Neonatal Fetal Nutrition & Metabolism
Category: Abstract Submission
Neonatal Fetal Nutrition & Metabolism I
275 - Impact of maternal diabetes on early weight loss and other health outcomes in moderate preterm infants in the neonatal intensive care unit
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 275
Publication Number: 275.119
Publication Number: 275.119
Catherine O. Buck, Yale School of Medicine, Guilford, CT, United States; Veronika Shabanova, Yale School of Medicine, New Haven, CT, United States; Reese H. Clark, MEDNAX, Myrtle Beach, SC, United States; Sarah N. Taylor, Yale School of Medicine, New Haven, CT, United States
.jpg)
Catherine O. Buck, MD (she/her/hers)
Assistant Professor of Pediatrics
Yale School of Medicine
Guilford, Connecticut, United States
Presenting Author(s)
Background: Diabetes in pregnancy is associated with adverse maternal and infant health outcomes, including preterm birth. Neonatal morbidities are higher in infants born moderately preterm compared with infants born at term. It is unknown how diabetes in pregnancy affects health outcomes in moderate preterm infants.
Objective: To examine the influence of diabetes in pregnancy on short term neonatal morbidities and early growth trajectories in moderate preterm infants.
Design/Methods: This is a retrospective study from the MEDNAX Clinical Data Warehouse of moderate preterm infants (32 0/7 to 36 6/7 weeks gestational age [GA]) discharged from neonatal intensive care units (NICU) 2008-2019. Infants who died, had major congenital anomalies or were discharged after 40 weeks post-menstrual age were excluded. Maternal and infant health characteristics and average percent weight loss were compared between maternal diabetes (DM) exposure groups. Change in growth parameters (weight, length, weight change per day) during the delivery hospitalization were compared between groups using linear mixed effects modeling.
Results: Of the 301,499 moderate preterm infants included in the analysis, 14% (N = 42,512) were born to mothers with DM in pregnancy (DM group). DM-group had higher incidence of hypoglycemia (33% vs 17%), hyperbilirubinemia (68% vs 65%), patent ductus arteriosus (5% vs 3%), and need for some respiratory support (56% vs 54%) than non-DM infants (Table 1). DM-group had faster weight loss in the first postnatal week when stratified by GA at birth (Table 2). The adjusted difference in weight (g/day) from days 0 to 3 was -7.2 (95% CI: -8.2, -6.2), -6.5 (95% CI: -7.4, -5.7), and -4.5 (95% CI: -5.1, -3.9) for infants born 36-, 35-, and 34-weeks GA, respectively. Patterns of weight change from birth weight also differed by GA and DM-group status, such that 36-week DM-group infants remained on average 2% (± 0.4) below birth weight on day 14, while 32-week DM-group infants were on average 2% (± 0.4) above birth weight on day 14 (Figure 1). Differences in other growth parameters from birth to hospital discharge were statistically significant, but small in magnitude (Table 2).Conclusion(s): In this large study of moderate preterm infants, diabetes in pregnancy was associated with common neonatal morbidities, including need for respiratory support in the first postnatal days. Weight loss patterns in the first postnatal weeks among infants with exposure to diabetes differed by gestational age at birth and could be related to feeding maturity and early nutritional management.
Figure 1. Percent weight change from birthweight among moderate preterm infants by exposure to diabetes in pregnancy and birth gestational age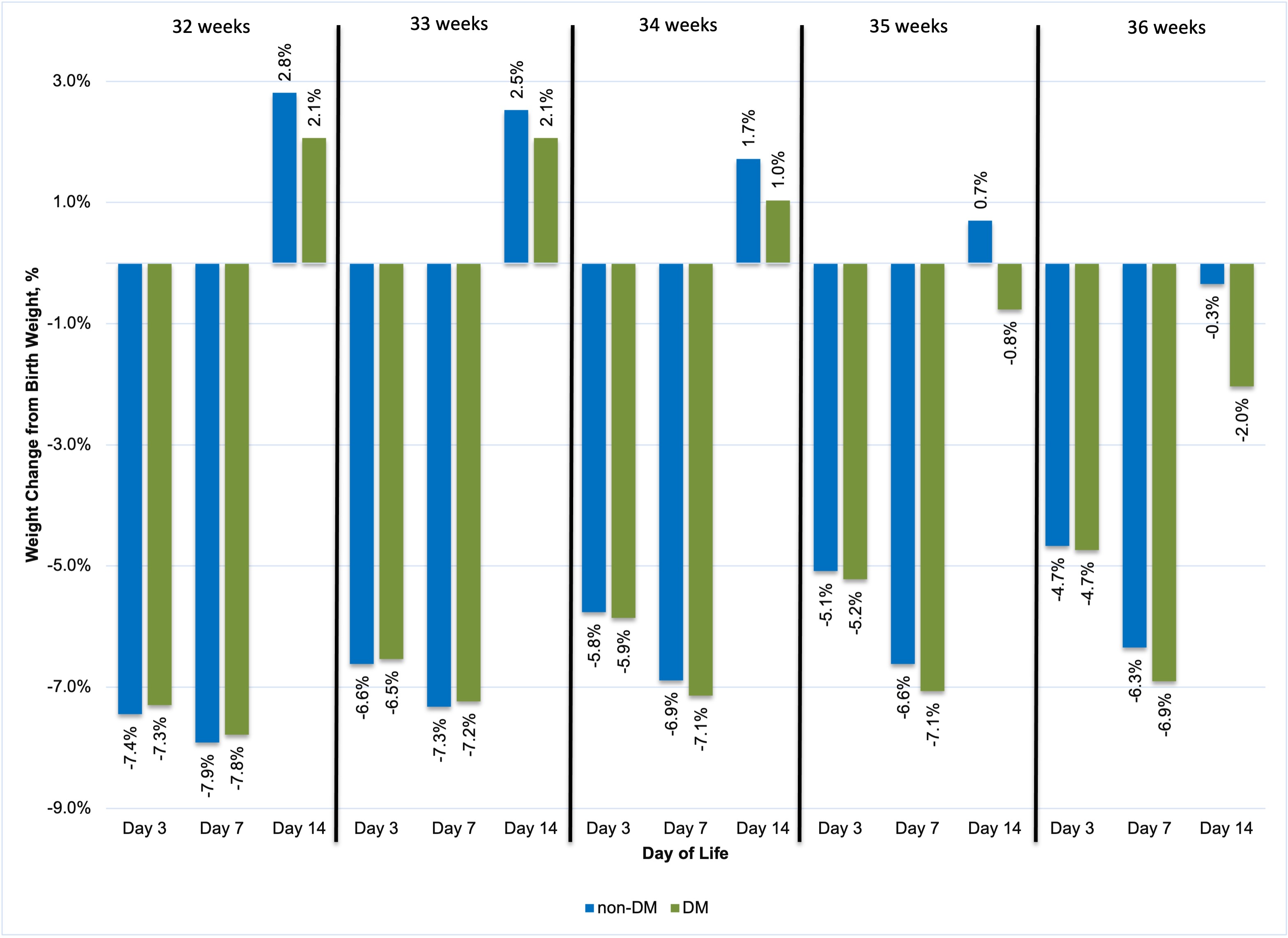 Legend: DM (diabetes group); non-DM (non-diabetes group)
Legend: DM (diabetes group); non-DM (non-diabetes group)
Table 1. Maternal and infant characteristics of the study sample by exposure to diabetes in pregnancyTable 1.jpegLegend:
Abbreviations: DM (diabetes mellitus)
Data are presented as N (%) and Median (25th – 75th percentile), unless otherwise indicated
*Chi square test for categorical variables or Wilcoxon Rank Sum test for continuous variables
1: Maternal hypertensive disorders: Gestational hypertension, chronic hypertension, pre-eclampsia and/or eclampsia
2: Need for respiratory support between birth and 3 days. Non-invasive support indicates need for oxygen, high flow nasal cannula, and/or non-invasive positive pressure ventilation. Invasive ventilation indicates need for high frequency ventilation or conventional ventilation by endotracheal intubation
3: Grade 2 or 3 necrotizing enterocolitis
Objective: To examine the influence of diabetes in pregnancy on short term neonatal morbidities and early growth trajectories in moderate preterm infants.
Design/Methods: This is a retrospective study from the MEDNAX Clinical Data Warehouse of moderate preterm infants (32 0/7 to 36 6/7 weeks gestational age [GA]) discharged from neonatal intensive care units (NICU) 2008-2019. Infants who died, had major congenital anomalies or were discharged after 40 weeks post-menstrual age were excluded. Maternal and infant health characteristics and average percent weight loss were compared between maternal diabetes (DM) exposure groups. Change in growth parameters (weight, length, weight change per day) during the delivery hospitalization were compared between groups using linear mixed effects modeling.
Results: Of the 301,499 moderate preterm infants included in the analysis, 14% (N = 42,512) were born to mothers with DM in pregnancy (DM group). DM-group had higher incidence of hypoglycemia (33% vs 17%), hyperbilirubinemia (68% vs 65%), patent ductus arteriosus (5% vs 3%), and need for some respiratory support (56% vs 54%) than non-DM infants (Table 1). DM-group had faster weight loss in the first postnatal week when stratified by GA at birth (Table 2). The adjusted difference in weight (g/day) from days 0 to 3 was -7.2 (95% CI: -8.2, -6.2), -6.5 (95% CI: -7.4, -5.7), and -4.5 (95% CI: -5.1, -3.9) for infants born 36-, 35-, and 34-weeks GA, respectively. Patterns of weight change from birth weight also differed by GA and DM-group status, such that 36-week DM-group infants remained on average 2% (± 0.4) below birth weight on day 14, while 32-week DM-group infants were on average 2% (± 0.4) above birth weight on day 14 (Figure 1). Differences in other growth parameters from birth to hospital discharge were statistically significant, but small in magnitude (Table 2).Conclusion(s): In this large study of moderate preterm infants, diabetes in pregnancy was associated with common neonatal morbidities, including need for respiratory support in the first postnatal days. Weight loss patterns in the first postnatal weeks among infants with exposure to diabetes differed by gestational age at birth and could be related to feeding maturity and early nutritional management.
Figure 1. Percent weight change from birthweight among moderate preterm infants by exposure to diabetes in pregnancy and birth gestational age
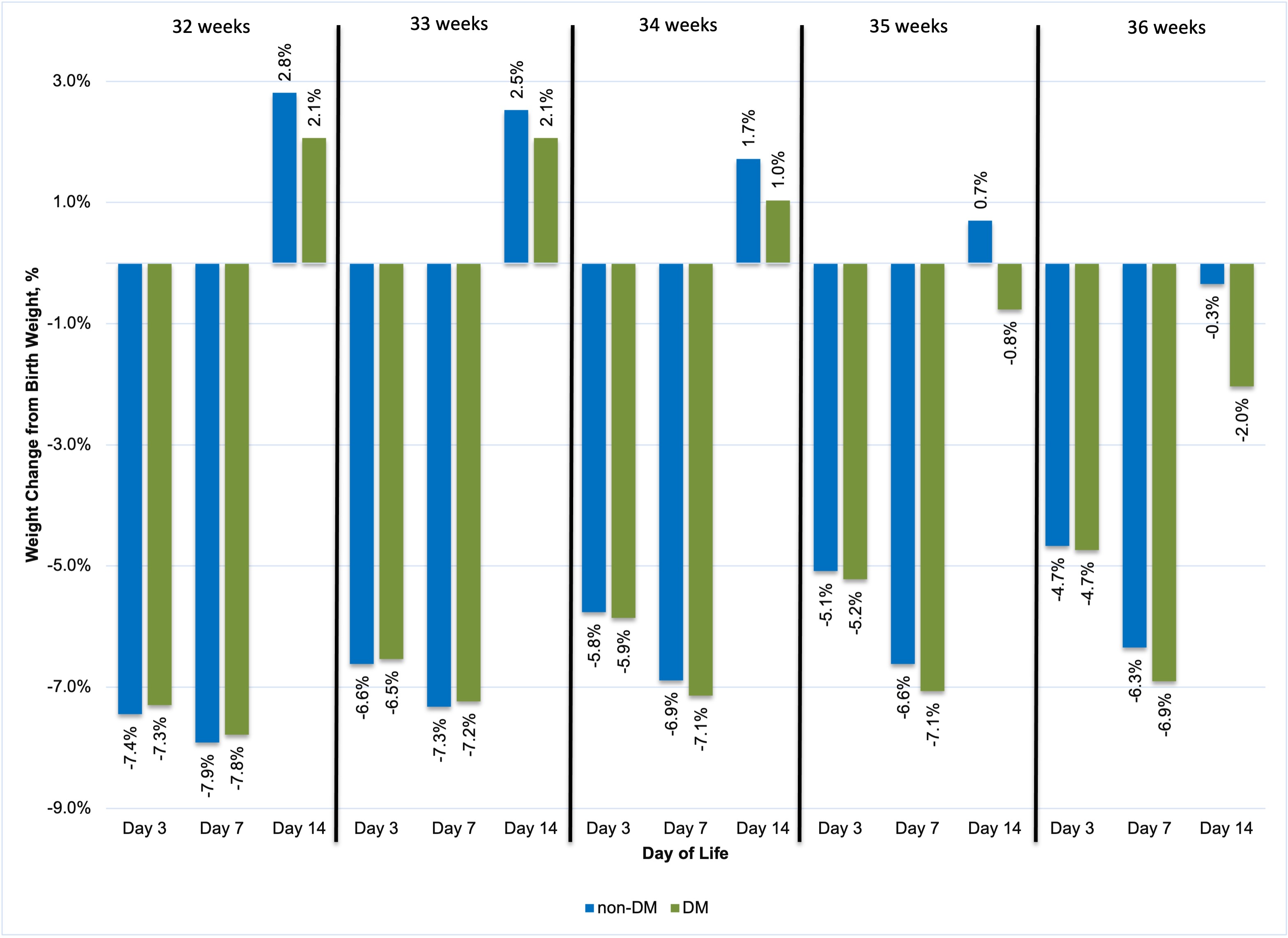 Legend: DM (diabetes group); non-DM (non-diabetes group)
Legend: DM (diabetes group); non-DM (non-diabetes group)Table 1. Maternal and infant characteristics of the study sample by exposure to diabetes in pregnancyTable 1.jpegLegend:
Abbreviations: DM (diabetes mellitus)
Data are presented as N (%) and Median (25th – 75th percentile), unless otherwise indicated
*Chi square test for categorical variables or Wilcoxon Rank Sum test for continuous variables
1: Maternal hypertensive disorders: Gestational hypertension, chronic hypertension, pre-eclampsia and/or eclampsia
2: Need for respiratory support between birth and 3 days. Non-invasive support indicates need for oxygen, high flow nasal cannula, and/or non-invasive positive pressure ventilation. Invasive ventilation indicates need for high frequency ventilation or conventional ventilation by endotracheal intubation
3: Grade 2 or 3 necrotizing enterocolitis
