Back
Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Clinical - Bronchiolitis/HFNC and Newborn Care
136 - When to Transfer: Predictors of High Flow Nasal Cannula Failure in Pediatric Patients Presenting to a Community Hospital
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 136
Publication Number: 136.415
Publication Number: 136.415
Kimiko Dunbar, Children's Hospital Colorado, Denver, CO, United States; Jacob Thomas, University of Colorado School of Medicine, Aurora, CO, United States; Sarah Nodine, University of Colorado School of Medicine, Golden, CO, United States; Mark Brittan, Children's Hospital Colorado, Aurora, CO, United States; Jillian M. Cotter, University of Colorado School of Medicine, Aurora, CO, United States

Kimiko S. Dunbar, MD
Pediatric Hospital Medicine Fellow
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: High flow nasal cannula (HFNC) is commonly used for acute respiratory illness. Children who do not improve, known as HFNC failure, often require escalation to an intensive care unit (ICU). To safely implement HFNC in community hospitals without an ICU, it is important to identify patients at risk for failure, enabling early transfer before deterioration. Prior literature has identified partial pressure of carbon dioxide (pCO2) > 50mmHg as one variable that can predict failure. Less is known about other risk factors of HFNC failure or the impact of a pCO2-driven protocol in the community setting.
Objective: To determine factors associated with HFNC failure among children presenting to a community hospital.
Design/Methods: We performed a retrospective cohort study of patients < 18 years who received HFNC at a community hospital from 7/2018 to 10/2019. We excluded patients with medical complexity. Per protocol, a pC02 was obtained prior to HFNC initiation, patients were transferred to a quaternary-care hospital if pCO2>50mmHg or based on clinical discretion. Our outcome was HFNC failure, defined as need for HFNC greater than the floor limit per age per policy, non-invasive positive pressure, or mechanical ventilation. In bivariable analysis, we compare demographic and clinical factors (e.g. diagnosis, vital signs, pCO2) between those with and without HFNC failure. We included variables in a multivariable model based on clinical and statistical significance (p < 0.2). We used Poisson regression with robust error variance to calculate the adjusted relative risk (aRR) of HFNC failure for each variable in the model. Receiver operating characteristic (ROC) analysis was performed to compare the predictive power of pCO2 alone vs a full multivariable model (with and without pCO2).
Results: Of 74 patients receiving HFNC, 42 had HFNC failure (Table 1). In multivariable regression, the risk of failure was higher in those who were younger (aRR 0.91, p=0.001), and had asthma (aRR 1.68, p=0.009). Patients with an improved respiratory rate (RR) after HFNC initiation were less likely to fail (aRR 0.61, p=0.024; Figure 1). In ROC analysis, pCO2 was not an accurate predictor of failure; models with all variables from the multivariable analysis, with and without pCO2, showed significantly better prediction compared to pCO2 alone (p=0.006, p=0.009 respectively; Figure 2).Conclusion(s): Patients who were younger, had asthma, and did not have an improved RR after HFNC initiation were more likely to experience HFNC failure. These factors should be considered when triaging who can be safely receive HFNC in the community setting.
Kimiko Dunbar CVDunbar.Kimiko.CV.pdf
Figure 1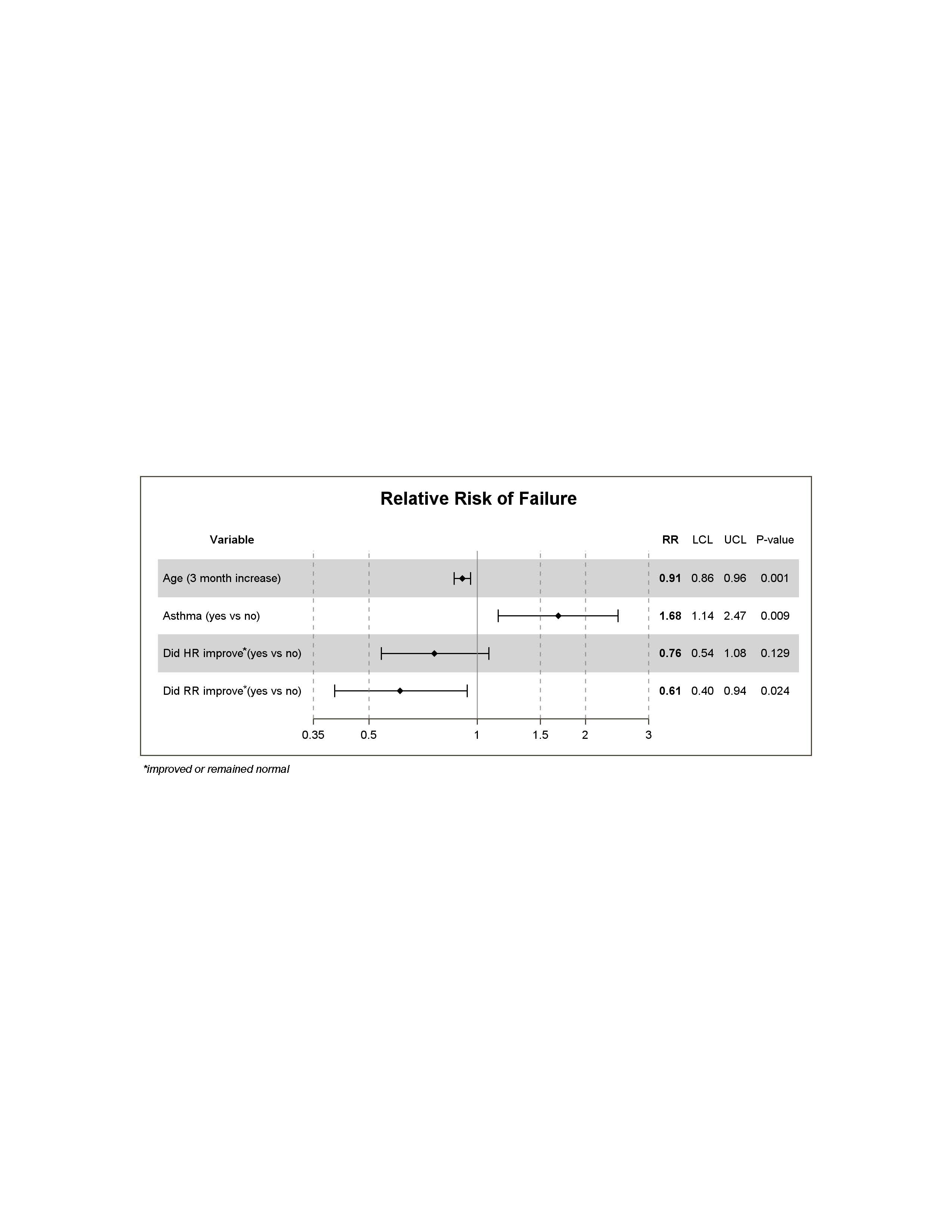 Relative Risk of Failure
Relative Risk of Failure
Objective: To determine factors associated with HFNC failure among children presenting to a community hospital.
Design/Methods: We performed a retrospective cohort study of patients < 18 years who received HFNC at a community hospital from 7/2018 to 10/2019. We excluded patients with medical complexity. Per protocol, a pC02 was obtained prior to HFNC initiation, patients were transferred to a quaternary-care hospital if pCO2>50mmHg or based on clinical discretion. Our outcome was HFNC failure, defined as need for HFNC greater than the floor limit per age per policy, non-invasive positive pressure, or mechanical ventilation. In bivariable analysis, we compare demographic and clinical factors (e.g. diagnosis, vital signs, pCO2) between those with and without HFNC failure. We included variables in a multivariable model based on clinical and statistical significance (p < 0.2). We used Poisson regression with robust error variance to calculate the adjusted relative risk (aRR) of HFNC failure for each variable in the model. Receiver operating characteristic (ROC) analysis was performed to compare the predictive power of pCO2 alone vs a full multivariable model (with and without pCO2).
Results: Of 74 patients receiving HFNC, 42 had HFNC failure (Table 1). In multivariable regression, the risk of failure was higher in those who were younger (aRR 0.91, p=0.001), and had asthma (aRR 1.68, p=0.009). Patients with an improved respiratory rate (RR) after HFNC initiation were less likely to fail (aRR 0.61, p=0.024; Figure 1). In ROC analysis, pCO2 was not an accurate predictor of failure; models with all variables from the multivariable analysis, with and without pCO2, showed significantly better prediction compared to pCO2 alone (p=0.006, p=0.009 respectively; Figure 2).Conclusion(s): Patients who were younger, had asthma, and did not have an improved RR after HFNC initiation were more likely to experience HFNC failure. These factors should be considered when triaging who can be safely receive HFNC in the community setting.
Kimiko Dunbar CVDunbar.Kimiko.CV.pdf
Figure 1
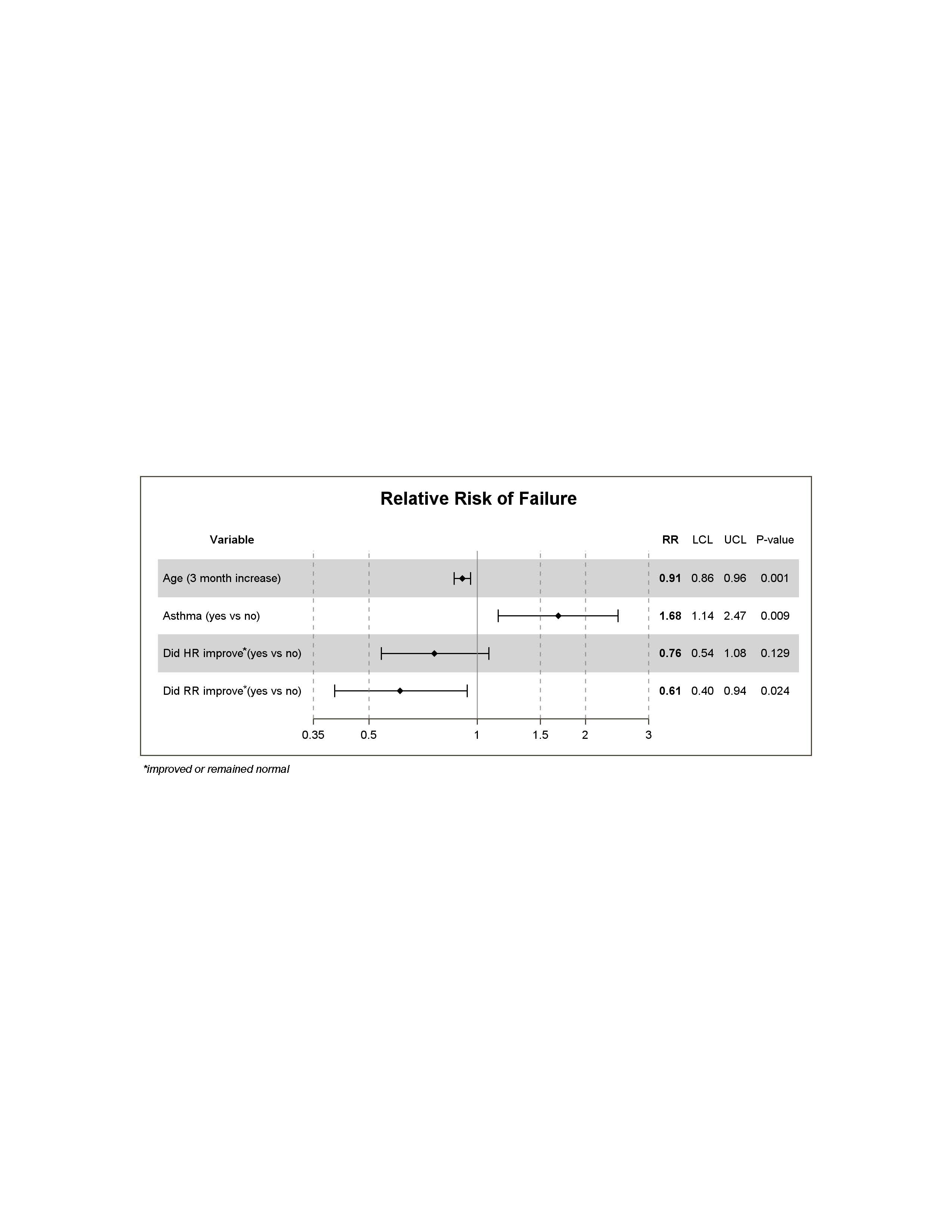 Relative Risk of Failure
Relative Risk of Failure