Medical Education: Resident
Category: Abstract Submission
Medical Education 13 - Medical Education: Resident IV
267 - Use of Practice Based Learning Modules to Teach Primary Care Preventative Measures in Pediatric Residency
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 267
Publication Number: 267.419
Publication Number: 267.419
Veronica S. Wang, University of Maryland Children's Hospital, Fulton, MD, United States; Rebecca G. Carter, University of Maryland School of Medicine, Baltimore, MD, United States; Katelyn Donohue, University of Maryland School of Medicine, Baltimore, MD, United States; Emily A. Wisniewski, University of Maryland Children's Hospital, Baltimore, MD, United States; Monica Mehta, University of Maryland School of Medicine, Prince Frederick, MD, United States

Rebecca Carter, MD (she/her/hers)
Assistant Professor
University of Maryland School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Identifying age-appropriate developmental milestones, vaccine schedules, and preventive screenings is a critical cornerstone of Pediatric residency training, and ultimately primary care practice. A prior study performed by our residents demonstrated that the implementation of practice based learning modules (PBLs) improved residents’ comfort with routine and special vaccine schedules, as well as routine lab screenings. However, the sample size was small and the data collection period was short.
Objective: The aim of this study was to extend the understanding of knowledge and comfort level of these topics at health supervision visits before and after participating in the PBLs, and their influence on the annual Pediatric In-Training Exam (ITE) scores.
Design/Methods: Pediatric residents participated in PBLs during their continuity clinics, utilizing modules to guide their practice and reflect on their ability to assess developmental milestones, vaccine schedules, and preventive care screenings. ITE data, including the total score and Preventive Care/Well Child sub-score (PC/WC), was analyzed to determine changes pre- and post-PBL implementation. In addition, residents completed pre- and post-intervention surveys to assess comfort with preventive care components.
Results: There was a statistically significant increase in overall ITE scores pre- and post-PBL implementation (n=45, p < 0.0001), but this did not extend to overall scores when comparing across training levels. When comparing PC/WC sub-scores within training levels pre- and post-PBL, there was a statistically significant improvement (p < 0.001, p=0.011). Survey analysis demonstrated improvement in residents’ comfort in their ability to identify age-appropriate developmental milestones (n=9, p=0.0081).Conclusion(s): Pre- and post-intervention analysis demonstrated improvement in the overall scores, as well as PC/WC sub-scores, suggesting that PBLs are an effective teaching tool for Pediatric primary care interventions. The post-PBL survey demonstrated improved resident comfort with developmental milestones but not with vaccine schedules or routine lab screenings, and the survey was limited by small sample size and inability to match pre- and post-data. Future studies should increase sample size of resident surveys and match ITE scores with survey data. Additionally, multi-institution data will reinforce the role of PBLs on ITE scores as well as resident comfort and understanding of preventive care measures.
CV for Veronica WangVeronica Wang CV.pdf
Table 2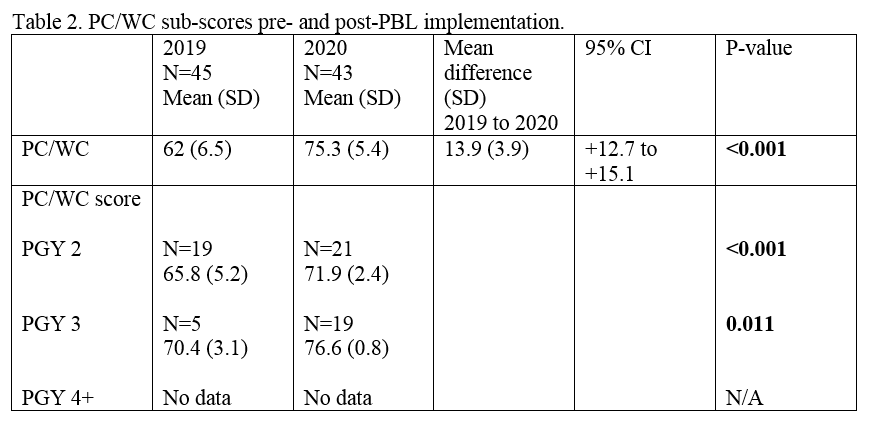 PC/WC sub-scores pre-and post-PBL implementation
PC/WC sub-scores pre-and post-PBL implementation
Objective: The aim of this study was to extend the understanding of knowledge and comfort level of these topics at health supervision visits before and after participating in the PBLs, and their influence on the annual Pediatric In-Training Exam (ITE) scores.
Design/Methods: Pediatric residents participated in PBLs during their continuity clinics, utilizing modules to guide their practice and reflect on their ability to assess developmental milestones, vaccine schedules, and preventive care screenings. ITE data, including the total score and Preventive Care/Well Child sub-score (PC/WC), was analyzed to determine changes pre- and post-PBL implementation. In addition, residents completed pre- and post-intervention surveys to assess comfort with preventive care components.
Results: There was a statistically significant increase in overall ITE scores pre- and post-PBL implementation (n=45, p < 0.0001), but this did not extend to overall scores when comparing across training levels. When comparing PC/WC sub-scores within training levels pre- and post-PBL, there was a statistically significant improvement (p < 0.001, p=0.011). Survey analysis demonstrated improvement in residents’ comfort in their ability to identify age-appropriate developmental milestones (n=9, p=0.0081).Conclusion(s): Pre- and post-intervention analysis demonstrated improvement in the overall scores, as well as PC/WC sub-scores, suggesting that PBLs are an effective teaching tool for Pediatric primary care interventions. The post-PBL survey demonstrated improved resident comfort with developmental milestones but not with vaccine schedules or routine lab screenings, and the survey was limited by small sample size and inability to match pre- and post-data. Future studies should increase sample size of resident surveys and match ITE scores with survey data. Additionally, multi-institution data will reinforce the role of PBLs on ITE scores as well as resident comfort and understanding of preventive care measures.
CV for Veronica WangVeronica Wang CV.pdf
Table 2
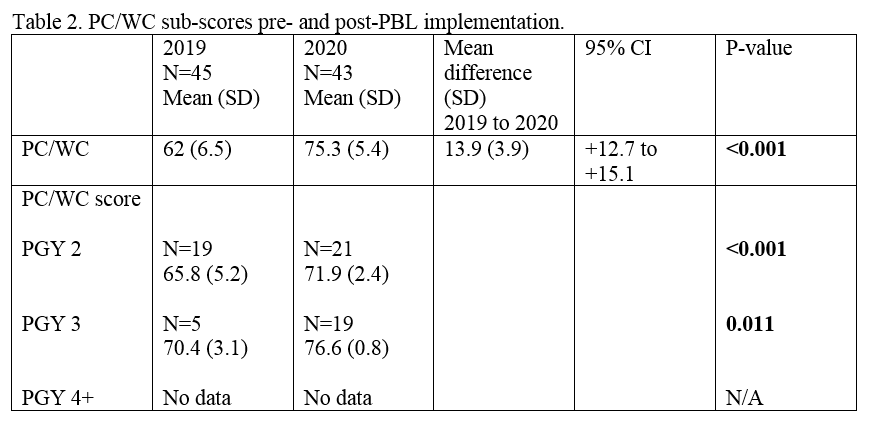 PC/WC sub-scores pre-and post-PBL implementation
PC/WC sub-scores pre-and post-PBL implementation