 1.13-1.86), required high flow nasal cannula (20.6% Vs 9.3%), noninvasive mechanical ventilation (12.7% Vs 6.2%), and invasive mechanical ventilation (14.2% Vs 8.8%, Table 2) and had a longer duration of oxygen support (Table 3). The rates of inotrope use, CPR, and mortality were similar in the two groups. The hospital LOS was higher in patients with pre-existing conditions (median = 14.3 Vs 7.5 days, p = 0.004).Conclusion(s): Our multicenter study demonstrates that children with pre-existing conditions and COVID-19 infection are less likely to present with MISC and more often require respiratory support and have a longer length of stay. Our study adds to the knowledge of COVID-19 infection in the vulnerable population of children with pre-existing conditions.
Table 1. Demographic characteristics and presenting signs and symptoms of children with pre-existing condition and children with no pre-existing condition and COVID-19 infection.
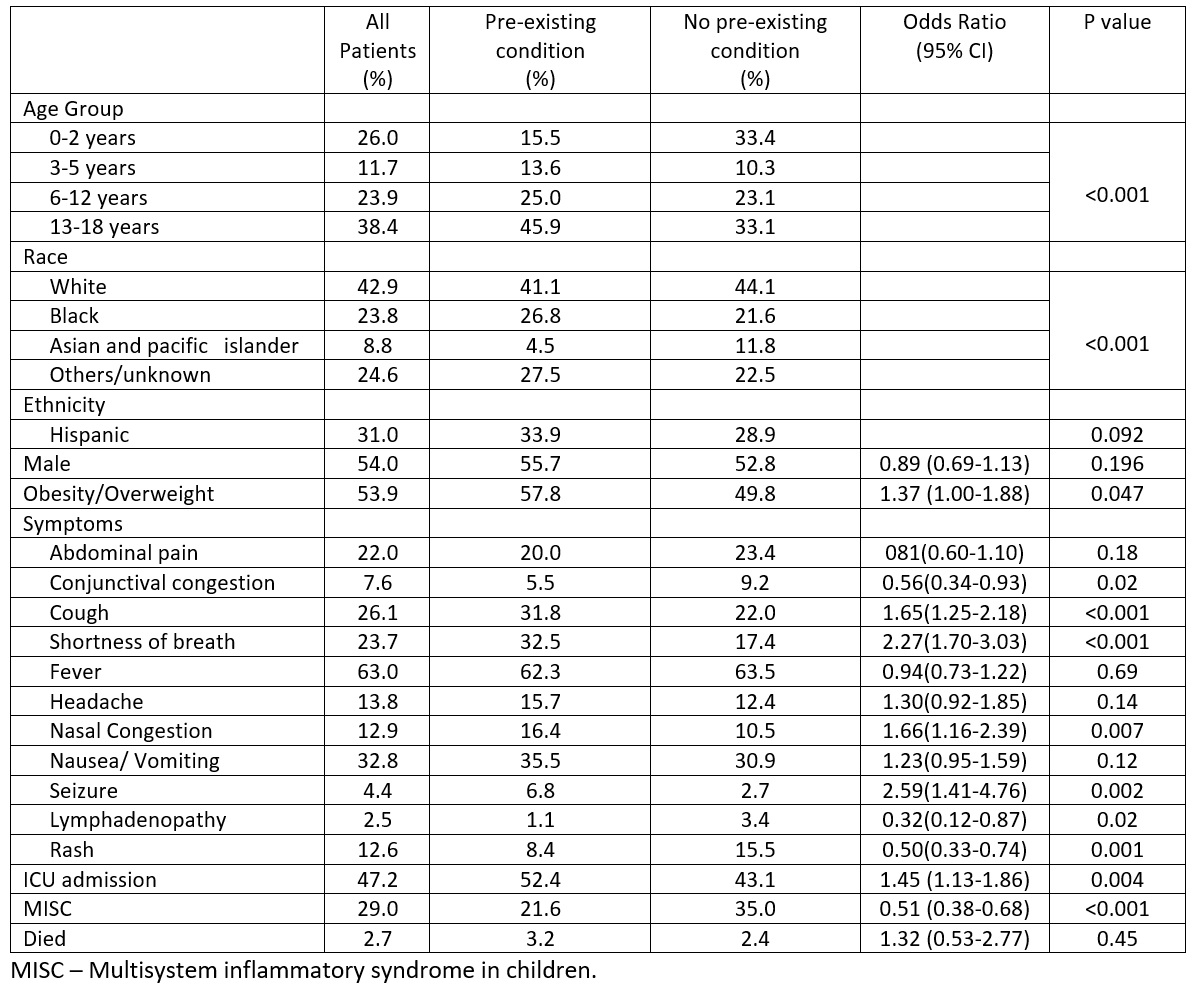
Table 2. Oxygenation methods in children with pre-existing condition and with no pre-existing condition and COVID-19 infection.