Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement VI
409 - The Do’s and Don’t(s) of Xray Positioning: Quality and Safety Initiatives aimed at reducing unnecessary radiation exposure and improving Xray quality in a level IV NICU in NE Florida
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 409
Publication Number: 409.436
Publication Number: 409.436
Emily Delaney, University of Florida College of Medicine, Jacksonville, FL, United States; Sfurti Nath, University of Florida College of Medicine, Jacksonville, FL, United States

Emily Delaney, PA-C
Physician Assistant in the NICU
University of Florida College of Medicine in Jacksonville, FL
Jacksonville, Florida, United States
Presenting Author(s)
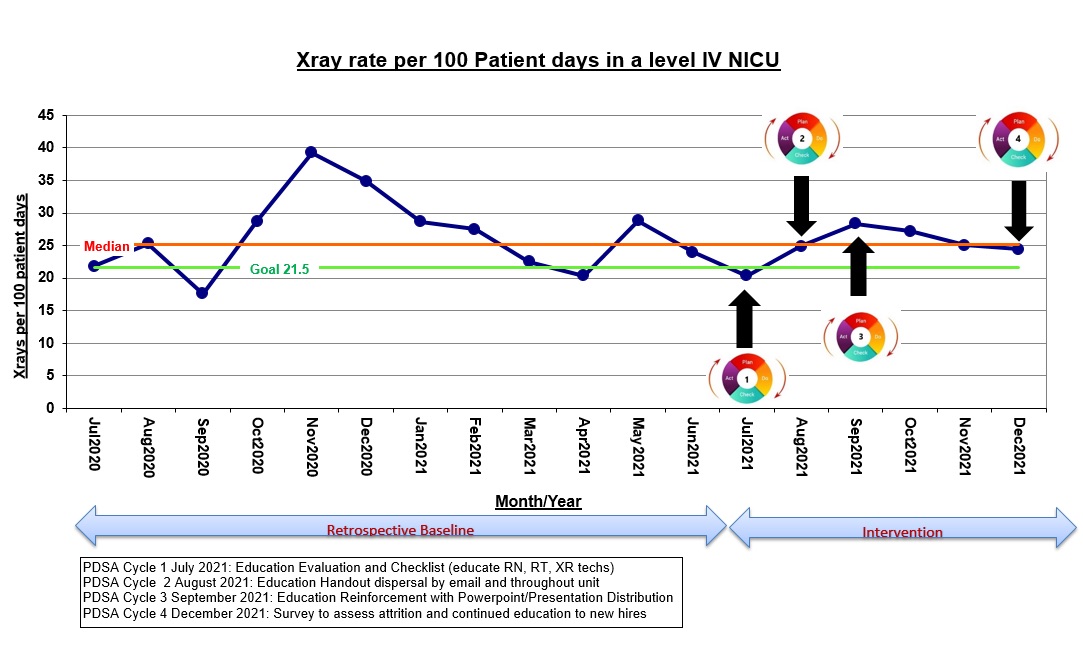
Background: Radiographs continue to be the cornerstone for formulating diagnoses and management in neonatal intensive care units (NICU). However, the ease of obtaining radiographs has impacted the quantity and impeded the quality of films. Poor technique, patient positioning, or artifacts obscuring areas of clinical interest lead to unnecessary repeat imaging and excessive radiation exposure in this vulnerable population.
Objective: The primary goal was to develop a structured approach involving the education of the interdisciplinary NICU team on proper X-ray (XR) holding to reduce the overall XR’s by 20% from baseline over a period of 1 year.
Design/Methods: This quality improvement project was performed between July 2020 and December 2021 after retrospective evaluation of baseline data. The 1st PDSA cycle was directed to nurses, nursing residents, respiratory therapists (RT) and x-ray (XR) technicians with bedside education using a poster visual aid with immediate feedback on clinical scenarios and hands-on manikin demos. Cycle 2 involved posting a pre-XR checklist at every bedside, educational handout distribution via email and print outs placed at all nursing stations. An educational powerpoint (ppt) was emailed after a month as part of the 3rd PDSA cycle. The attrition rates were evaluated as survey responses in the 4th PDSA cycle.
Results: PDSA cycles 1 through 3 involved 100% education for the NICU team with subsequent evaluation of case scenarios, manikin demos, and distributed educational handouts and ppt presentation by email. 4th PDSA cycle involved assessment of attrition rates via a survey and continued education. Survey response rate was 50%. 65% of respondents felt extremely confident in correctly positioning infants with 100% correct identification of basic steps for good quality imaging. While response rate was high for endotracheal tube and arm PICC positioning (85%; 89%), fewer correct responses were received for lower limb PICC (64%). >85% identified at least two mistakes in suboptimal XR. Identification of critical NICU conditions were variable ranging from 78% to 89% (esophageal atresia; congenital diaphragmatic hernia). 32% correctly responded to applied learning case scenarios evaluating analysis and deduction. Conclusion(s): Structured approach through education, safety checklists, continued audits and attritional evaluation are effective practices in improving safety and quality of XR in the NICU leading to reduction in number of XR and improving imaging quality. There is a need for frequent surveillance and identification of best practices for continued performance improvement.
Xray Frequency per 100 patients from July 2020 to December 2021.jpg)
Xray rate per 100 Patient Days in a level IV NICU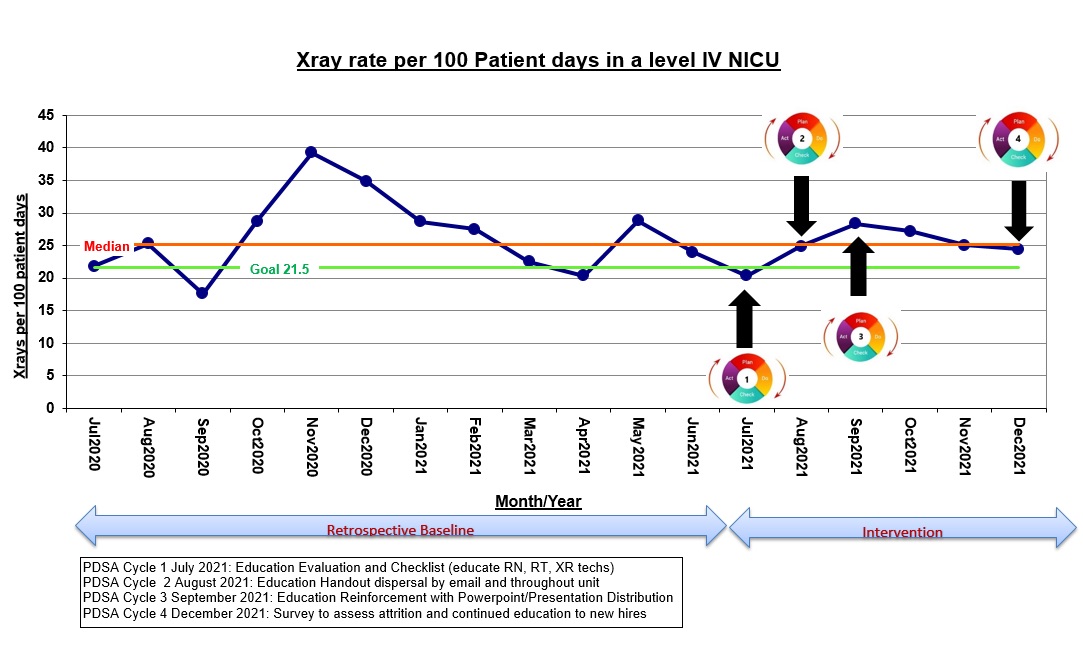
Objective: The primary goal was to develop a structured approach involving the education of the interdisciplinary NICU team on proper X-ray (XR) holding to reduce the overall XR’s by 20% from baseline over a period of 1 year.
Design/Methods: This quality improvement project was performed between July 2020 and December 2021 after retrospective evaluation of baseline data. The 1st PDSA cycle was directed to nurses, nursing residents, respiratory therapists (RT) and x-ray (XR) technicians with bedside education using a poster visual aid with immediate feedback on clinical scenarios and hands-on manikin demos. Cycle 2 involved posting a pre-XR checklist at every bedside, educational handout distribution via email and print outs placed at all nursing stations. An educational powerpoint (ppt) was emailed after a month as part of the 3rd PDSA cycle. The attrition rates were evaluated as survey responses in the 4th PDSA cycle.
Results: PDSA cycles 1 through 3 involved 100% education for the NICU team with subsequent evaluation of case scenarios, manikin demos, and distributed educational handouts and ppt presentation by email. 4th PDSA cycle involved assessment of attrition rates via a survey and continued education. Survey response rate was 50%. 65% of respondents felt extremely confident in correctly positioning infants with 100% correct identification of basic steps for good quality imaging. While response rate was high for endotracheal tube and arm PICC positioning (85%; 89%), fewer correct responses were received for lower limb PICC (64%). >85% identified at least two mistakes in suboptimal XR. Identification of critical NICU conditions were variable ranging from 78% to 89% (esophageal atresia; congenital diaphragmatic hernia). 32% correctly responded to applied learning case scenarios evaluating analysis and deduction. Conclusion(s): Structured approach through education, safety checklists, continued audits and attritional evaluation are effective practices in improving safety and quality of XR in the NICU leading to reduction in number of XR and improving imaging quality. There is a need for frequent surveillance and identification of best practices for continued performance improvement.
Xray Frequency per 100 patients from July 2020 to December 2021
.jpg)
Xray rate per 100 Patient Days in a level IV NICU