Back
Critical Care
Category: Abstract Submission
3: Critical Care I
21 - Cardiac Recovery in Children Admitted to the Pediatric Intensive Care Unit with Multisystem Inflammatory Syndrome in Children
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 21
Publication Number: 21.102
Publication Number: 21.102
Zelda Ghersin, Hackensack Meridian Health, Neptune City, NJ, United States; Andrew Corson, K. Hovnanian Children's Hospital at Jersey Shore University Medical Center, Neptune, NJ, United States; Sara Galeotti, K. Hovnanian Children's Hospital at Jersey Shore University Medical Center, Ocean, NJ, United States; Stephanie Chin, K. Hovnanian Children's Hospital at Jersey Shore University Medical Center, Brick, NJ, United States; Hannah Kim, Joseph M. Sanzari Children's Hospital Hackensack University Medical Center, Hackensack, NJ, United States; saranga Agarwal, Pediatric intensive care , Hackensack University Medical Center, Hackensack, NJ, United States

Andrew Corson, MD
Pediatric Resident
K. Hovnanian Children's Hospital at Jersey Shore University Medical Center
Neptune, New Jersey, United States
Presenting Author(s)
Background: Multi-System Inflammatory Syndrome in Children (MIS-C) is a post-acute infection dysregulated inflammatory response that occurs four to six weeks after SARS-CoV-2 infection. Up to 80% of patients hospitalized with MIS-C develop cardiac complications. Due to low incidence of disease and limited data, there is no clear consensus on predictors of cardiac recovery or the cardiac outcomes in patients with MIS-C.
Objective: To evaluate the short and midterm cardiac outcomes in children hospitalized with MIS-C in two pediatric intensive care units (PICU) in New Jersey.
Design/Methods: We conducted a retrospective review of children admitted to the PICU with a diagnosis of MIS-C between April 2020 through March 2021. Cardiac biomarkers and echocardiograms performed during hospitalization were analyzed. Follow-up echocardiograms were performed two to eight weeks post-discharge, with interval follow-up of up to one year. Shortening fraction (SF) was used to assess left ventricular systolic function using standard M-mode (SF < 28% considered abnormal).
Results: Twenty-seven patients (18 male; median age 11 years) were included. The mean peak Troponin I in 25 patients was 2.10 +/- 5.0 ng/dL, and mean peak NT-ProBNP level in 26 patients was 1,606 +/- 1293 pg/dL. Most patients had normalization of cardiac biomarkers by time of discharge (Table 1). Seven of the 23 patients who had an echocardiogram on admission had a SF less than 28%. Lowest SF and SF at the time of discharge were compared in 21 patients with a median improvement of 6% (p < 0.001) (Table 2). Nineteen patients had a follow-up echocardiogram two to ten weeks post discharge and 18 of those had normal left ventricular systolic function (p < 0.001). No patient had evidence of diastolic dysfunction at follow-up. Eight patients had midterm follow-up five to seven months post-discharge, and one patient was followed for one-year post-discharge. Abnormalities that persist in these patients include low normal left ventricular systolic function. Three subjects had evidence of left coronary artery dilation (z score >2) during hospitalization and continued to have diffuse dilation at follow-up; with one developing right coronary artery dilation.Conclusion(s): In this cohort of patients, most children admitted to the PICU with MIS-C had abnormal cardiac biomarkers with normal to mildly decreased left ventricular systolic function that improved by time of discharge and continued to improve with midterm (5-7 months) follow-up. A very small subset of patients, however, continue to have cardiac complications including diffuse coronary artery dilation.
Table 1.png)
Results: Cardiac Biomarkers
Table 2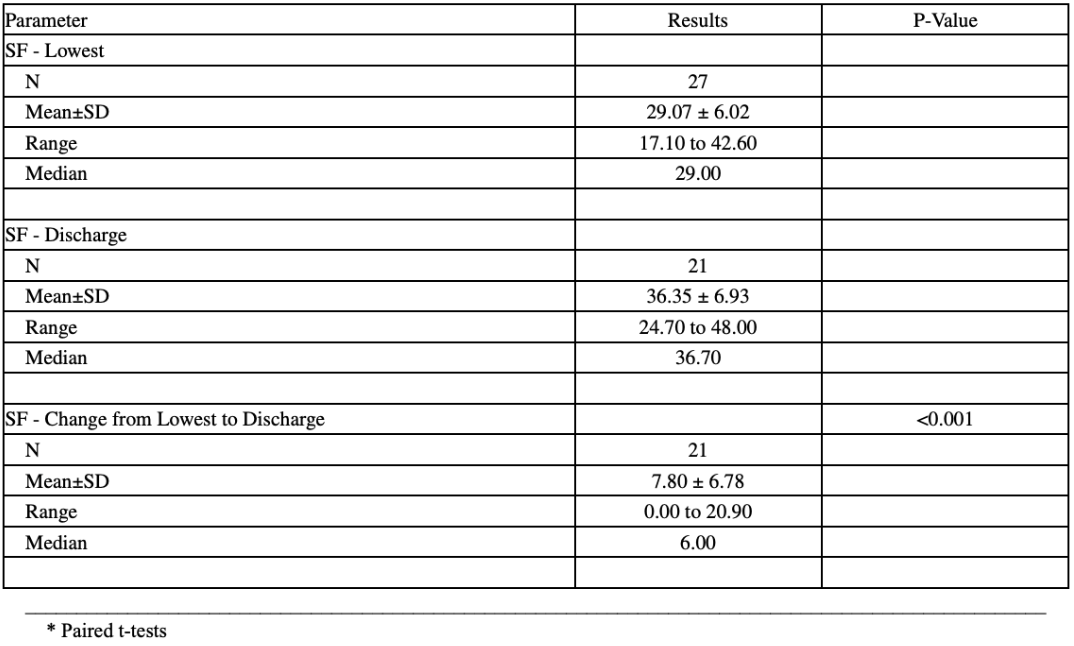
Results: Shortening Fraction by Echocardiography
Objective: To evaluate the short and midterm cardiac outcomes in children hospitalized with MIS-C in two pediatric intensive care units (PICU) in New Jersey.
Design/Methods: We conducted a retrospective review of children admitted to the PICU with a diagnosis of MIS-C between April 2020 through March 2021. Cardiac biomarkers and echocardiograms performed during hospitalization were analyzed. Follow-up echocardiograms were performed two to eight weeks post-discharge, with interval follow-up of up to one year. Shortening fraction (SF) was used to assess left ventricular systolic function using standard M-mode (SF < 28% considered abnormal).
Results: Twenty-seven patients (18 male; median age 11 years) were included. The mean peak Troponin I in 25 patients was 2.10 +/- 5.0 ng/dL, and mean peak NT-ProBNP level in 26 patients was 1,606 +/- 1293 pg/dL. Most patients had normalization of cardiac biomarkers by time of discharge (Table 1). Seven of the 23 patients who had an echocardiogram on admission had a SF less than 28%. Lowest SF and SF at the time of discharge were compared in 21 patients with a median improvement of 6% (p < 0.001) (Table 2). Nineteen patients had a follow-up echocardiogram two to ten weeks post discharge and 18 of those had normal left ventricular systolic function (p < 0.001). No patient had evidence of diastolic dysfunction at follow-up. Eight patients had midterm follow-up five to seven months post-discharge, and one patient was followed for one-year post-discharge. Abnormalities that persist in these patients include low normal left ventricular systolic function. Three subjects had evidence of left coronary artery dilation (z score >2) during hospitalization and continued to have diffuse dilation at follow-up; with one developing right coronary artery dilation.Conclusion(s): In this cohort of patients, most children admitted to the PICU with MIS-C had abnormal cardiac biomarkers with normal to mildly decreased left ventricular systolic function that improved by time of discharge and continued to improve with midterm (5-7 months) follow-up. A very small subset of patients, however, continue to have cardiac complications including diffuse coronary artery dilation.
Table 1
.png)
Results: Cardiac Biomarkers
Table 2
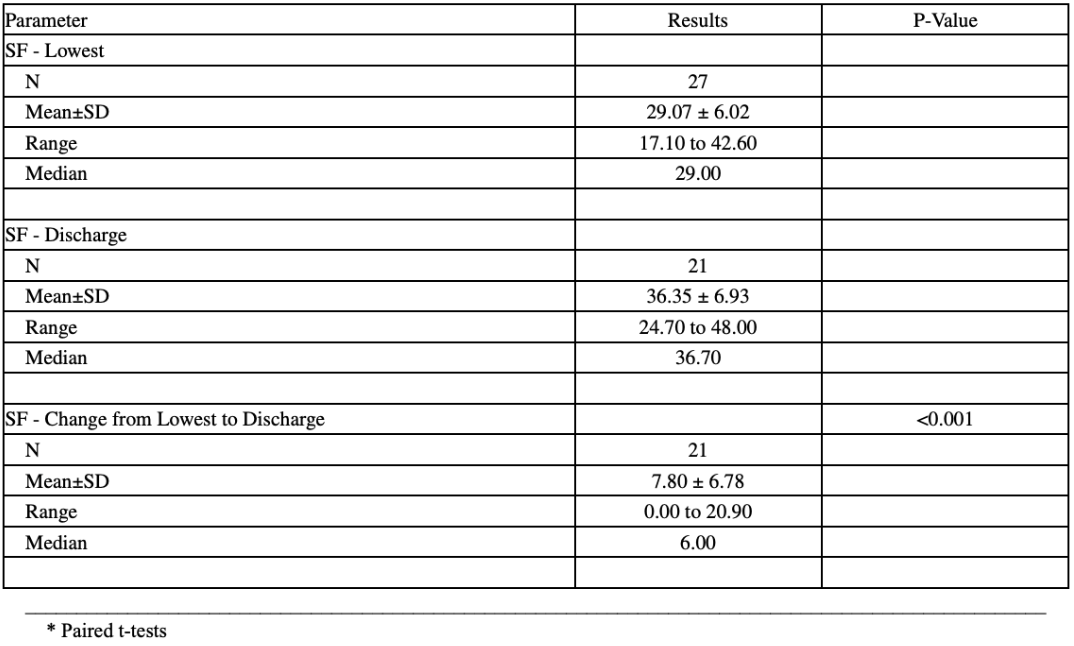
Results: Shortening Fraction by Echocardiography
