Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 7: Neonatal Neurology Term Imaging
356 - The predictive value of MRI scoring systems for neurodevelopmental outcome in infants with hypoxic ischemic encephalopathy
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 356
Publication Number: 356.443
Publication Number: 356.443
Csilla Andorka, Semmelweis University, Budapest, Budapest, Hungary; Tímea Seszták, Semmelweis University, Budapest, Budapest, Hungary; Ludovika Dunai, Semmelweis University, Budapest, Budapest, Hungary; Agnes Jermendy, Semmelweis University, Budapest, Budapest, Hungary; Miklós Szabó, Division of Neonatology Ist Dept. of Pediatrics Semmelweis University, Budapest, Budapest, Hungary; Enikő Szakmár, Semmelweis University, Budapest, Budapest, Hungary

Eniko Szakmar, MD, PhD
Pediatric Resident
Semmelweis University
Budapest, Hungary
Presenting Author(s)
Background: Several MRI scoring systems are used to quantify brain injury in infants with hypoxic-ischemic encephalopathy (HIE). The Barkovich score system relies on conventional MRI sequences to assess injury in the basal ganglia, thalamus and watershed areas. Recently, Weeke et al. has developed a scoring system assessing brain injury of grey matter, white matter, cortex and cerebellum including diffusion weighted images (DWI) and proton magnetic resonance spectroscopy (H-MRS). Both scoring systems have been shown to predict adverse outcomes at 2 years of age.
Objective: Our objective was to compare the predictive value of two MRI scoring systems for adverse outcome (severe disabilities or death) in infants receiving hypothermia for HIE.
Design/Methods: This single center retrospective cohort study included infants who received hypothermia for HIE between 2013 and 2019. Post-rewarming brain MRI images were evaluated according to the two MRI scoring systems developed by Barkovich (total score 9) and Weeke et al. (total score 55). Follow-up was performed using Bayley- II Scales of Infant Development at 18-24 months of age. Adverse outcome was defined as death or severe disabilities if Bayley II score was < 70 in any domain. Receiver Operating Characteristics (ROC) curve was used to calculate area under the curve (AUC), with the DeLong- test for comparison of AUCs.
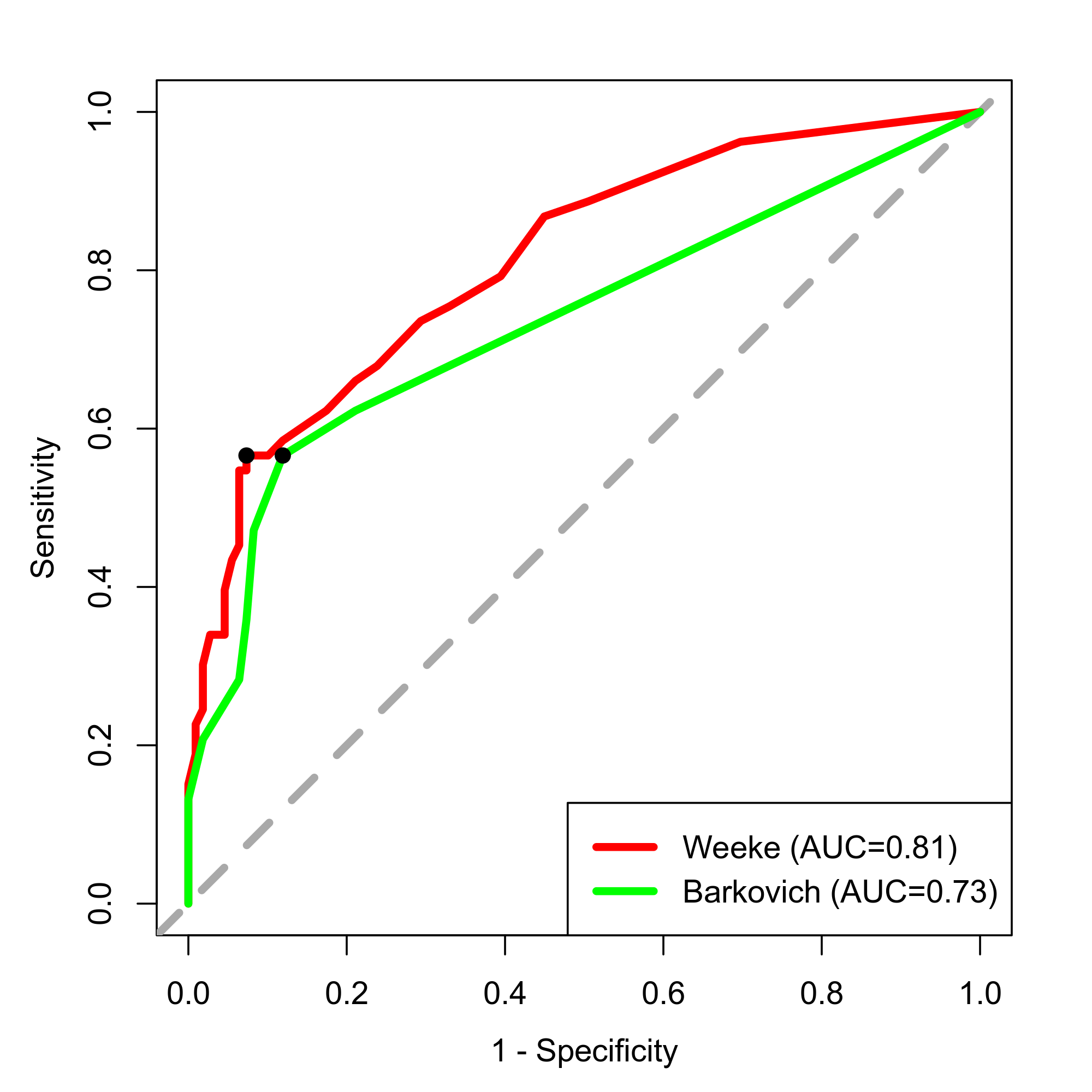
Results: A total of 163 infants were included. The rate of death was 5.6% and severe disabilities occurred in 27.3% (44/162) of the cases. MRI studies were carried out at a median 4.7 days of life [IQR 3.5; 6.2]. Brain injury was detected with higher frequency using Weeke score compared to Barkovich (71% vs. 35%, p<0.001). The median total score of Weeke was 4 [IQR 1; 11], whereas median score of Barkovich was 0 [IQR 0; 2]. The area under the ROC curve was 0.81 [95%CI 0.74; 0.88] with the optimal cutoff point of 12 (Sensitivity 57%, Specificity 93%) for adverse outcome using the Weeke score. The AUC was 0.73 [95%CI 0.66; 0.81] with the optimal cutoff point of 2 (Sensitivity 57%, Specificity 88%) based on the Barkovich score. DeLong- test showed a significant difference between the two AUCs (p= 0.0012) (Figure 1).Conclusion(s): Our findings confirm that a more detailed scoring system incorporating DWI and H-MRS has a better predictive value for adverse outcome in infants with HIE. MRI can serve as a bridging biomarker and a surrogate end point for neurodevelopmental outcome, so it is crucial to quantify brain injuries based on standardized scoring systems.
Receiver operating characteristic curves for adverse outcome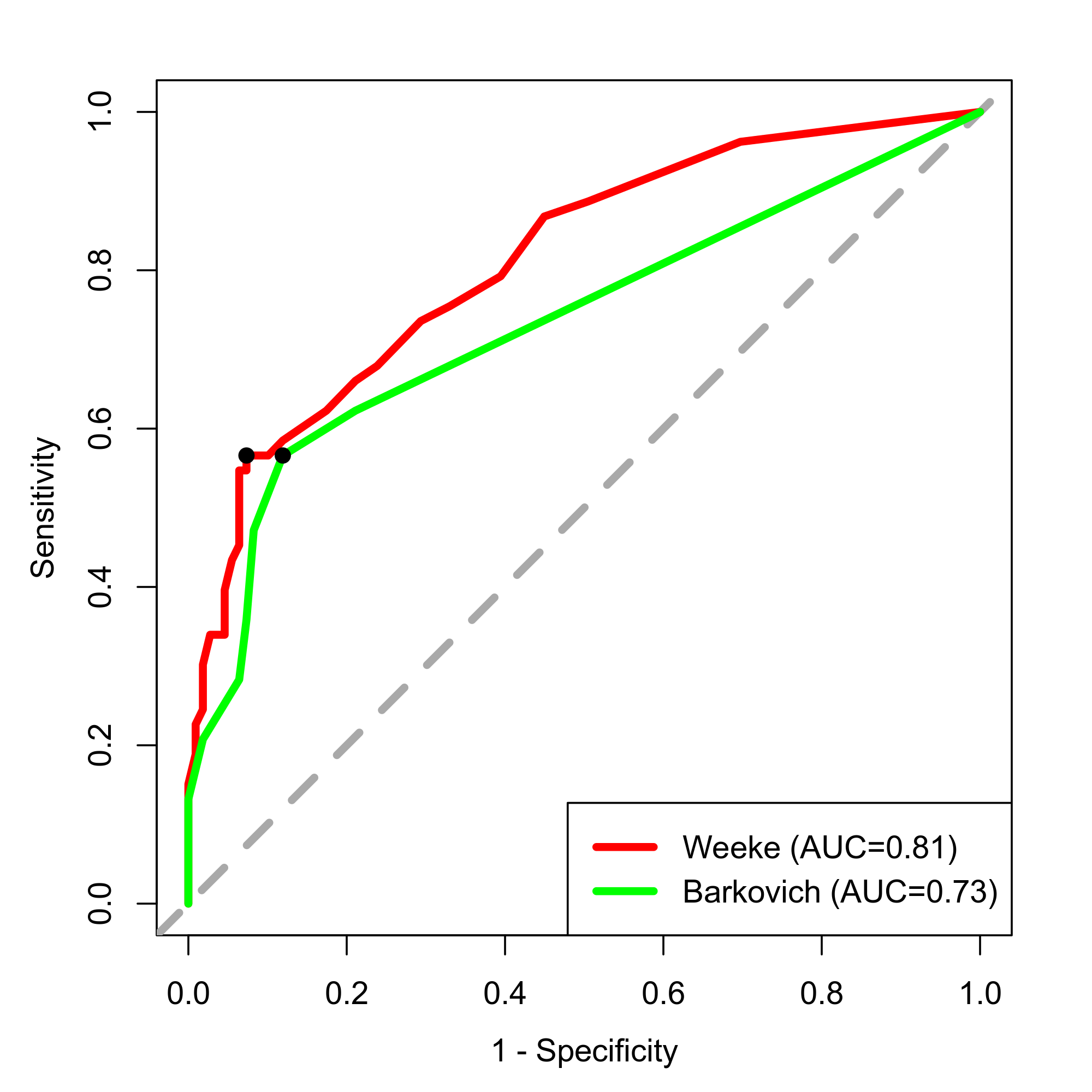
Objective: Our objective was to compare the predictive value of two MRI scoring systems for adverse outcome (severe disabilities or death) in infants receiving hypothermia for HIE.
Design/Methods: This single center retrospective cohort study included infants who received hypothermia for HIE between 2013 and 2019. Post-rewarming brain MRI images were evaluated according to the two MRI scoring systems developed by Barkovich (total score 9) and Weeke et al. (total score 55). Follow-up was performed using Bayley- II Scales of Infant Development at 18-24 months of age. Adverse outcome was defined as death or severe disabilities if Bayley II score was < 70 in any domain. Receiver Operating Characteristics (ROC) curve was used to calculate area under the curve (AUC), with the DeLong- test for comparison of AUCs.
Results: A total of 163 infants were included. The rate of death was 5.6% and severe disabilities occurred in 27.3% (44/162) of the cases. MRI studies were carried out at a median 4.7 days of life [IQR 3.5; 6.2]. Brain injury was detected with higher frequency using Weeke score compared to Barkovich (71% vs. 35%, p<0.001). The median total score of Weeke was 4 [IQR 1; 11], whereas median score of Barkovich was 0 [IQR 0; 2]. The area under the ROC curve was 0.81 [95%CI 0.74; 0.88] with the optimal cutoff point of 12 (Sensitivity 57%, Specificity 93%) for adverse outcome using the Weeke score. The AUC was 0.73 [95%CI 0.66; 0.81] with the optimal cutoff point of 2 (Sensitivity 57%, Specificity 88%) based on the Barkovich score. DeLong- test showed a significant difference between the two AUCs (p= 0.0012) (Figure 1).Conclusion(s): Our findings confirm that a more detailed scoring system incorporating DWI and H-MRS has a better predictive value for adverse outcome in infants with HIE. MRI can serve as a bridging biomarker and a surrogate end point for neurodevelopmental outcome, so it is crucial to quantify brain injuries based on standardized scoring systems.
Receiver operating characteristic curves for adverse outcome